Schnitzler Syndrome (SchS) is a rare disorder, with ∼350 cases reported in the literature, characterized by a neutrophilic urticarial dermatosis and monoclonal gammopathy (IgM in more than 90% of the cases), associated with clinical and biological signs of inflammation.1–3 In 2013, Lipsker, Schnitzler, and other experts met and proposed the Strasbourg diagnostic criteria, which are widely used today to diagnose SchS (Table 1).1,4 We report a case of a man with a clinical and laboratory diagnosis of SchS in Brazil.
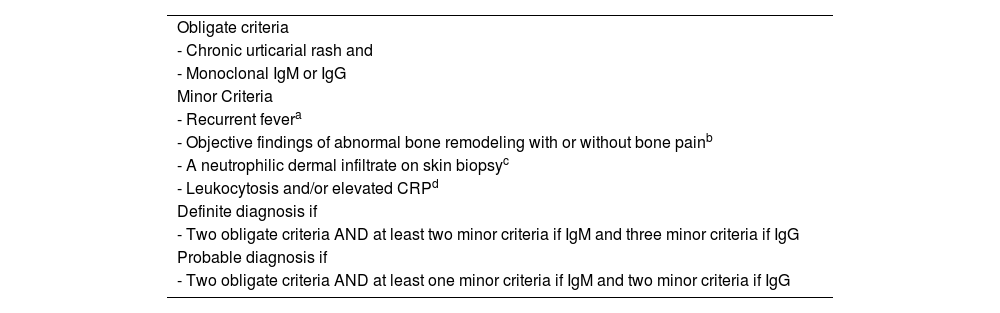
Strasbourg diagnostic criteria of Schnitzler syndrome.
| Obligate criteria |
| - Chronic urticarial rash and |
| - Monoclonal IgM or IgG |
| Minor Criteria |
| - Recurrent fevera |
| - Objective findings of abnormal bone remodeling with or without bone painb |
| - A neutrophilic dermal infiltrate on skin biopsyc |
| - Leukocytosis and/or elevated CRPd |
| Definite diagnosis if |
| - Two obligate criteria AND at least two minor criteria if IgM and three minor criteria if IgG |
| Probable diagnosis if |
| - Two obligate criteria AND at least one minor criteria if IgM and two minor criteria if IgG |
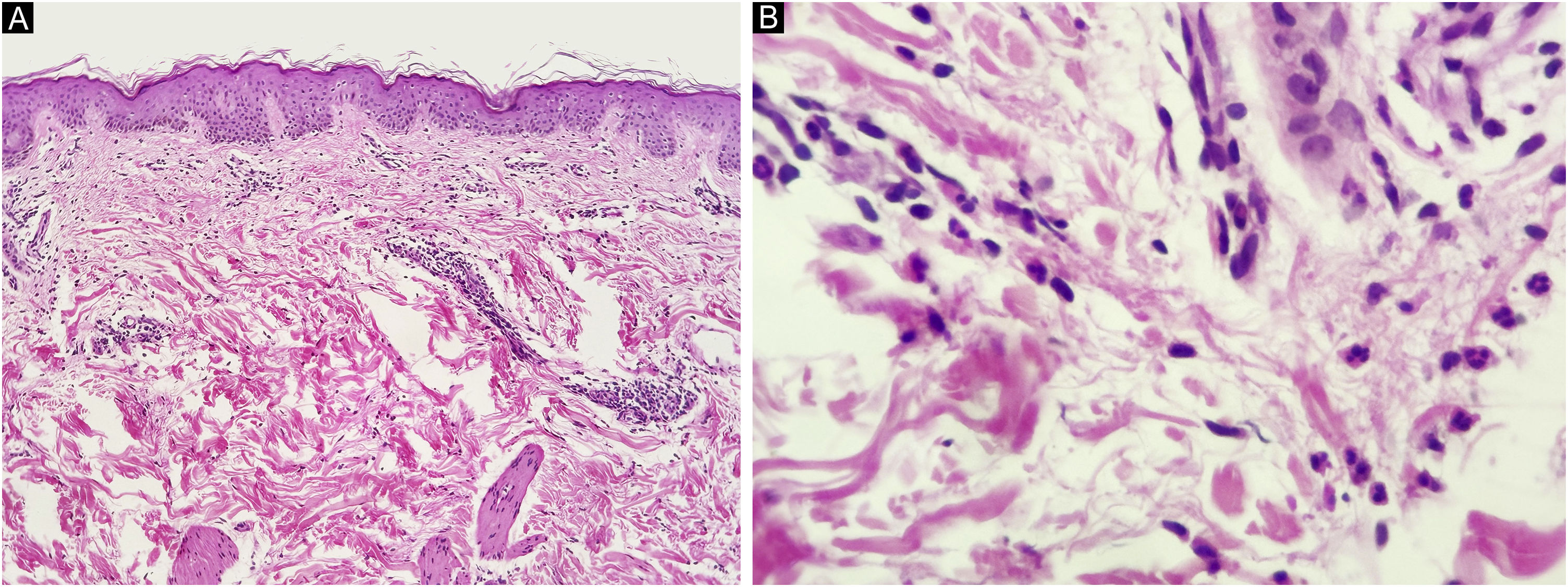
A 67-year-old man presented to our department with recurrent pruritic, not painful, urticaria-like lesions on the extremities and the trunk (Fig. 1). The lesions resolved within 24 hours without leaving behind dusky hyperpigmentation. He had intermittent fever of up to 39 °C, generalized arthralgia, and fatigue. The inflammatory episodes lasted for 2–5 days with severe general impairment. The patient suffered outbreaks with variable intensity on almost a monthly basis over the past fifteen years. Histopathology of lesional skin showed a perivascular and interstitial polymorphonuclear infiltrate, described as consistent with the diagnosis of urticarial lesions and compatible with SchS (Fig. 2).
