Dear Editor,
Cutaneous mucinoses are a group of diseases in which there is an abnormal deposit of mucin in the skin. It can be classified into primary and secondary forms. An uncommon subtype of primary mucinosis, acral persistent papular mucinosis (APPM) is currently considered as a clinicopathological variant of lichen myxedematosus.
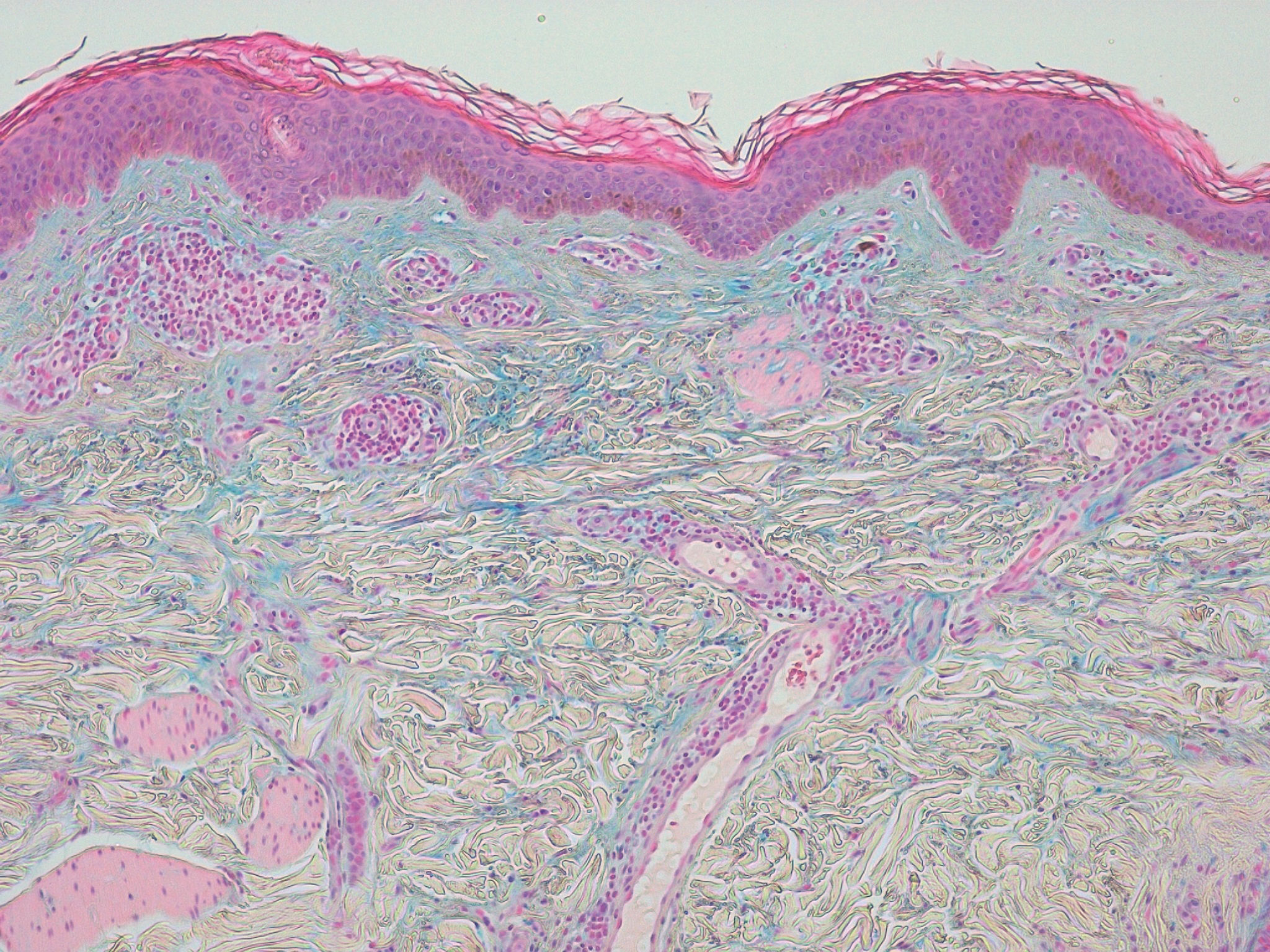
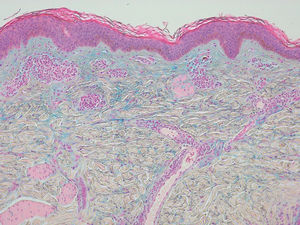
A 31-year-old woman presented a 10-year history of persistent pruritic lesions on her arms. She had no relevant medical history. Physical examination revealed multiple, non-follicular and small (2-5 mm) skin-colored papules, some of them translucent, on the dorsum of both forearms (Figure 1). There were no other similar lesions on the rest of the body. The patient reported that topical corticosteroids were ineffective and sun exposure increased the number of lesions. Laboratory studies were within normal range, including blood cell count, liver, kidney and thyroid function. Antinuclear antibodies were negative. Skin punch biopsy of a papule was performed and histopathological examination showed no alteration in the epidermis. There was a focal area in the upper and mid reticular dermis due to a separation of collagen fibers. Deposit of mucin in the papillary dermis that stained positively with alcian blue was observed. There was no deposit of mucin in the reticular dermis. Fibroblast proliferation was not evident (Figure 2). APPM was then diagnosed.
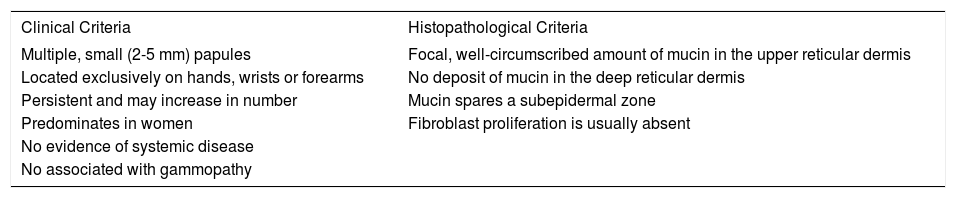
APPM was first described by Rongioletti et al. in 19861 and the etiology is unknown, although both genetic and environmental factors are thought to play a role. Rongioletti and Rebora in 2001 proposed several diagnostic criteria for APPM and, to date, there have been more than 30 reported cases of this entity that met the criteria (Table 1).2 Three cases showed family history.3 Clinically, it is characterized by small flesh-colored, papules that most often