Lupus erythemathosus is a chronic, relapsing disease with acute, subacute, and chronic lesions. Effluvium telogen occurs in the setting of systemic activity of the disease, and cicatricial alopecia results from discoid lesionsin on the scalp. Other types of alopecia, like alopecia areata, may rarely be found in lupus. Frontal fibrosing alopecia is characterized by frontotemporal hairline recession and eybrow loss. Histophatologically, it cannot be differentiated from lichen planopilaris.It is controversial whether frontal fibrosing alopecia is a subtype of lichen planopilaris.. A pacient with chronic lichenoid lupus erythematosus is described with clinical, histophatological and dermoscopic features of frontal fibrosing alopecia.We have not been able to find in the literature cases of frontal fibrosing alopecia as a clinical manifestation of lupus.
Frontal fibrosing alopecia (FFA) is a typical pattern of scarring alopecia that affects the frontal hairline and is associated with loss of eyebrows and eyelashes, and visible changes of the vellus hair of the face. It can also lead to the development of minute papules on the frontotemporal region. It occurs mainly in postmenopausal women.1 On histopathology, a reduction in the number of follicles, with lymphocytic infiltrate and fibrosis can be seen, along with interface dermatitis on the follicular epithelium, indistinguishable from lichen planopilaris (LPP).2 In discoid lupus erythematosus (DLE), atrophy and permanent alopecia are late features, since in the early phases only erythema, adhered scales, and follicular plugs are observed. The differential diagnosis of scarring alopecias is clinically difficult, and histopathology and dermoscopy are necessary for diagnostic clarification.3,4
We describe the case of a patient with DLE since the age of 45 years, presenting as bilateral frontotemporal scarring alopecia, associated to rarefaction of the eyebrows. We discuss the relationship of FFA and lupus erythematosus: an overlap or an atypical presentation of lupus scarring alopecia.
