Papular elastorrhexis is an acquired disease of elastic tissue; considered rare, its etiology and pathogenesis remain unknown. The vast majority of cases occur in women in the first or second decade of life. The disease manifests as multiple uniformly-sized, circumscribed, hypochromic and achromic papules located predominantly on the trunk and upper extremities. The lesions are generally asymptomatic and have a stable evolution over years. Its diagnosis is based on clinical and histopathological findings. The benignity of papular elastorrhexis and the subtlety of its clinical changes make the expectant treatment perfectly viable. The authors present one case in a young female patient.
Papular elastorrhexis is a disease of elastic tissue; considered rare, its etiology and pathogenesis remain unknown. Most cases occur in females in the first or second decade of life. There is usually no history of trauma, inflammation or previous acne. The disease is characterized by multiple small, uniformly-sized, circumscribed, hypochromic and achromic, non-follicular, oval or round papules located predominantly on the torso and upper extremities.
Case ReportA 25-year-old white, female patient A 25-year-old white, female patient complained of lesions on the anterior side of the thorax and on the upper portion of the back, which emerged approximately seven years prior to the appointment, during pregnancy, and was accompanied by mild pruritus, pain and erythema. She was a smoker, G1 P1 A0, and was using only oral contraception. There was no family history of dermatological affections or neoplasias.
During physical examination, papule-type lesions of whitish and yellowish coloration were noted on the anterior side of the thorax and on the upper part of the back (Figures 1 and 2). Grade 1 acne was also observed on the face. Steatocystoma multiplex and post-acne scarring were hypothesized, and a punch biopsy was performed.
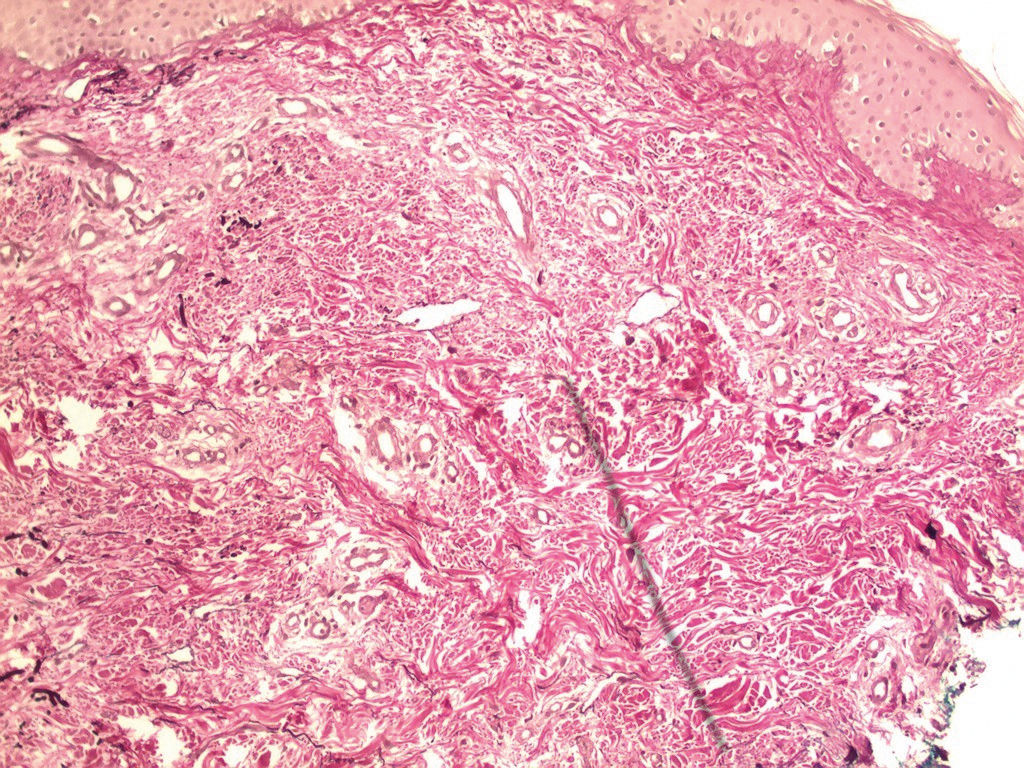
The histopathological examination revealed an area of the skin with thickening of the dermal connective bundles, and Weigert’s stain showed elastic fibers to be thin, fragmented and in reduced number in the examined topography, supporting the hypothesis of an elastic tissue disease such as papular elastorrhexis (Figure 3).
