Dear Editor,
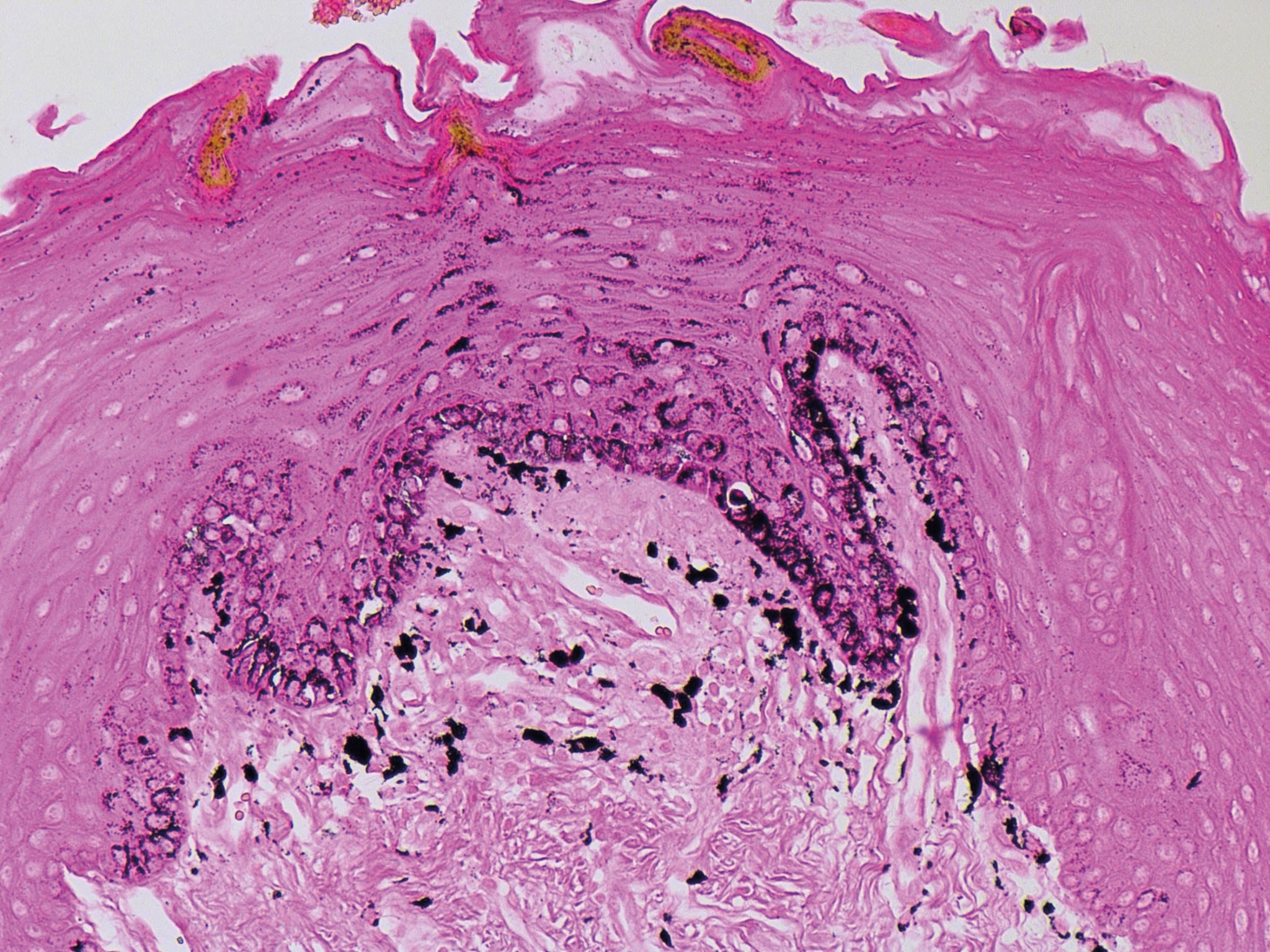
Lingual melanotic macule is a rare entity that, when reported, is usually congenital. We report the case of a 28-year-old female patient who presented with a lesion with no comorbidities. The patient was a non-smoker with no dental restoration and a family history of basal cell carcinoma. She reported a stable asymptomatic brown spot on the tongue for three months, with no history of bleeding or local trauma. She denied the use of prescription drugs. Physical examination revealed a homogeneous dark brown macule, with relatively regular borders, 4x3 mm in diameter, located on the right lateral border of the tongue (Figure 1). In the region adjacent to the lesion, we noted a 6mm light brown spot. Based on clinical findings, the diagnostic hypotheses included melanotic macula, melanoma, fixed pigmented erythema, and postinflammatory hyperpigmentation. An excisional biopsy was performed, and anatomopathological examination confirmed the diagnosis of lingual melanotic macula (Figure 2).
