Sweet’s syndrome is a rare dermatosis with little-known pathogenesis, associated with some clinical conditions such as infections, autoimmune diseases, inflammatory bowel diseases, vaccination, medications and neoplasms. Hematologic malignancies are the diseases most related to paraneoplastic Sweet’s syndrome, but this clinical entity can also be found occasionally in some solid tumors, including genitourinary tract tumors. We report a rare case of paraneoplastic Sweet’s syndrome associated with the diagnosis of cervical cancer.
Paraneoplastic syndromes are clinical conditions that are related to primary or metastatic tumors but are not directly attributed to the physical effects of these neoplasias. They can occur concomitantly or precede the oncological condition, and the treatment of the neoplasia generally leads to their resolution.
Sweet’s syndrome was first described by Robert Douglas Sweet in 1964. It is a rare, etiologically unknown dermatosis that can be idiopathic or associated with certain clinical conditions.1 Among these conditions are infections, autoimmune diseases, inflammatory bowel diseases, vaccinations, the use of medications, and neoplasias. Hematological neoplasias, particularly acute myeloid leukemia, are the most commonly described, but the condition may also be related to solid tumors, being those of the genitourinary tract the most associated with the syndrome.
Case ReportA 58-year-old female patient, with recent diagnosis and treatment of cervical cancer, was taken to the oncological dermatology clinic of the hospital due to the sudden appearance, five days earlier, of painful, macular, erythematoviolaceous lesions on the palms, with subsequent emergence of nodular lesions and plaques on the upper and lower limbs. The patient stated that, concomitant to the cutaneous presentation, there was fever (not measured), indisposition and general malaise. She had been treated with three cycles of chemotherapy three months before, the first two with cisplatin combined with radiotherapy, and the last with paclitaxel and carboplatin.