The patient was informed regarding the benignity of the condition. The proposed treatment was 2% triamcinolone infiltration on the lesions and, in refractory cases, an oral isotretinoin prescription.
DiscussionPapular elastorrhexis is an elastic tissue disease that is considered rare and whose etiology and pathogenesis remain unknown.1,2 The majority of cases occur in females in the first or second decade of life, in an episodic and acquired manner.1,2 Rarely, an association with atopic dermatitis is observed.3 There is usually no history of trauma, inflammation or previous acne.1,4
The disease is characterized by multiple small, circumscribed, uniformly-sized, hypochromic and achromic, non-follicular, oval or rounded papules located predominantly on the torso and upper extremities.1,2,5 Rarely, there is involvement of the mandibular, occipitocervical and retroauricular regions, face and scalp.3 The lesions are generally asymptomatic, with a stable evolution over years.1 No extracutaneous manifestations have been reported.1
The diagnosis of papular elastorrhexis is based on clinical and histopathological findings.6 The histopathological assessment of the lesions reveals characteristic rarefaction and important fragmentation of the elastic fibers of the reticular dermis.4,5 There can be a perivascular lympho-histiocytic infiltrate. The collagen is thickened or normal.1,3 The presence of mucin should be evaluated during the histopathological examination to exclude associated diseases, such as lymphoma.1
Papular elastorrhexis was previously postulated to be a variant of nevus anelasticus or an abortive form of Buschke-Ollendorff syndrome.1 Currently, however, most authors agree that the disease is an entity distinct from the other.3Nevus anelasticus is a predominantly congenital condition characterized by asymmetric, grouped, perifollicular papules on the anterior region of the thorax.5 The most important histopathological finding is a considerable reduction in the number of elastic fibers; in papular elastorrhexis, the fragmentation of such fibers is more characteristic.3
Buschke-Ollendorff syndrome is a dominant autosomal disease characterized by disseminated connective tissue nevi, associated with osteopoikilosis (disseminated condensing osteopathy).5 Elastomas are more commonly found in this syndrome, and the histopathology reveals an accumulation of elastic fibers, forming clusters.4,5 Papular elastorrhexis, however, differs from Buschke-Ollendorff syndrome in that it does not present hereditary characteristics, having a later onset, and does not present signs of osteopoikilosis.4
In addition to nevus anelasticus and Buschke-Ollendorff, the differential diagnosis includes eruptive collagenoma, papular acne scars, anetoderma, mid-dermal elastolysis, disseminated lenticular dermatofibrosis, postinflammatory elastolysis, pseudoxanthoma elasticum, and cutis laxa.
Eruptive collagenoma is an acquired disease that manifests in youth and is characterized by the presence of connective tissue nevi.7 The histopathology reveals an abnormal accumulation of components of the extracellular matrix (collagen, elastic fibers and glycosaminoglycans).7
Papular acne scars are, obviously, associated with a history of acne and do not occur in areas such as the abdomen and thighs.7 In anetoderma and mid-dermal elastolysis, elastolysis occurs in the absence of elastorrhexis, and the collagen is usually normal.7
Currently, there is no specific treatment for papular elastorrhexis.3 Being a benign disease with only cosmetic complications, expectant management is acceptable.3 Some therapeutic options include oral antibiotics, oral isotretinoin, topical isotretinoin, benzoyl peroxide, and intralesional injection of triamcinolone; however, the response is variable and generally absent.1,3,4
Financial support: None.
Conflict of interests: None.