Crusted scabies is a less common variant of scabies that is highly contagious, difficult to treat and involves infestation by Sarcoptes scabiei var.hominis. The classical clinical presentation includes crusted, scaly and generally non-pruritic lesions usually located on the head, neck, palmar, plantar and periungual region. It was first described in Norway in 1848 in patients with leprosy who presented with crusted lesions. In this study, we report the case of a patient with crusted scabies with florid clinical manifestations and chronic liver disease due to hepatitis B and delta virus infection.
Crusted scabies (CS) is a less common variant of scabies with a massive infestation by Sarcoptes scabiei var. hominis, related to poor hygiene, institutionalization, immunosuppressive conditions or medications, psychiatric disturbances and sensory neuropathies as predisposing factors.1 The diagnosis of the disease is clinical; however, in cases of diagnostic uncertainty, microcopy of skin scrapings or histopathology can be performed.2 Treatment is preferentially with ivermectin 200μg/kg on days 1, 2, 8, 9 and 15. Permethrin 5% or Sulphur 5% associated with keratolytics can also be used.3
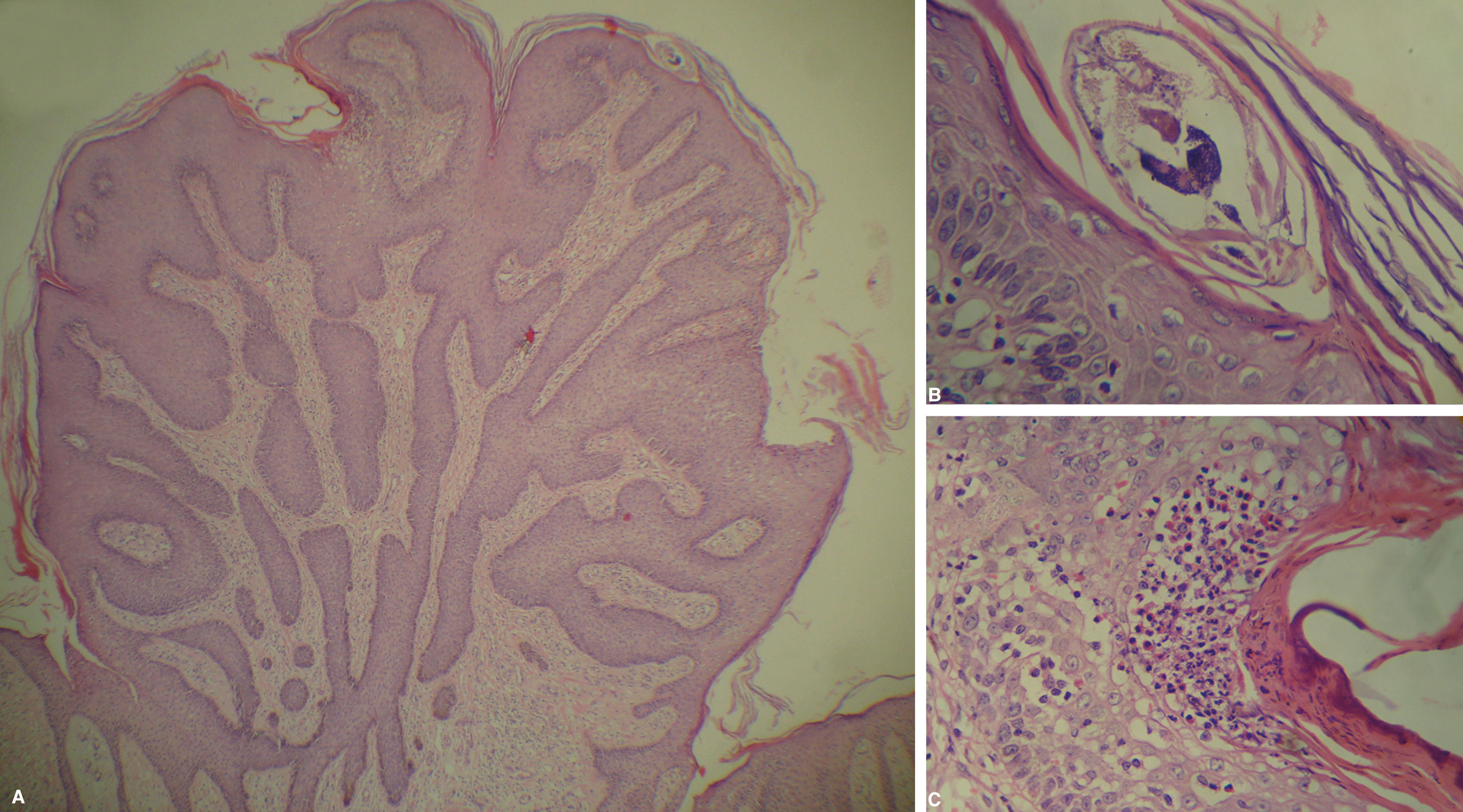
Case ReportA 46-year-old male patient, born in Tapauá (AM) and living in Manaus (AM), attended the dermatology outpatient clinic with grey, scaly, well-defined plaques on the trunk, buttocks and lower limbs (Figure 1). His past history included motor neuropathy due to cerebral palsy. The patient also reported alcohol and tobacco consumption. Direct microscopy from a skin scraping revealed numerous parasites. Histopathology with H&E revealed hyperkeratosis, parakeratosis, papillomatosis, pseudoepitheliomatous hyperplasia, focal intraepidermal eosinophilic infiltrate, besides mites in the stratum corneum (Figure 2). The patient also had peripheral eosinophilia (23%) and monoclonal IgE 20-times higher than normal (2500 U/ml). Serology was positive for hepatitis B and delta viruses, with positive HBsAg, anti-HBc-T, anti-HBe and anti-HDV. HIV and HTLV serologies were negative. Abdominal ultrasound revealed signs of chronic liver disease. Treatment was performed with five doses of ivermectin (200μg/kg/day) and Sulphur 5% associated to salicylic acid in Vaseline for 5 days. He progressed with clinical cure (Figure 3).
Hematoxylin & eosin staining of histology sections revealed hyperkeratosis, parakeratosis, papillomatosis, pseudoepitheliomatous hyperplasia (A -Hematoxylin & eosin, X100), focal eosinophilic infiltrate in the epidermis and mites in the stratum corneum (B and C - Hematoxylin & eosin, X400)
The mechanism for the development of CS is still not totally clear, but it is frequently associated to an imbalance between cellular and humoral immunities. There would be a predominance of the humoral response (T-helper 2) with raised levels of IgE, IgG and eosinophils and negligible cellular immune response in CS. The inability of controlling the parasite multiplication could explain the florid lesions.4 During laboratory screening, we observed that the patient had chronic liver disease due to hepatitis B and delta viruses, which, associated to chronic alcoholism could justify the reduced immunity and the appearance of an extensive and atypical form of CS. The patient was born in Tapauá, a municipality part of the hepatitis B and delta viruses endemic area in the Amazonas.5 The patient responded satisfactorily to the prescribed treatment, and is undergoing follow-up with the dermatology and hepatology clinics.
Financial support: None.
Conflict of interest: None.