Dear Editor,
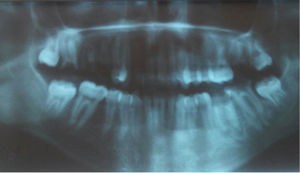
Papillon-Lefèvre syndrome is a rare, autosomal recessive genodermatosis with an estimated prevalence of one to four cases per million people, without sexual or racial predominance.1 It is clinically characterized by diffuse palmaoplantar keratoderma, associated with a severe periodontopathology, with premature loss of deciduous and permanent teeth.1 The cutaneous changes commonly begin during the first four years of life, and the severe destruction of periodontal regions results in loss of the primary teeth within these first four years, as well as premature loss of the permanent teeth.1 The syndrome is caused by a mutation in the gene that encodes the protein cathepsin C, a lysosomal protease known as dipeptidyl-peptidase 1, present in the epithelial regions commonly affected by the syndrome, as well as in cells of the immune system, including polymorphonuclear leukocytes, macrophages and their precursors.1 This case is reported because of the rarity of its pathology and to highlight the importance of the presence of extracutaneous manifestations in diffuse palmoplantar keratodermas, which are often erroneously diagnosed as psoriasis. This case involves a 17-year-old male patient with a history of gingival and periodontal changes since the age of three. The patient mentioned softening and breakage of the teeth, accompanied by halitosis, since the age of eight. In the last three years, exuberant asymptomatic palmoplantar keratoderma has evolved, accompanied by diffuse palmoplantar hyperhydrosis, requiring the continuous use of socks to reduce the discomfort of humidity. He presented a history of multiple hospitalizations for pneumonia and gastroenteritis during infancy, as well as a report of consanguinity. In the dermatological exam, the patient presented accentuated palmoplantar hyperkeratosis on the hands and feet (Figure 1). The oral cavity showed edema and gingival erythema, with bleeding upon manipulation, and the presence of purulent secretion from the lower gingiva (Figure 2). Panoramic radiography of the dental arch revealed areas of alveolar bone loss and ridge resorption (Figure 3). Treatment with acitrentin, emollients and keratolytics was initiated, with satisfactory improvement in the keratoderma and the odontological condition. The palmoplantar keratoderma in Papillon-Lefèvre syndrome typically begins within the first four years of life, with keratotic plaques on the palmar and plantar regions.1,2 Coeli et al. (2008) and Sharma et al. (2013) described cases of this syndrome that presented typical palmoplantar keratoderma in the first year of life, differing from the case described in this report, which presented delayed onset of the cutaneous involvement at 14 years of age.1,2 Severe periodontopathy is the principal oral manifestation of the syndrome, with premature loss of deciduous dentition between the fourth and fifth years of life, and loss of permanent dentition around the fourteenth year. The reported case and the cases described by Coeli et al. (2008) and Kaur et al. (2013) corroborate the early onset of oral manifestations.1–3 In the reported case, the patient presented a history of frequent hospitalizations during infancy for pneumonia and gastroenteritis, which confirms the important susceptibility to infections, described by Liu et al. (2000) and Khan et al. (2012), due to decreased phagocytosis of neutrophils, decreased chemotaxis of leukocytes and peripheral lymphocyte reduction.4,5 The relationship between this genodermatosis and consanguinity is described in 20% to 40% of cases in the literature and is corroborated by the association presented in this case.4,5 The histopathological exam of the lesions is nonspecific, with hyperkeratosis, irregular parakeratosis and moderate perivascular inflammatory infiltrate, the diagnosis being eminently clinical.3–5 Electron microscopy showed vacuoles similar to lipids in the corneocytes and granulocytes, a reduction of tonofilaments and abnormal keratohyalin granules. The cutaneous maifestations are usually treated with keratolytics, emollients and systemic retinoids, with excellent response of the cutaneous lesions and a reduction of edema and gingival erythema, which was proved by the satisfactory therapeutic response in the case reported here and in the cases described by Coeli et al. (2008).1,3,5 The appropriate dermatological treatment, combined with early odontological treatment, is capable of reversing the cutaneous condition, avoiding loss of dentition and, therefore, significantly improving the quality of life of patients.
Financial support: None.
Conflict of interest: None.