Paracoccidoiomycosis is a systemic mycosis with a higher incidence in males with history of exposure to the rural environment; its classic clinical manifestation is an oro-pulmonary lesion. The authors report a case of a female, urban, 76-year-old patient with atypical clinical-dermatological presentation and diagnostic conclusion after histopathological examination. The clinical response was quick and complete after treatment with itraconazole 400mg/day in the first month, decreased to 200mg/day until the sixth month of treatment.
Paracoccidioidomycosis is a systemic mycosis caused by dimorphic fungi of the genus Paracoccidioides (P. brasiliensis or P. lutzii),1 which, in the chronic clinical presentation in adults, mainly affects men (male/female ratio: up to 22/1) in the range from 30 to 59 years old.2 Lung and oral mucosa involvement is usual in this clinical form.
The authors report a case of a 76-year-old female patient with painful skin lesions two months prior to presentation. The patient denied trauma or fever; she had undergone treatment with antibiotics, without improvement. She reported type II diabetes mellitus and systemic arterial hypertension. The dermatological examination showed phagedenic ulcers, with necrotic areas, surrounded by an inflammatory halo (Figs. 1 and 2). The lesions were more exuberant in the deltoid regions, with satellite lesions on the shoulders and forearms. The supplemental clinical examination was normal, although the patient presented depression symptoms and was suffering from her illness.
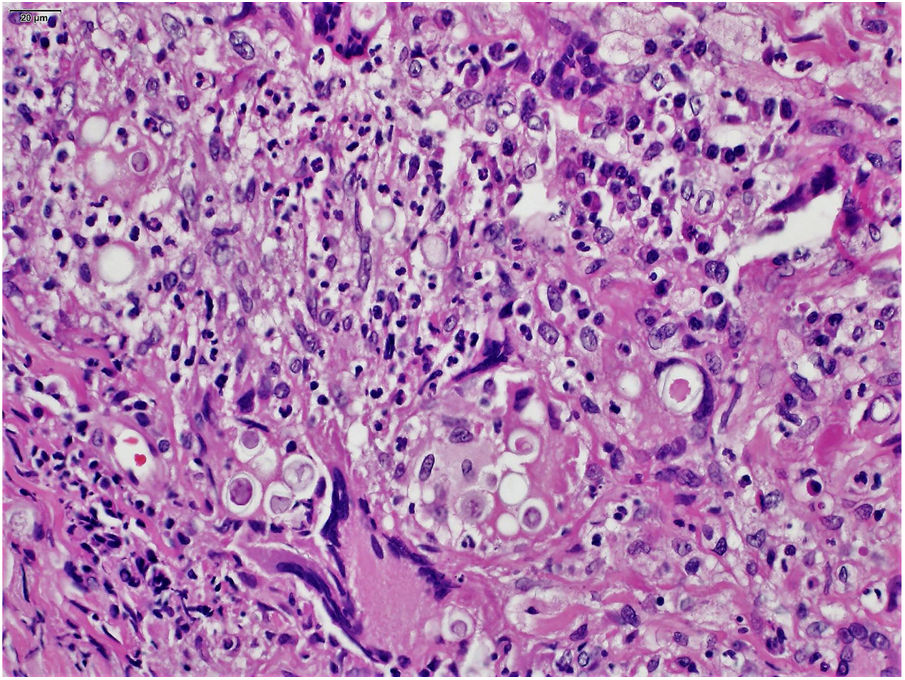
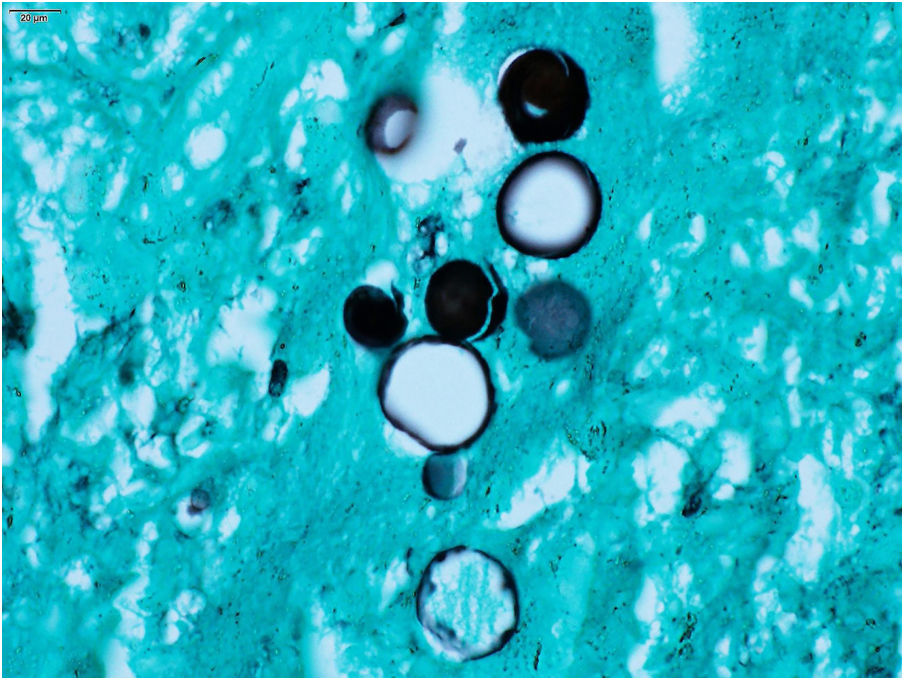
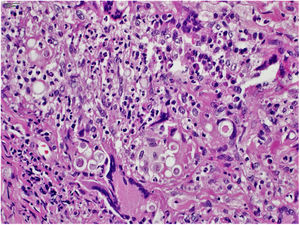
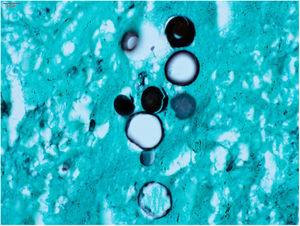
The clinical hypothesis was that of pyoderma gangrenosum, due to the presence of painful ulcers, of rapid growth and geographical aspect; however, no violet halo was observed and the edges were not undermined. Another hypothesis was primary cutaneous cryptococcosis, due to the inflammatory aspect associated with necrosis, localized in exposed areas; however, the bilateral aspect of the lesions did not correspond to this hypothesis. Biopsies and laboratory investigation were performed; the final diagnosis of paracoccidioidomycosis was surprising and confirmed by histopathological examination (Figs. 3 and 4) and direct mycological examination. Complementary tests, including chest and abdominal computed tomography (CT), ruled out involvement of other organs. Laboratory tests revealed elevated CRP and glycemia, negative HIV and anti-P. brasiliensis serology, and negative culture for bacteria and fungi. The clinical response was complete after treatment with itraconazole 400mg/day in the first month, decreased to 200mg/day until the sixth month of treatment.