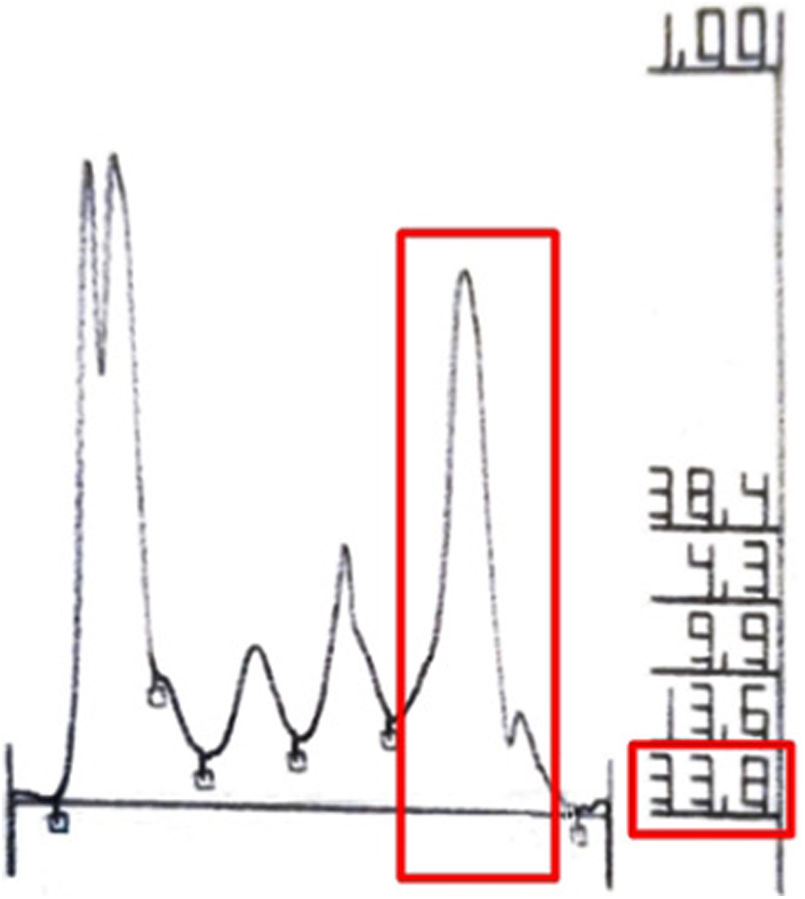
Laboratory investigations revealed leucocytosis (up to 21.000 mm3, ref 4000–11600 mm3), an elevated ESR (120 mm/hr; 0∼20 mm/hr), and increased IgM levels (2550 mg/dL; 46∼260 mg/dL) in serum protein electrophoresis (Fig. 3). In the bone scan, there is a slight asymmetry of uptake in the tibias, slightly greater on the left. Bone marrow biopsy was performed with a negative cytogenetic study for lymphoproliferative diseases. Based on these clinical and laboratory findings, he was diagnosed with Schnitzler Syndrome.
He was started on a high-dose corticosteroid, NSAIDs, and antihistamines with partial remission of his symptoms.
