Lupus miliaris disseminatus faciei (LMDF) predominantly occurs at 20–30 years of age and is rarely seen in children. We report a pediatric case of LMDF affecting the face and the labia majora.
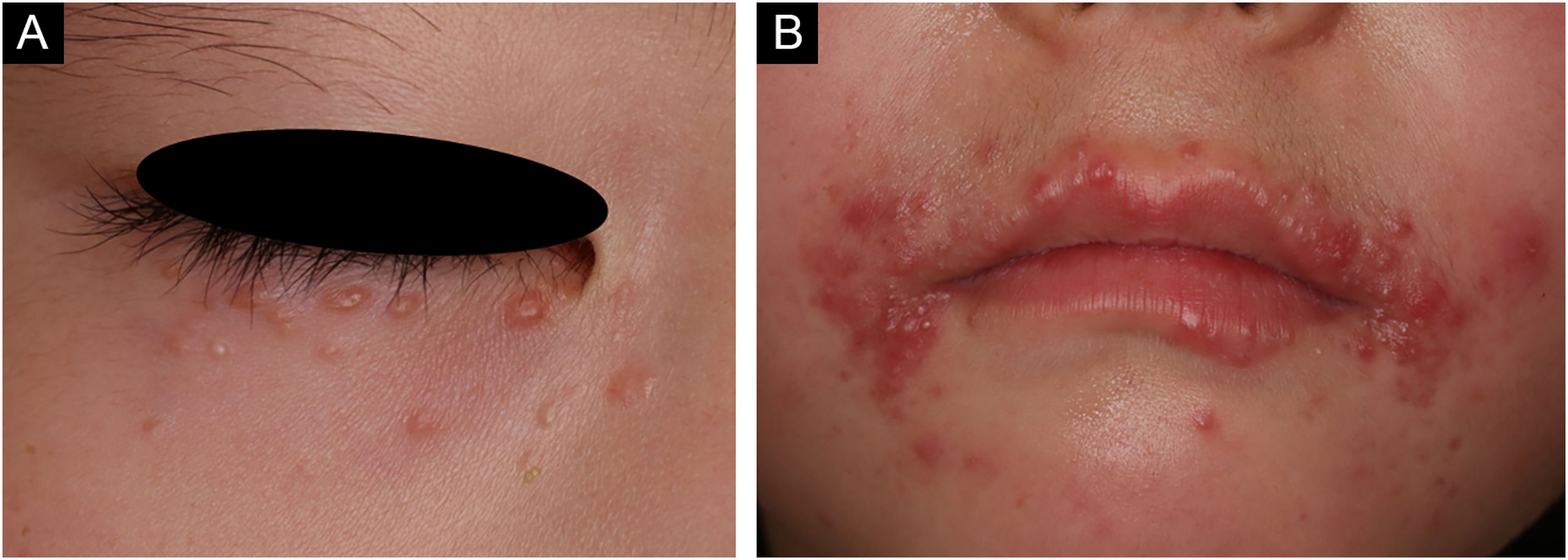
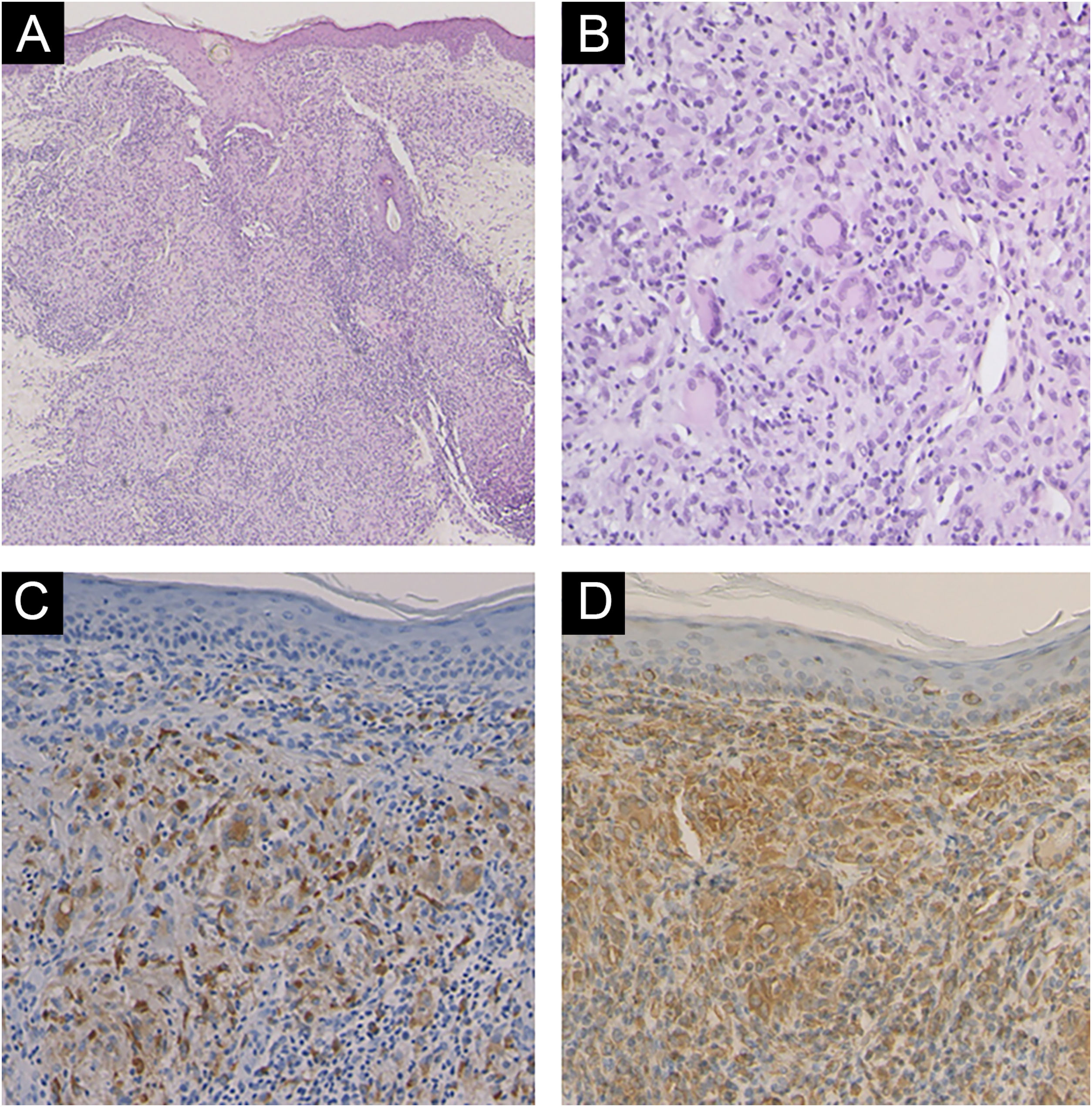
A 6-year-old Japanese girl was referred to our department, complaining of a 5-month history of pruritic papular eruptions on the face. She had been treated with oral antiallergic drugs and topical corticosteroids, but without effects. Physical examination showed numerous 1‒2 mm dome-shaped small reddish papulonodules around the mouth and lower eyelids (Fig. 1 A and B). In addition, reddish papules were scattered in the labia majora (Fig. 2). A skin biopsy was carried out from papular eruptions on the right jaw. Histological examination revealed dermal epithelioid cell granulomas without caseous necrosis (Fig. 3A). Magnified epithelioid cell granuloma images showed multinucleated giant cells in the dermis (Fig. 3B), as well as inflammatory lymphocytic and histiocytic infiltration around the granulomas and hair follicles area. Immunostaining was positive for CD68 and CD163 antigens (Fig. 3 C and D). A tuberculin test was negative. Treatment with oral administration of clarithromycin showed favorable effects on the vulvar lesions after 5 months and the facial lesions after 9 months.
The present case developed multiple palpebral and perioral papulonodular lesions, which are the frequently involved sites of LMDF. In addition, vulvar involvement was observed. The patient did not have any organ symptoms suggestive of juvenile-onset sarcoidosis. Granulomatous rosacea was excluded, because neither facial erythema nor telangiectasia was observed, and the patient denied flushing.