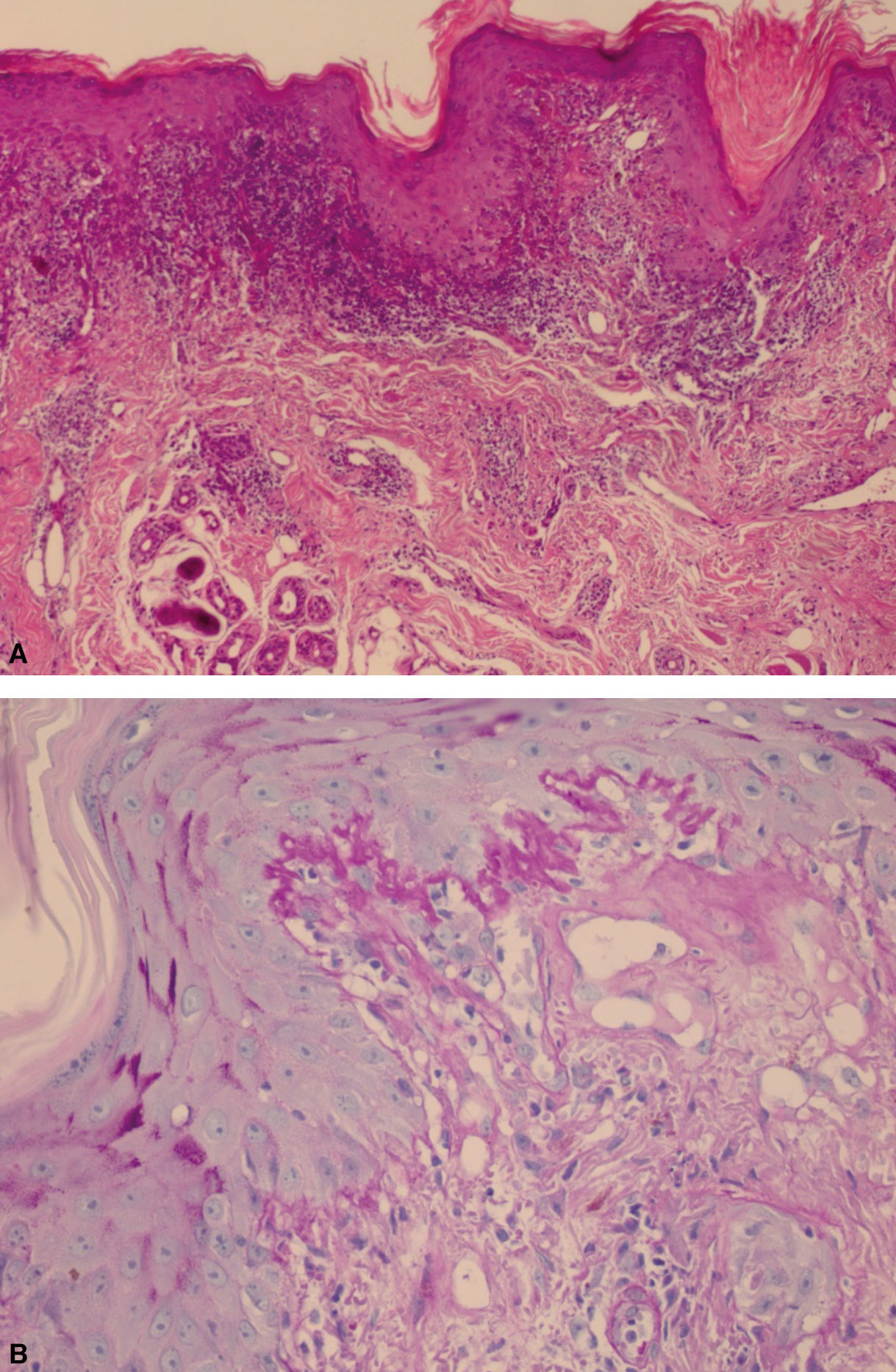
Case ReportA 58-year-old woman with a 13-year follow-up of chronic cutaneous lupus erythematosus presenting with photosensitivity and arthralgia, fine dotted nuclear pattern ANA (1:320), and no other immunological abnormalities. She had a past history of hypothyroidism, systemic hypertension, type-2 diabetes mellitus, and dyslipidemia. Initially, she presented with erythematous, tumid plaques on the nose and upper lip, with mild atrophy, and frontal alopecia with bilateral rarefaction of the eyebrows (Figure 1). Two biopsies from the facial lesions, in 2006 and 2010, showed changes consistent with lichenoid lupus erythematosus, with negative direct immunofluorescence (DIF), and a scalp biopsy in 2006 showed lichenoid perifolliculitis (Figure 2). From 2003 to 2010, she was treated with mometasone cream and minoxidil (2% solution), with no improvement. She was then started on hydroxychloroquine (400 mg daily). Still with no improvement, in 2014 methotrexate was added (15mg weekly), with good clinical response. In a few months, the clinical picture progressed with brown macules on the face and recurrence of the atrophic oval-shaped lesions with central erythema on the periocular, supralabial and nasal regions, along with absence of hair and perifollicular hyperkeratosis on the eyebrows, and no progression of the frontal alopecia. Methotrexate dose was increased to 17.5mg weekly, and hydroxychloroquine was maintained. Seven months later, the alopecia remained stable, and the cutaneous lesions had no activity. The patient was lost to follow- up for one year. With worsening of the alopecia, a dermoscopy examination was performed and revealed c features of FFA. A new biopsy confirmed the diagnosis (Figures 3 and 4).
