Dear Editor,
Frontal fibrosing alopecia (FFA) was first described by Kossard in 1994.1 Since then, case series have been described, the largest one in Spain.2
Most cases have slow progression and subsequent spontaneous stabilization. The progression may be evaluated by measuring frontotemporal recession.2,3
Here we describe a retrospective observational study, with data collected through medical records and a questionnaire applied to patients who were diagnosed with frontal fibrosing alopecia and monitored at the Dermatology Service of the Hospital de Clínicas of the Federal University of Paraná and at a private dermatological clinic. The study was approved by the Research Ethics Committee, protocol number 644.431. The patients authorized the use of their data and images.
The study assessed a total of 38 female patients. The mean age of participants was 61.1 years (38-84 years), and most of them had skin type 2 (76.31%), corroborating data found in the literature.2
The diagnosis was considered an examination finding in four (10.5%) patients. Among the 34 remaining patients, the mean time between disease onset and the correct diagnosis was 3 years (0-10 years).
At onset of the disease, 10 (26.31%) patients were premenopausal, 28 (73.68%) patients were postmenopausal, and 16 (42.1%) patients had undergone hormone replacement therapy prior to FFA diagnosis. The mean onset of the disease was 44 years in the premenopausal group and 59 years and 7 months in the postmenopausal group.
Thirty-three (86.84%) patients reported frequent application of chemical treatments (hair dye or straightening) to their hair. Fifteen (39.47%) patients reported routine use of sunscreen, 8 (21,05%) of whom used it at least once a month.
Ten (26.31%) patients reported maternal history of alopecia, and 16 (42.1%) patients reported paternal history. One patient referred to a daughter with FFA, and another patient reported a daughter with cutaneous lichen planus.
All patients had frontotemporal hairline recession (Figure 1), three of whom also had nonscarring diffuse hair loss, and one also presented occipital hairline recession. Only four patients presented patches of cicatricial alopecia in a lichen planopilaris (LPP) pattern.
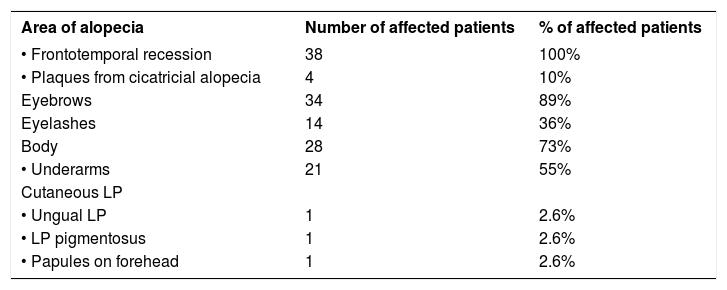
Table 1 shows the clinical presentations in our patients. Only one patient had frontal facial papules histopathologically confirmed, despite six of them presenting it clinically.
Sites of alopecia and other clinical presentations in our patients
| Area of alopecia | Number of affected patients | % of affected patients |
|---|---|---|
| • Frontotemporal recession | 38 | 100% |
| • Plaques from cicatricial alopecia | 4 | 10% |
| Eyebrows | 34 | 89% |
| Eyelashes | 14 | 36% |
| Body | 28 | 73% |
| • Underarms | 21 | 55% |
| Cutaneous LP | ||
| • Ungual LP | 1 | 2.6% |
| • LP pigmentosus | 1 | 2.6% |
| • Papules on forehead | 1 | 2.6% |
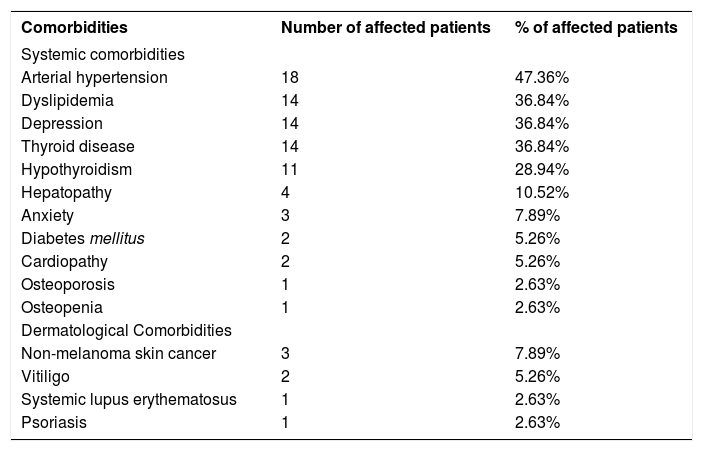
Table 2 shows the comorbidities presented by the patients. Six (15,78%) patients referred to facial plastic surgery concomitant with the onset of FFA.
Systemic and skin comorbidities in our patients
| Comorbidities | Number of affected patients | % of affected patients |
|---|---|---|
| Systemic comorbidities | ||
| Arterial hypertension | 18 | 47.36% |
| Dyslipidemia | 14 | 36.84% |
| Depression | 14 | 36.84% |
| Thyroid disease | 14 | 36.84% |
| Hypothyroidism | 11 | 28.94% |
| Hepatopathy | 4 | 10.52% |
| Anxiety | 3 | 7.89% |
| Diabetes mellitus | 2 | 5.26% |
| Cardiopathy | 2 | 5.26% |
| Osteoporosis | 1 | 2.63% |
| Osteopenia | 1 | 2.63% |
| Dermatological Comorbidities | ||
| Non-melanoma skin cancer | 3 | 7.89% |
| Vitiligo | 2 | 5.26% |
| Systemic lupus erythematosus | 1 | 2.63% |
| Psoriasis | 1 | 2.63% |
Thirty-five patients had a mean follow-up time of 2 years and six months (0-11 years). Regarding therapy, 34 (89.47%) patients were administered topical (topical steroids and minoxidil), and 33 (86.84%) patients received systemic treatment (27 with antimalarials, 17 with 5α-reductase inhibitors (finasteride), and only four with methotrexate, cyclosporine and mycophenolate mofetil). In this group, 20 patients reported stabilization, six experienced worsening of the disease, and nine presented regrowth.
The involvement of the eyebrows occurred in 34 (89.47%) patients, also concordant with the literature data.2,3,4 Fourteen referred to eyelash loss, and 28 reported body hair involvement, a higher proportion than that found in the literature.4 One case series included patients presenting non-cicatricial involvement of peripheral body hair, all histopathologically confirmed.5 This suggests that AFF can be considered as a generalized hair loss process not restricted to the scalp.
Despite the limitations of the study, it is possible to confirm the predominance of postmenopausal women among those affected, and we observed some benefit of the treatments in the interruption of the disease's evolution. The frequency of involvement of eyebrows and other body hair should be noted. An association with cutaneous lichen planus in other areas of the body was rare.
The study suggested that the use of hair dye (33 patients; 86.84%) could be included as a risk factor for FFA, and laboratory tests of thyroid function should be requested in patients with FFA.