The present case differs from the usual pattern of paracoccidioidomycosis in several aspects. The disease is uncommon in both female and elderly patients. As a rule, lung involvement is present in adult patients, being the source of metastatic spread of the infection to other organs.3 Pulmonary involvement was not observed in the present case, even using high-resolution CT.4 Nonetheless, the most unusual finding was the pattern of skin lesions. In paracoccidioidomycosis, skin lesions are observed in up to 62.1% of cases, usually on the face, such as acneiform lesions, in infiltrated plaques, or vegetating and simultaneously with multiple organ involvement, including the lungs.5 Ulcers with necrotic areas are uncommon, as the skin ulcers in paracoccidioidomycosis are generally shallow, granular, and usually with hemorrhagic spots, similar to what is observed in mucosal lesions; they are not phagedenic or painful.5
The patient's advanced age, immunosenescence, and diabetes probably contributed to the rapid evolution and atypical presentation in this case.6,7 Itraconazole has been considered as the first treatment option and is effective at a dose of 200mg/day for 9–18 months.8 In the present study, itraconazole was successfully used at 400mg/day in the first month with the aim of promoting quick resolution of injuries, improving quality of life, and reducing the psychological stress experienced by the patient.
Financial supportNone declared.
Authors’ contributionBruno Augusto Alvares: Approval of the final version of the manuscript; conception and planning of the study; intellectual participation in propaedeutic and/or therapeutic conduct of studied cases.
Cláudia Alves Lapa Gracia: Approval of the final version of the manuscript; intellectual participation in propaedeutic and/or therapeutic conduct of studied cases; critical review of the manuscript.
Mariangela Esther Alencar Marques: Approval of the final version of the manuscript; intellectual participation in propaedeutic and/or therapeutic conduct of studied cases; critical review of the manuscript.
Silvio Alencar Marques: Approval of the final version of the manuscript; conception and planning of the study; critical review of the manuscript.
Conflicts of interestNone declared.
How to cite this article: Alvares BA, Gracia CAL, Marques MEA, Marques SA. Paracoccidioidomycosis: an uncommon clinical presentation. An Bras Dermatol. 2020. https://doi.org/10.1016/j.abd.2020.06.001
Study conducted at the Department of Dermatology and Radiotherapy, Faculdade de Medicina, Universidade Estadual Paulista, Botucatu, SP, Brazil.