We report the case of a 24-year-old female, Fitzpatrick phototype V, referred to our Dermatology Department for an asymptomatic mass in her left dorsal region. The patient reported a slow growth of this mass over several years. Physical examination revealed a palpable, soft, subcutaneous tumor in the left dorsal region, without apparent involvement of the superjacent skin, which was painless on palpation. The remainder of the examination was otherwise normal.
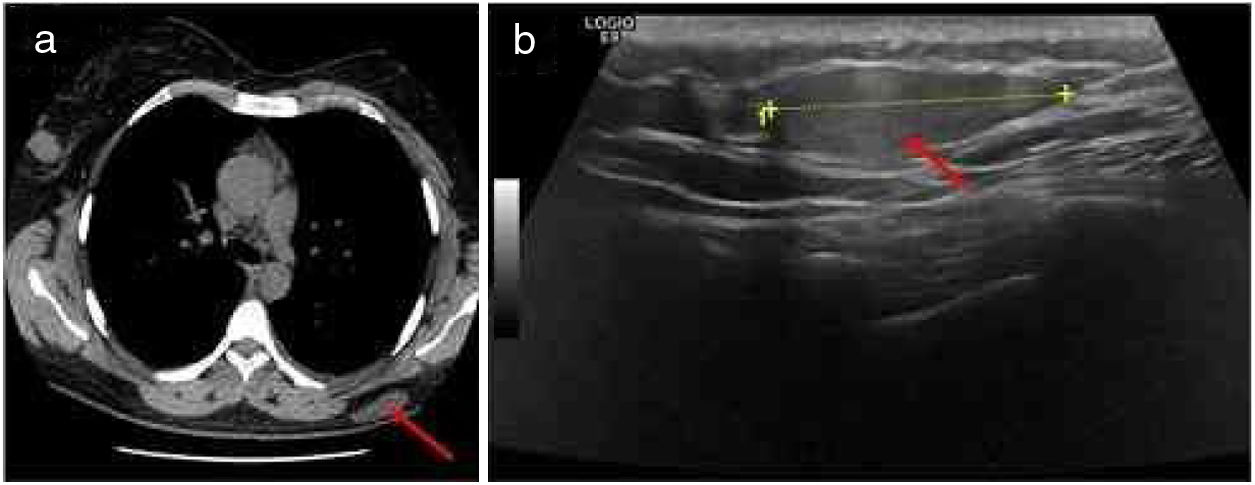
A high-resolution thoracic computed tomography performed one year before, in the context of an episode of asthma exacerbation, had revealed a large, low-density, subcutaneous nodularity in the referred topography (Fig. 1A). Also, an ultrasound-guided core needle biopsy (Fig. 1B)of this well-defined, slightly hyperechoic, subcutaneous mass identified a neoplasm of globular cells, some with multi-vacuolated cytoplasm and others with granular, eosinophilic cytoplasm, without nuclear atypia.
Imagiological features of the tumor: A, High-resolution thoracic computed tomography revealing a large, low-density, subcutaneous nodule in the left dorsal region (red arrow); B, Ultrasound revealing a well-defined, slightly hyperechoic, subcutaneous mass in the left dorsal region (red arrow).
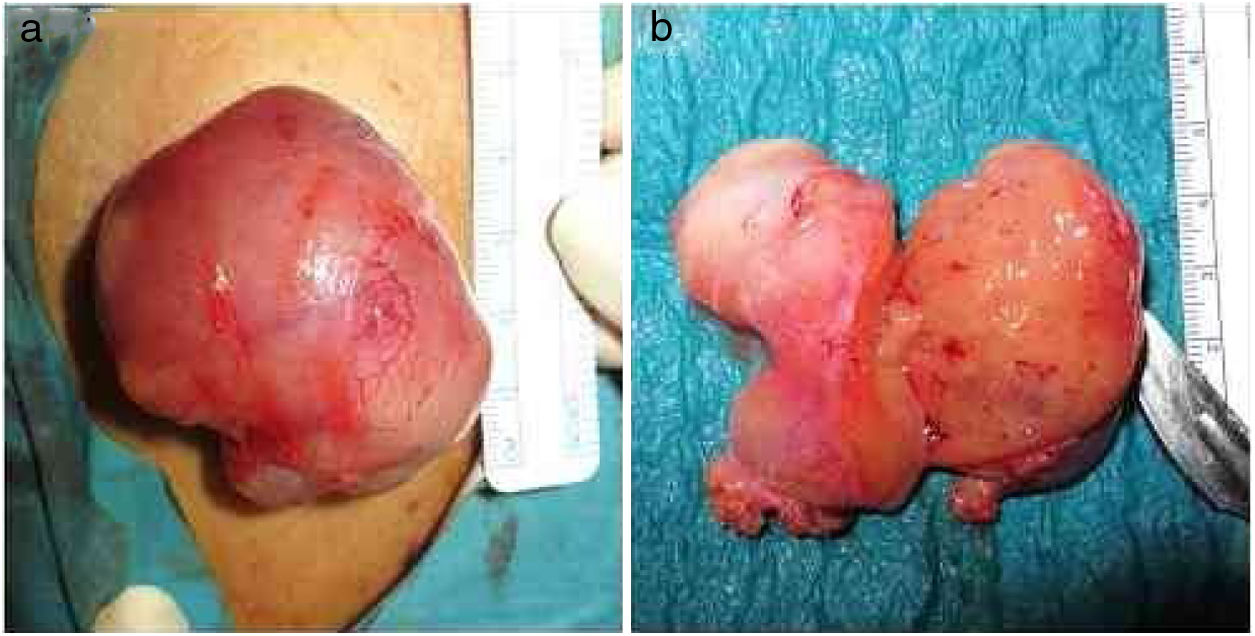
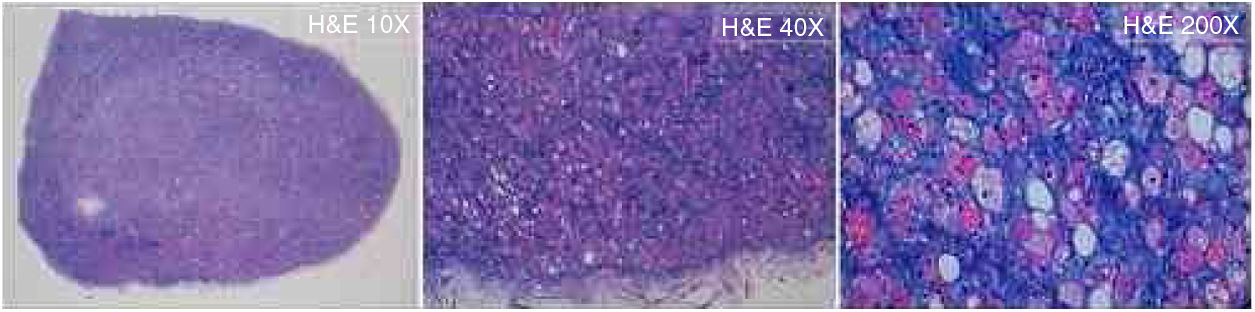
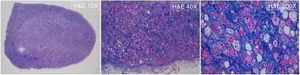
Considering this, we performed a complete surgical tumor resection, under local anesthesia, in an uneventful procedure (Fig. 2A). The tumor measured approximately 60×50×20mm, had a gelatinous external surface and, on section, showed a soft consistency and a brownish coloration (Fig. 2A and B). The histopathological examination revealed a hypodermic tumor, involved by a thin fibrous capsule, constituted by adipocytes with granular, eosinophilic cytoplasm, without cytologic atypia, numerous multi-vacuolated adipocytes and some uni-vacuolated cells, establishing the definite diagnosis of a hibernoma (Fig. 3). The patient recovered fully after surgery, without tumor recurrence after six months of follow-up.
Microscopic features of the tumor: The histopathological examination (hematoxylin & eosin: 10×, 40×, 200×) of the surgical specimen revealed a hypodermic tumor, involved by a thin fibrous capsule, constituted by adipocytes with granular, eosinophilic cytoplasm, without cytologic atypia, numerous multi-vacuolated adipocytes, and some uni-vacuolated cells, establishing the definitive diagnosis of hibernoma.