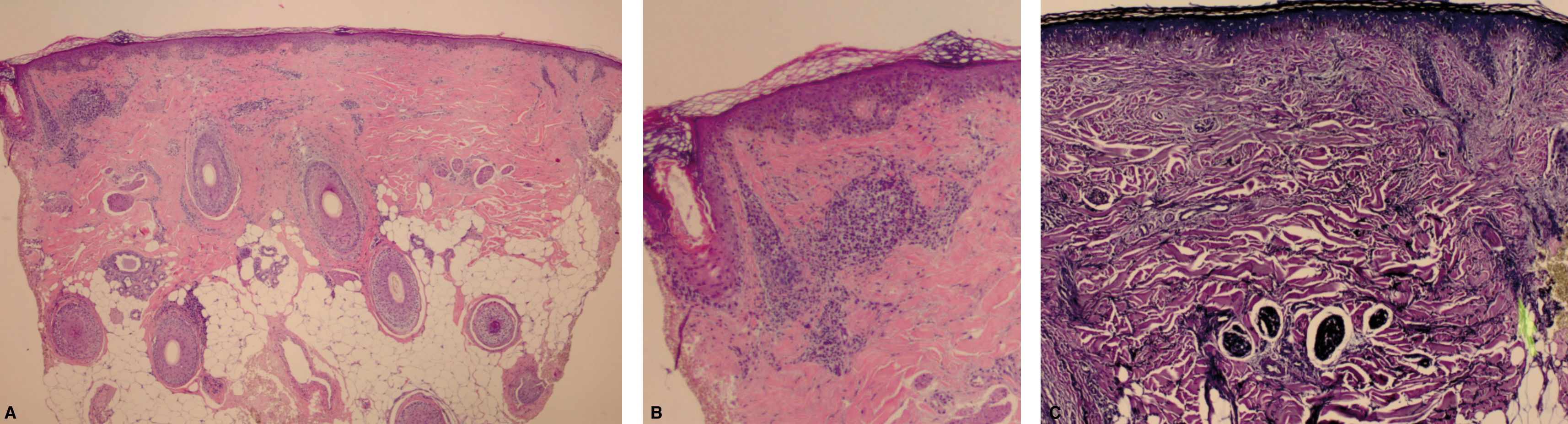
There are few reports of the association of FFA and DLE, and the clinical and histopathological distinction between both conditions can be difficult.5,6 The presence of cutaneous lesions on other parts of the body can help in the differential diagnosis. Classically, the histopathological aspects of FFA are the presence of lichenoid interface dermatitis in the upper portions of the follicle, especially in the peri-infundibular region and isthmus, with a predominantly lymphocytic infiltrate.7 These features were seen in our patient (Figure 4). On the other hand, in DLE, lymphocytic infiltrate is perifollicular, superficial and deep, and perivascular, with melanocytes in the upper dermis.
Scalp (frontoparietal region) A - Reduction in the number of hair follicles and replacement by fibrosis. B - Presence of a hair follicle with lymphocytic inflammatory infiltrate affecting the isthmus, suggetive of frontal fibrosing alopecia (Hematoxylin & eosin, X40). C - Evaluation of elastic fibers, architectural derangement where a hair follicle was previously located (arrow) (Verhoeff, X100)
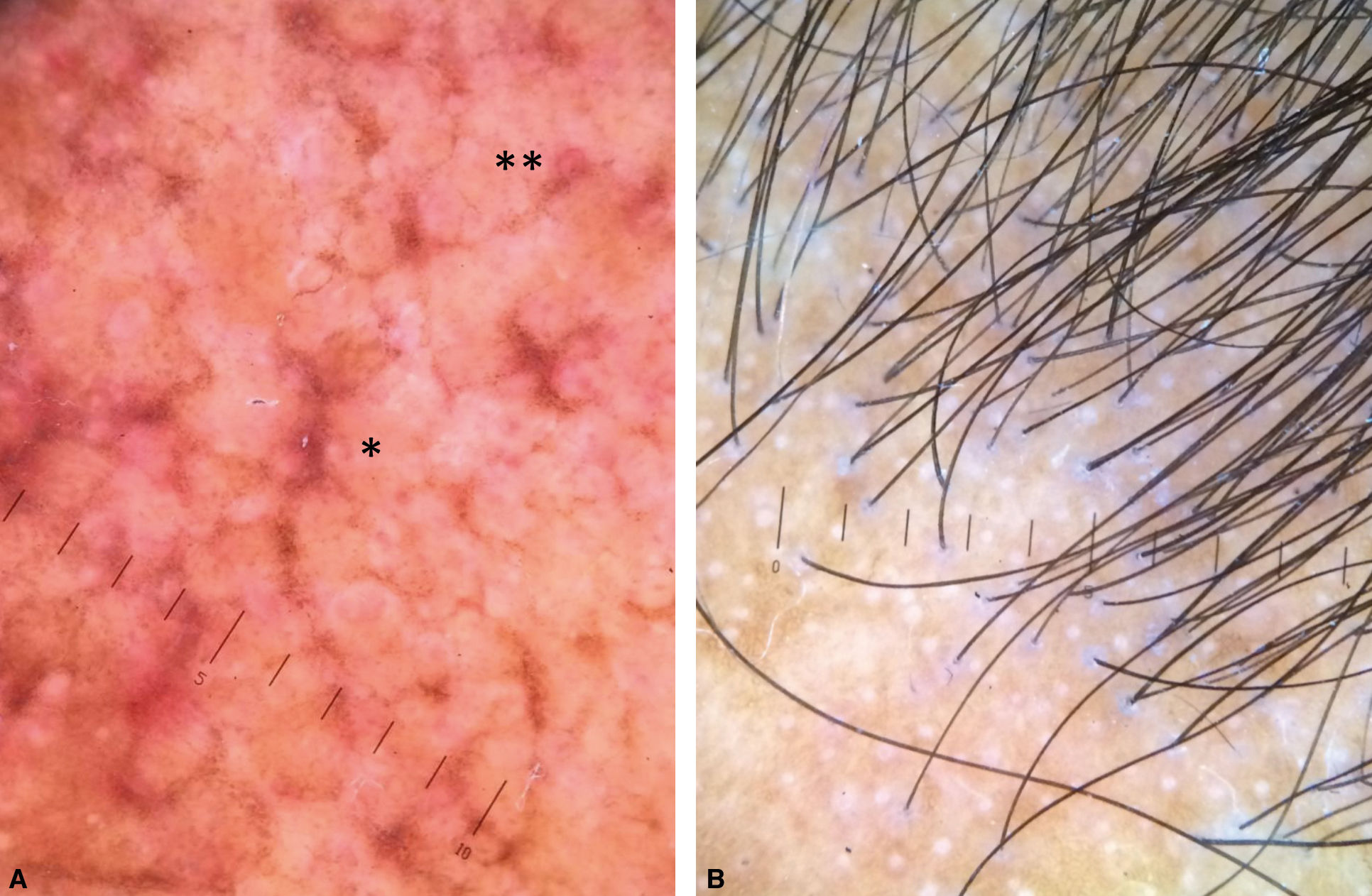
The dermoscopic aspect of early FFA lesions corresponds to erythema and perifollicular scaling; in DLE there are white plaques, arborizing vessels and keratotic plugs. Interfollicular lesions are obvious in DLE, with tortuous and arborizing vessels (blue-red linear ramifications). The loss of follicular openings is common to both conditions in the late phases.8
Our patient had on the scalp perifollicular scaling, small caliber interfollicular white dots, and preservation of pigment network, findings consistent with FFA; on the face, there were whitish areas and pigmentation, corresponding to DLE late lesions.
The dermatoscopic features of chronic lesions of lupus erythematosus on glabrous skin are well known: perifollicular whitish halo, keratotic follicular plugs and monomorphic telangiectasias in the early stages, and whitish areas in the late stages.9 In subacute lesions, whitish scales and mixed vascular pattern over an erythematous base were described.10 Our patient had the dermoscopic features of a late discoid lesion (Figure 3).
We reported a case of a patient with associated DLE and FFA. Early clinical features of FFA could not be confirmed on histopathologic examination, since the lichenoid infiltrate can be seen in both conditions. Only after a course of 13 years did we observe the typical features of FFA. Even though we can consider that the initial biopsy might have been performed in an area not typical for FFA, we can raise the question if there was an overlapping of both conditions or if it was a progression of a chronic lupus lesion to FFA.
Financial support: None.
Conflict of interest: None.