A physical examination found nodular and erythematous lesions, some with a target-like aspect, on the arms and legs; erythematous pseudo-vesicular plaques on the forearms, and painful erythematoviolaceous macules on the palms (Figures 1–3).
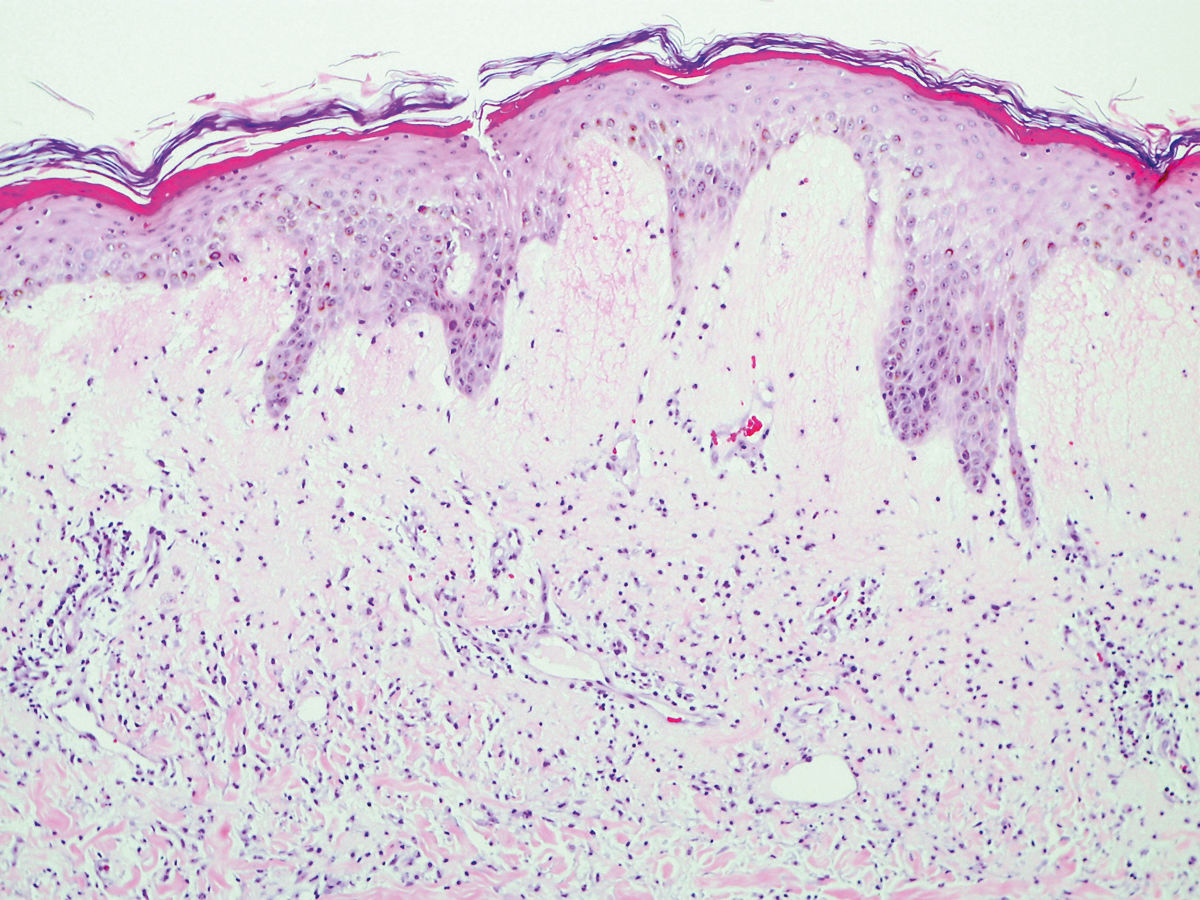
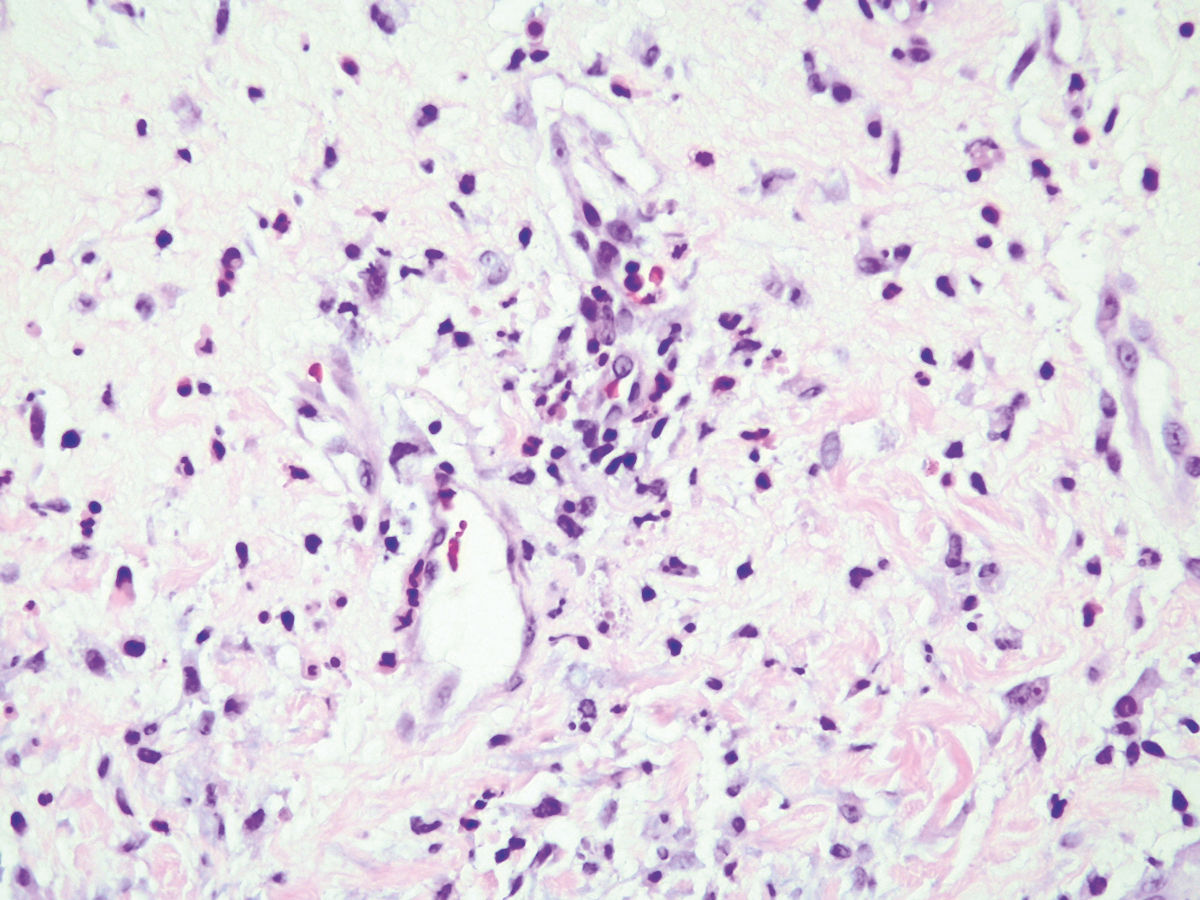
Given the clinical findings, Sweet’s syndrome was suspected. A hemogram was ordered and a pseudo-vesicular plaque on the left forearm was biopsied. The patient returned with the hemogram results, which showed anemia, discrete leukocytosis, unchanged neutrophils, and thrombocytosis. The results of the histopathological examination were compatible with Sweet’s syndrome: hyperkeratosis, foci of parakeratosis, intracorneal neutrophilic microabscesses, subcorneal and papillary dermal edema, and mixed inflammatory infiltrate with leukocytoclasia in the upper dermis (Figures 4 and 5).
Treatment began with prednisone at a dose of 0.5mg/kg/day, with significant improvement of the lesions. The condition recurred with a reduction in the prednisone dosage. The typical presentation of Sweet’s syndrome indicated the relapse of the tumor, and the patient was subsequently taken for new treatment. After the reintroduction of chemotherapy and radiotherapy, the patient presented total resolution of the condition without the use of prednisone.
DiscussionSweet’s syndrome is a rare dermatosis characterized by cutaneous lesions, fever, neutrophilia, and dense dermal infiltrate of neutrophils. Clinically, the lesions present as papules, nodules, and taut, painful, erythematous plaques distributed asymmetrically, mainly on the face, neck and upper limbs. Since its first report, this syndrome has been associated with infections, malignant diseases, drugs, autoimmune diseases, and vaccines.1
