Adult-onset Still’s disease is a systemic inflammatory disorder of unknown etiology, characterized by skin rash, spiking fever, arthralgias or arthritis, and leukocytosis. The typical skin rash is evanescent, salmon-pink, nonpruritic and maculopapular, predominantly on the extremities. It is considered one of the major Yamaguchi’s criteria in adult-onset Still’s disease. However, atypical skin lesions are also described. Here, a 61-year-old woman with sore throat, spiking fever, polyarthritis and evanescent salmon-pink nonpruritic maculopapular skin rash on the extremities was diagnosed with adult-onset Still’s disease. In addition, atypical brown macules on oral mucosa, localized on the inner lips and tongue were also observed. Biopsy revealed a neutrophilic infiltrate. Despite treatment and improvement of the adult-onset Still’s disease, the atypical oral mucosal lesions persisted.
Adult-onset Still’s disease (AOSD) is a systemic inflammatory disorder of unknown etiology, characterized by evanescent non-pruritic, maculopapular, salmon-pink skin rash, spiking fever, arthralgias or arthritis, and leukocytosis (>10000mm3) with at least 80% neutrophils. Other signs and symptoms include sore throat, lymphadenopathy, splenomegaly, hepatomegaly and systemic involvement. Elevated erythrocyte sedimentation rate, C- reactive protein (CRP) and ferritin is common. The diagnosis needs clinical suspicion, and the exclusion of infection, malignancy, and systemic disease. The diagnostic criteria for AOSD proposed by Yamaguchi et al show 96.2% sensitivity and 92.1% specificity when two or more criteria are present.1 Typical skin rash, which flares and fades with the rise and fall of fever, is well-known, and it is considered one of the major criteria of AOSD. However, atypical lesions like persistent papular lesions, pruritic edematous erythema, urticaria, and linear pigmentation are also described in AOSD.2 This article reports a case with atypical oral mucosal lesions in a patient with the diagnosis of AOSD.
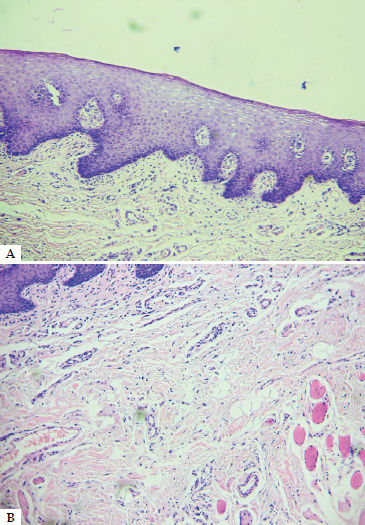
Case ReportA previously healthy 61-year-old woman presented with sore throat, spiking fever once a day of 39.5-40°C at night, with marked polyarthritis of the carpometacarpal and proximal interphalangeal joints, elbows, knees, and ankles. An evanescent, salmon-pink, nonpruritic, maculopapular skin rash was present on the extremities. Laboratory findings were: leukocytosis (14,000mm3 - neutrophils 80%), ESR 100mm, CRP 45 mg/dl (normal range <5.0), ferritin levels >20000ng/ml (normal range: 10–277ng/ml). Other biochemical parameters were within the normal range. Rheumatoid factor and antinuclear antibodies were negative, as well as other immunological tests. Serum protein electrophoresis, complement factors, typical and atypical viral serology were normal/negative. Chest X-ray, electrocardiogram, and echocardiogram were normal. Thoracic, abdominal and pelvic computed tomography imaging scan did not show a primary disease. Extensive cultures for infections were negative. The patient had all Yamaguchi’s diagnostic criteria and other immunologic, infectious and malignant conditions were excluded. An adult-onset Still’s disease was diagnosed. The patient also had brown macules on the oral mucosa, localized on the inner lips and tongue, of approximately 5 mm in the larger diameter, which appeared with the onset of the clinical manifestations (Figure 1). No other mucosal lesions were observed. The AOSD improved with prednisone but, due to the persistence of the polyarthritis, methotrexate was prescribed. Despite the treatment, the oral mucosal lesions persisted and a biopsy was done. The epithelium was preserved, but a perivascular inflammatory infiltrate with a predominance of neutrophils and edema was found in the dermis (Figure 2).
Still disease was described by George F. Still in 1897 in 22 children with chronic polyarthritis referred to as juvenile rheumatoid arthritis. Bywaters described 14 cases resembling Still’s disease that started in adulthood and named it adult-onset Still’s disease.3 The typical skin rash described by Bywaters was characterized by small macules, often with peripheral pallor, that do not spread as in erythema marginatum. These macules disappear during the night to reappear with fever on the next day on a different area, usually on the limbs, but may also appear on the face and trunk. Outlined friction lines may be seen.4 Cutaneous involvement occurs in about 80% of patients and represents one of the Yamaguchi’s criteria.1 The most common skin manifestation is a nonpruritic, evanescent, maculopapular, salmon pink or erythematous exanthema, predominantly on the trunk and proximal limbs, with rare involvement of face and distal limbs, frequently evanescent and prominent during febrile spikes. The spectrum of histopathologic findings in cutaneous lesions are nonspecific.4
Other less common skin manifestations of AOSD have been reported. Itchy annular erythema chronicum migrans, frequently seen in patients with Lyme’s disease, is described in AOSD.5 In addition to the typical rash, persistent papular lesions on face, neck and upper and lower back are also reported.6Pruritic edematous erythemas with persistent plaques are reported in other patients, mainly on the trunk. These lesions persist even when the fever disappeared and show prominent linear pigmentation.7Urticaria and fixed plaques, prurigo pigmentosa-like lesions represents an eruption seen in a subset of patients.8,9 Lee et.al. studied evanescent and persistent pruritic eruption in 36 patients with the diagnosis of AOSD. They found that persistent pruritic eruptions are common among patients with AOSD. Other lesions described include lichenoid papules, prominent linear dermographism, dermatomyositis-like lesions, prurigo pigmentosa-like, and lichen amyloidosis-like, in decreasing order.10 In persistent pruritic papules and plaques, the histopathologic findings are characterized by dyskeratosis confined to the upper layers of the epidermis as well as a sparse superficial dermal infiltrate containing scattered neutrophils. The combination of multiple individual necrotic keratinocytes in the upper epidermis and a dermal infiltrate of neutrophils are present in persistent lichenoid.10
Some authors suggest these atypical manifestations could indicate an increased risk of systemic complications or a longer time until clinical remission.
In our patient, the presence of macular lesions on the lips and tongue is an unusual form of presentation which has not been described yet in AOSD. Therefore, some patients with AOSD could have an atypical rash or mucosal lesions as manifestation of AOSD which could persist after treatment.
Financial support: None.
Conflict of interest: None.
Work performed at the Rheumatology Centre, Bone Biology Laboratory, School of Medicine, Universidad Nacional de Rosario, National Council of Scientific and Technical Research (CONICET), Rosario, Argentina; and Pathological Anatomy Department, Pergamino, Argentina.