Hibernomas are rare, benign soft-tissue tumors arising from vestigial brown fat, which can be located in the subcutaneous tissue, the skeletal muscle, or the intermuscular fascia.1,2 There are four histological variants of hibernoma: typical (82%), myxoid (9%), lipoma-like (7%), and spindle-cell (2%).1 Hibernomas vary in size (1–24cm, average dimension 9.3cm) and location, occurring most commonly in the thigh, peri- and interscapular region, neck, arm, abdominal cavity, and retroperitoneum, and they are typically highly vascularized.1,3–5 They are most often diagnosed in adults (mean age 38 years).1
These lipomatous tumors generally present either as slow-growing, painless, soft, palpable and mobile masses, or as incidentalomas in imaging studies.1,3–5 Symptoms secondary to compression of adjacent structures can also develop due to their growth.1,3,4 Differential diagnosis is not always straightforward, and includes not only benign soft-tissue neoplasms (like atypical lipomas, hemangiomas, and angiolipomas) but also malignant, aggressive tumors (namely well-differentiated liposarcomas, myxoid liposarcomas, and rhabdomyosarcomas).1,2 In fact, hibernomas can mimic these other tumors clinically, imagiologically, and even histologically, considering some similar features in biopsy specimens.1–5
Histopathological examination of the tumor following complete surgical excision, which is curative, is essential for confirming the diagnosis.1,4,5
Author's contributionMargarida Moura Valejo Coelho: Approval of the final version of the manuscript; elaboration and writing of the manuscript; obtaining, analyzing and interpreting the data; effective participation in research orientation; intellectual participation in propaedeutic and/or therapeutic conduct of the case studied; critical review of the literature; critical review of the manuscript.
Alexandre João: Approval of the final version of the manuscript; obtaining, analyzing and interpreting the data; intellectual participation in propaedeutic and/or therapeutic conduct of the case studied; critical review of the manuscript.
Cândida Fernandes: Approval of the final version of the manuscript; obtaining, analyzing and interpreting the data; intellectual participation in propaedeutic and/or therapeutic conduct of the case studied; critical review of the manuscript.
Financial supportNone declared.
Conflicts of interestNone declared.
Please cite this article: Valejo Coelho MM, João A, Fernandes C. Hibernoma: case report of a rare lipomatous tumor. An Bras Dermatol. 2019;94:626–8.
Study conducted at the Department of Dermatology and Venereology, Centro Hospitalar Universitário de Lisboa Central, Lisbon, Portugal.