Periungual basal cell carcinoma is rare and needs to be differentiated from other common diseases that affect this region. Several factors are associated with the development of this tumor, and sun damage seems to play an important role in its pathogenesis. Dermoscopy of clinically indolent lesions on the nail unit can shorten the diagnostic process and avoid destructive treatment and functional damage.
Basal cell carcinoma is the most common malignancy in humans. It is caused, among other factors, by ultraviolet radiation. However, some areas with high levels of sun exposure, such as the dorsum of the hands and forearms, are rarely affected.1,2 This difference in susceptibility to the development of this tumor in different areas has not yet been fully established.3 Therefore, its occurrence in unusual anatomical sites can usually delay the diagnosis. For this reason, dermoscopy is very effective in identifying these lesions.3,4
This article reports a case of periungual basal cell carcinoma and emphasizes the importance of dermoscopy in the early diagnosis of tumor lesions that affect uncommon sites.
Case ReportA 58-year-old female patient, phototype II, presented with a progressive growth lesion in the periungual region of her left thumb for over two years. She has undergone several treatments with antibiotics and topical corticosteroids, with no response. Clinical history revealed no traumatic or triggering factors that justified the development of the lesion in this area of her body.
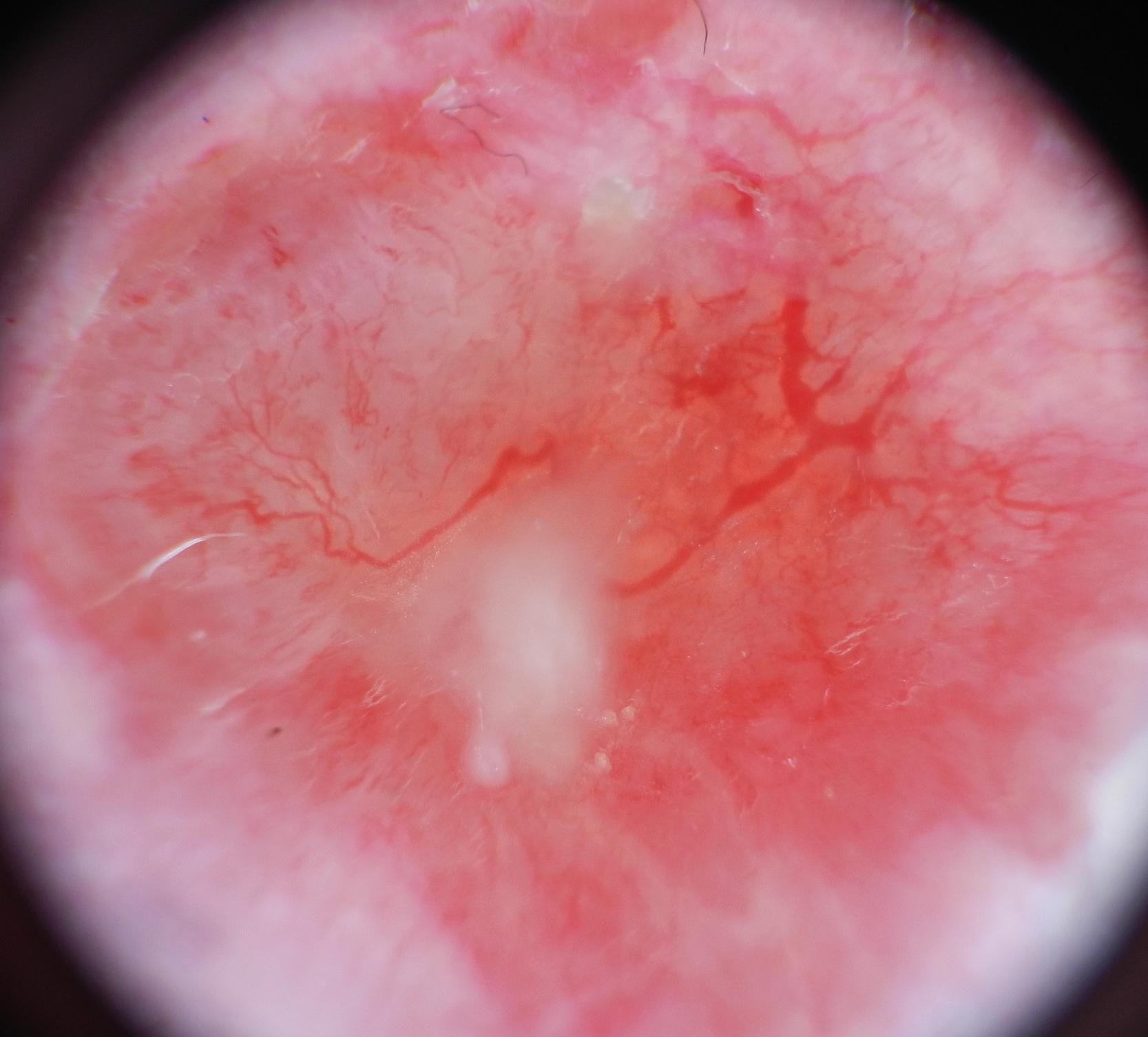
Upon examination, we observed a granulomatous and friable ulcer with infiltrated margins measuring about 2cm in diameter (Figure 1).
Dermoscopy of the lesion revealed an erythematous lesion with typical thin and branched arboriform vessels and a white halo and ulceration (Figure 2). These findings are very suggestive of basal cell carcinoma, but the white halo around the vessels may indicate a keratinocytic origin.