Although the pathogenesis in not well known, approximately 21% of the patients that present Sweet’s syndrome have some associated malignant disease. Of these, 85% have hematological neoplasias, and 15% have solid tumors, most commonly of the genitourinary tract.2 The presence of anemia and of abnormal platelet counts, absence of neutrophilia, and locations and forms of atypical presentation of the disease emphasize the need to investigate associated neoplasms, since these findings are uncommon in the idiopathic form.3
Sweet’s syndrome generally responds well to treatment with corticosteroids, independent of the hidden malignant neoplasm, and treatment of the neoplasia results in complete remission of the syndrome.4
In the present report of the clinical and histopathological diagnosis of Sweet’s syndrome, we considered it to be of paraneoplastic etiology, based on the laboratory tests and on the fact that the patient is known to have cervical neoplasia. Paraneoplastic Sweet’s syndrome was then diagnosed, and treatment of this pathology was initiated. Currently in the literature, only four cases relate Sweet’s syndrome to cervical cancer.5,6
The preferred treatment for neoplasia associated with Sweet’s syndrome is that in progress and may result in complete remission of the syndrome in the case of a solid tumor. However, a cycle of systemic corticosteroid is administered preliminarily. Systemic corticosteroids are the reference standard in the treatment of classic Sweet’s syndrome, and prednisone is the most commonly used drug.7 Nevertheless, there is no specific guideline for the treatment of Sweet’s syndrome related to malignant neoplasias.2
The diagnosis of Sweet’s syndrome in patients known to have neoplasia must be promptly assessed due to the possibility of persistent, recurrent or metastatic disease.
Therefore, Sweet’s syndrome may be a warning sign for the detection of undiagnosed neoplasms. The cutaneous signs offer physicians an opportunity to detect and treat incipient cancer. This article highlights the importance of the recognition of Sweet syndrome and its presentation as a paraneoplastic disease.
Financial support: None.
Conflict of interests: None.