There are a few cases reported in Latin America and in general, it is underdiagnosed despite the well-established diagnostic criteria, but the pathogenesis is unknown.5
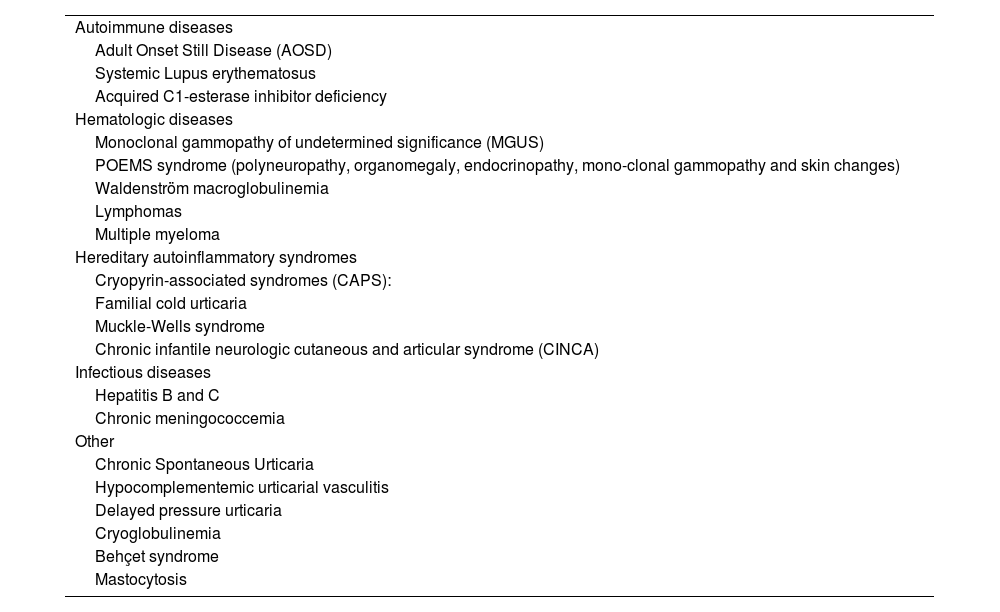
The major complication is hematological malignancy, with lymphoproliferative disorder occurring in about 10%‒20% of patients.5,6 In addition to chronic spontaneous urticaria, other differential diagnoses should be considered (Table 2).7
Differential diagnoses of Schnitzler syndrome.
| Autoimmune diseases |
| Adult Onset Still Disease (AOSD) |
| Systemic Lupus erythematosus |
| Acquired C1-esterase inhibitor deficiency |
| Hematologic diseases |
| Monoclonal gammopathy of undetermined significance (MGUS) |
| POEMS syndrome (polyneuropathy, organomegaly, endocrinopathy, mono-clonal gammopathy and skin changes) |
| Waldenström macroglobulinemia |
| Lymphomas |
| Multiple myeloma |
| Hereditary autoinflammatory syndromes |
| Cryopyrin-associated syndromes (CAPS): |
| Familial cold urticaria |
| Muckle-Wells syndrome |
| Chronic infantile neurologic cutaneous and articular syndrome (CINCA) |
| Infectious diseases |
| Hepatitis B and C |
| Chronic meningococcemia |
| Other |
| Chronic Spontaneous Urticaria |
| Hypocomplementemic urticarial vasculitis |
| Delayed pressure urticaria |
| Cryoglobulinemia |
| Behçet syndrome |
| Mastocytosis |
At present, for patients with CRP < 3 mg/dL, treatment options include, colchicine, Nonsteroidal Anti-inflammatory Drugs (NSAIDs), and hydroxychloroquine.1,2 Corticosteroids has a moderate effect and antihistamine therapy has no effect.8 According to Simon et al., the efficacy of colchicine is only 25%, but based on the benefit/risk ratio, colchicine is recommended as the first choice of treatment.9 Experts recommend the use of anakinra (IL-1 block) in more symptomatic patients, such as Erythrocyte Sedimentation Rate (ESR) and CRP above the upper limit of normal (CRP > 3 mg/dL).1
Treatment with corticosteroids, NSAIDs, and antihistamines is symptomatic and unsatisfactory.9 Anakinra (IL-1-neutralizing) is the choice drug. The effect of inhibition of IL-1 has led to new expectations, but there is currently unavailable in Brazil. An alternative drug could be canakinumab, a human anti-IL-1β monoclonal antibody aiming at the neutralization of 1β signaling.10
In patients presenting with chronic urticaria associated with signs of systemic inflammation, this rare and debilitating syndrome should be considered. Early treatment can improve patient's quality of life and disease prognosis.
Financial supportNone declared.
Authors’ contributionsKelielson Cardoso de Macêdo Cruz: Preparation and writing of the manuscript; intellectual participation in propaedeutic and/or therapeutic management of studied cases; approval of the final version of the manuscript; critical literature review.
Daniela de Abreu e Silva Martinez: Preparation and writing of the manuscript; approval of the final version of the manuscript.
Danielle Carvalho Quintella: Preparation and writing of the manuscript; approval of the final version of the manuscript.
Tullia Cuzzi: Preparation and writing of the manuscript; approval of the final version of the manuscript.
Sergio Duarte Dortas Junior: Preparation and writing of the manuscript; intellectual participation in propaedeutic and/or therapeutic management of studied cases; approval of the final version of the manuscript.
Solange Oliveira Rodrigues Valle: Preparation and writing of the manuscript; intellectual participation in propaedeutic and/or therapeutic management of studied cases; approval of the final version of the manuscript.
Conflicts of interestNone declared.
Study conducted at the Hospital Universitário Clementino Fraga Filho, Universidade Federal do Rio de Janeiro, Rio de Janeiro, RJ, Brazil.