Multiple causes of hyperpigmented lesions of the oral mucosa are known, with oral and labial melanotic macules as the most common melanotic lesions.1,2 Trauma, radiation, and medications may result in an increased production of melanin seen in melanotic macules, but the pathophysiological mechanism of this disorder is still unknown.1,2 Histologically, melanotic macula of the oral and labial mucosa is characterized by increased melanin in the basal cell layer and lamina propria. Pigmentary incontinence may be present.1-3 Diagnoses of hyperpigmented lesions of the oral mucosa include physiologic melanin pigmentation, drug-induced skin pigmentation, oral melanocytic nevus, melanoma, black hairy tongue, oral melanoacanthoma, smoker’s melanosis, amalgam tattoo, postinflammatory hyperchromia, and Laugier-Hunziker syndrome (pigmentation of the oral mucosa associated with melanonychia). Hyperchromia in Addison’s disease is more diffuse and there are signs of systemic involvement. In Peutz-Jeghers syndrome, pigmentation is more extensive and speckled. In most cases, such diagnoses can be ruled out through clinical history and physical examination.1,2,4
With only a few reports, lingual melanotic macule is considered a rare or underdiagnosed entity.1,2 In a review of the literature in 2015, Savoia et al. found 14 cases of congenital lingual melanotic macules.4 The present case would be the first and only described in an adult patient, based on a survey conducted in December 2016 on PubMed using the keywords “tongue”, “melanotic macule,” and “adult”.
Most melanotic macules are congenital, affect Caucasian individuals, may be single or multiple, have a diameter varying between 0.3cm and 3cm, tend to grow in proportion to the body growth, and are unrelated to any systemic condition.2,4 Their clinical features are not yet well-defined.1,2 The etiology of the disease still remains uncertain, but it is suggested that congenital cases may represent melanocyte hamartomas.2
Histology of the described cases of lingual melanotic macule reveals increased melanin in the basal cell layer, some pigment-laden macrophages in the dermis, normal number of melanocytes with no or a slight increase of melanin in their interior and variable degrees of hyperkeratosis.2 There are no nests of melanocytes, atypia, or alterations in the lingual tissue, and, in some cases, slight elongation of the epithelial ridges has been described.2 Also, according to Dohil et al., no similar histopathological alteration was identified in the non-affected lingual tissue.2
Our patient is an adult woman, which is uncommon when compared to other cases described. The most relevant differential diagnosis in this case would be to rule out the possibility of melanoma.
Some authors recommend anatomopathological examination for diagnostic confirmation, although others sustain that the diagnosis is only clinical and follow-up is necessary to investigate changes in size, shape, and color of the lesion.2,4 Although the number of documented cases allows no definitive conclusions, a clinical diagnosis of congenital melanotic macule of the tongue should be considered in the presence of the following characteristics: single or multiple lingual melanotic lesions, presence of a macular lesion at birth with proportional growth, and absence of family history of systemic conditions associated with mucosal pigmentation.2 For acquired cases, lingual melanotic macules, although rare, should be considered in the differential diagnosis of pigmented lesions of the oral mucosa. Dohin et al. suggest that the biopsy sample of lingual melanotic lesions include normal tissue so that it is easier to compare the normal pigmentation with that of the lesion.2
Although lingual melanotic macule is a benign condition, an important differential diagnosis is made with melanoma. Therefore, we reiterate the importance of anatomopathological examination, especially in acquired cases.
Financial support: None.
Conflict of interests: None.
Financial support: None.
Conflict of interests: None.