are symmetrically localized on the back of the hands, wrists and extensor aspects of distal forearms. Differential diagnosis includes lichen nitidus, common warts and other forms of mucinosis. The lesions are usually asymptomatic, although in our case they were very pruritic. They tend to persist and may increase slowly. There is a female predominance. Neither systemic disease nor monoclonal gammopathy in peripheral blood are observed in this entity. The possible association with malignancies has not been clarified yet.4 The typical histopathology of APPM is a focal, well-circumscribed deposit of mucin in the papillary and mid-dermis. The deposit never extends to the deep reticular dermis. Fibroblastic proliferation is variable, although normally they are not increased in number. Due to the absence of symptoms, treatment is rarely necessary. APPM has been treated with topical corticosteroids, tacrolimus, pimecrolimus, liquid nitrogen, electrocoagulation and Erbium-YAG laser with some success.5 In our case, the patient reported pruritus, so we treated with topical 0.1% tacrolimus ointment for five weeks, but it was ineffective. We prescribed a fluid emulsion 12% sodium lactate for two months and the symptoms disappeared. We herein present a new case of this rare mucinosis. It is important to know that most cases are asymptomatic, but in our case, the patient presented pruritic lesions.
Diagnostic criteria for APPM
| Clinical Criteria | Histopathological Criteria |
|---|---|
| Multiple, small (2-5 mm) papules | Focal, well-circumscribed amount of mucin in the upper reticular dermis |
| Located exclusively on hands, wrists or forearms | No deposit of mucin in the deep reticular dermis |
| Persistent and may increase in number | Mucin spares a subepidermal zone |
| Predominates in women | Fibroblast proliferation is usually absent |
| No evidence of systemic disease | |
| No associated with gammopathy |
Financial support: None.
Conflict of interest: None.