Clinical and pathological features of pediatric LMDF are slightly different from adult LMDF, such as i) Papules concentrated around the mouth, on the nasolabial fold, and on the lower eyelids, ii) Small papule size, iii) Few pustules and scarring, iv) Redness around the mouth, v) Few caseous necrosis within epithelioid granulomas, and vi) Short clinical course.1 On the other hand, Childhood Granulomatous Periorificial Dermatitis (CGPD) was reported as a disease in which yellow-brown papular eruptions limited to the perioral, perinasal, and periocular regions that histopathologically show epithelioid cell granulomas around hair follicles.2 The features of LMDF in childhood are highly similar to those of CGPD, and differentiation of both disorders is challenging and possibly both disorders are the same entity.1
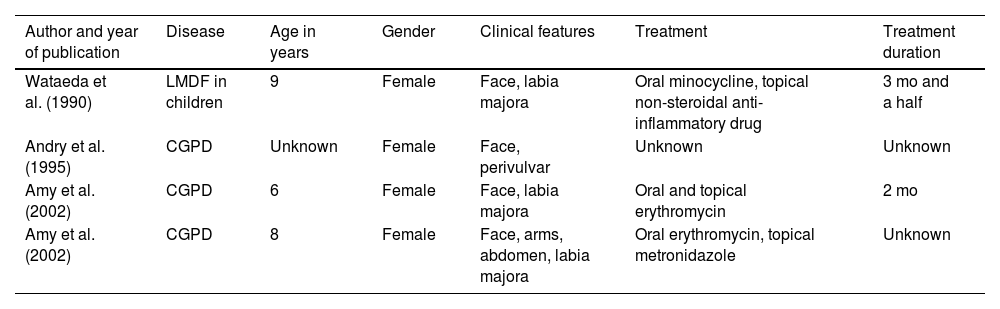
There are several cases of LMDF with extra-facial involvement in sites such as the neck, axilla, groin, and extremities. Genital regions are also affected, and to our knowledge, there are only four reported cases of this involvement in childhood LMDF (1 case) and CGPD (3 cases) (Table 1).3,4 The age of onset was 6–9 years, and all cases were girls. They were successfully treated with oral minocycline, topical non-steroidal anti-inflammatory drugs, oral and topical erythromycin, topical metronidazole, topical tacrolimus, and topical metronidazole.4,5 Treatment response is better in pediatric LMDF than in adult cases. In pediatric cases of LMDF, genital areas should be examined in detail.
Cases of vulvar involvement in childhood Lupus miliaris disseminatus faciei and childhood granulomatous periorificial dermatitis.
| Author and year of publication | Disease | Age in years | Gender | Clinical features | Treatment | Treatment duration |
|---|---|---|---|---|---|---|
| Wataeda et al. (1990) | LMDF in children | 9 | Female | Face, labia majora | Oral minocycline, topical non-steroidal anti-inflammatory drug | 3 mo and a half |
| Andry et al. (1995) | CGPD | Unknown | Female | Face, perivulvar | Unknown | Unknown |
| Amy et al. (2002) | CGPD | 6 | Female | Face, labia majora | Oral and topical erythromycin | 2 mo |
| Amy et al. (2002) | CGPD | 8 | Female | Face, arms, abdomen, labia majora | Oral erythromycin, topical metronidazole | Unknown |
None declared.
Authors’ contributionsMisaki Kusano: Approval of the final version of the manuscript; critical literature review; data collection; analysis and interpretation; study conception and planning; management of studied cases; manuscript critical review; preparation and writing of the manuscript.
Maki Takada: Approval of the final version of the manuscript; critical literature review; manuscript critical review; preparation and writing of the manuscript.
Natsuko Matsumura: Approval of the final version of the manuscript; critical literature review; manuscript critical review; preparation and writing of the manuscript.
Toshiyuki Yamamoto: Approval of the final version of the manuscript; critical literature review; data collection; analysis and interpretation; study conception and planning; manuscript critical review; preparation and writing of the manuscript.
Conflicts of interestNone declared.
Study conducted at the Fukushima Medical University, Fukushima, Japan.