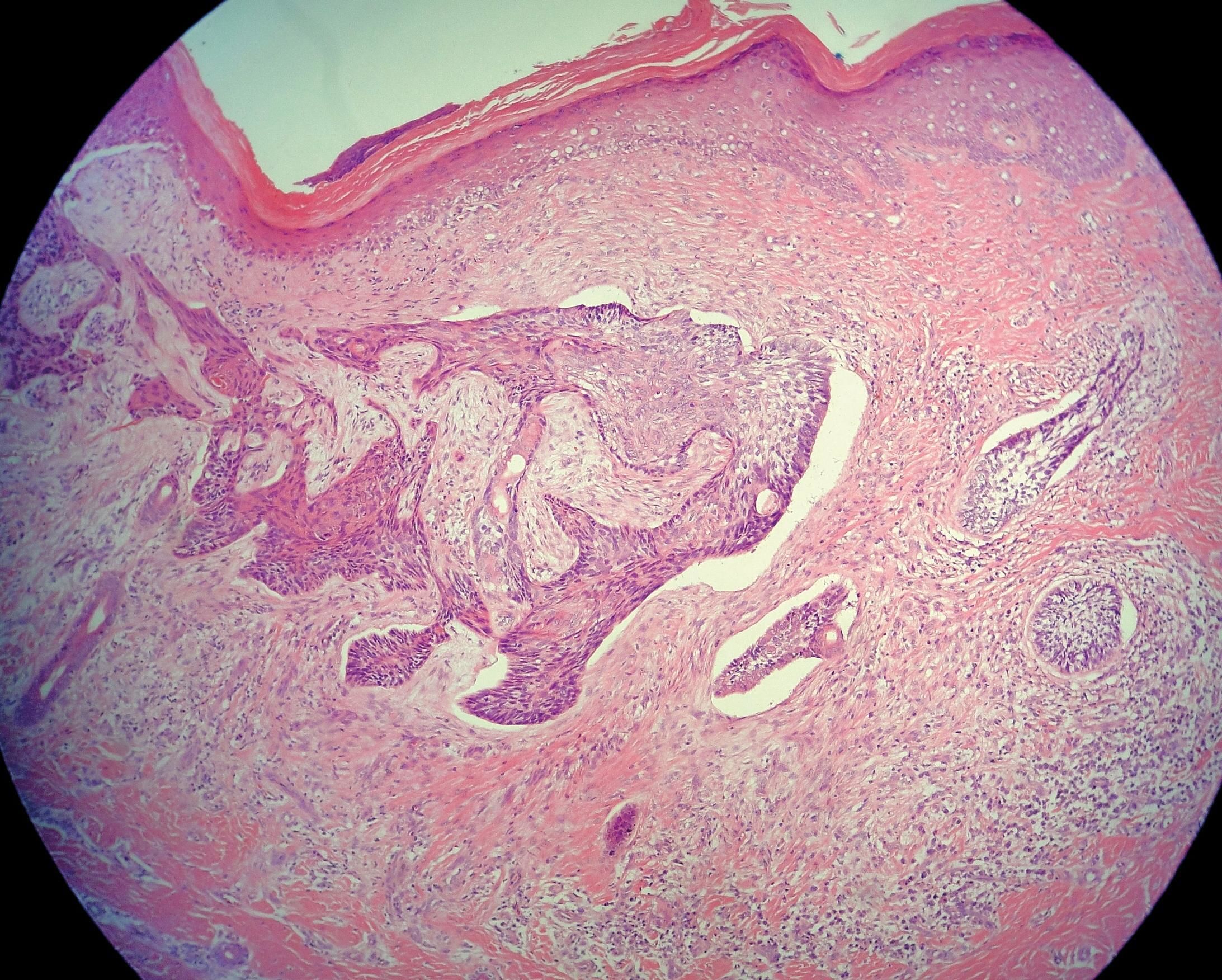
Histopathological examination of incisional biopsy showed a peripheral palisade of basaloid cells and adjacent retraction, as well as swirls of squamous cells, which confirmed the diagnosis of basosquamous cell carcinoma (Figure 3). The patient underwent complete excision of the lesion, with a safety margin of six millimeters, including the nail plate and matrix, and secondary closure and healing by secondary intention. There was no functional damage to her finger, and the aesthetic result was satisfactory.
DiscussionBasal cell carcinoma is a skin tumor believed to be associated with prolonged sun damage. Other factors such as chronic trauma, exposure to arsenic, burns, radiotherapy, and viruses may also be related to the pathogenesis of the disease. The most commonly affected sites are the head and neck. However, it occasionally occurs in covered areas such as the axillae, nipples, inguinal region, and palms. Nevertheless, the involvement of peripheral areas, such as the hands – which are typically photoexposed – is rare and can lead to difficulties and diagnostic delays. The periungual localization is often underdiagnosed and may be confused with other diseases such as chronic paronychia, herpes simplex, and pyoderma, delaying diagnosis and limiting therapeutic possibilities.1,4 Basosquamous carcinoma is a rare and more aggressive subtype of basal cell carcinoma, with characteristics of basal cell carcinoma and squamous cell carcinoma. The latter is more destructive and shows greater local recurrence.5,6 Several treatments can be used to treat this condition. Conventional and Mohs micrographic surgeries are the most employed treatments and the least likely to lead to recurrence.5,7,8 The earlier the diagnosis, the greater the chances of preserving the nail structures with less functional damage.
Basal cell carcinoma has well-established dermoscopic criteria that help differentiate between the different types of skin tumors and between tumor and infectious lesions. With dermoscopy, we are able to assess margins and responses to therapeutic methods. In addition, we can improve recommendations for biopsies to identify complex lesions, making diagnosis faster and more accurate.2,3,8
Financial support: None.
Conflict of interest: None.