Fox-Fordyce disease is a relatively infrequent pathology of the apocrine glands that affects almost exclusively young women. The disease is characterized by the presence of pruritic follicular papules mainly in the armpits that respond poorly to treatment and severely affect the patient’s quality of life. We report two cases with clinical diagnosis and histopathological confirmation, presenting perifollicular xanthomatosis on histological examination, recently described as a distinctive, consistent, and specific feature of this disease.
Fox-Fordyce disease (FFD), also known as apocrine miliaria or chronic pruritic papular eruption of the pubis and armpits, affects areas where apocrine glands are found predominantly, such as the pubic, axillary, and anogenital regions.1,2 The pathogenesis remains unknown, and the disease affects primarily young women.3 Commonly used treatments are poorly or partially effective, as the lesions frequently recur and the symptoms persist.
We present two cases with both clinical and histopathological diagnosis of perifollicular xanthomatosis.
Case ReportsCASE 1A 33-year-old female patient, resident of Mexico City, previously healthy, reported a one-month history of multiple mildly pruritic papules in both armpits. Patient reported hyperhidrosis and no prior treatment.
Physical examination showed localized, bilateral, asymmetric alterations affecting both axillae, more prominently on the left, characterized by yellowish-brown punctate papules 1 mm in diameter with a smooth uniform surface and follicular distribution (Figure 1).
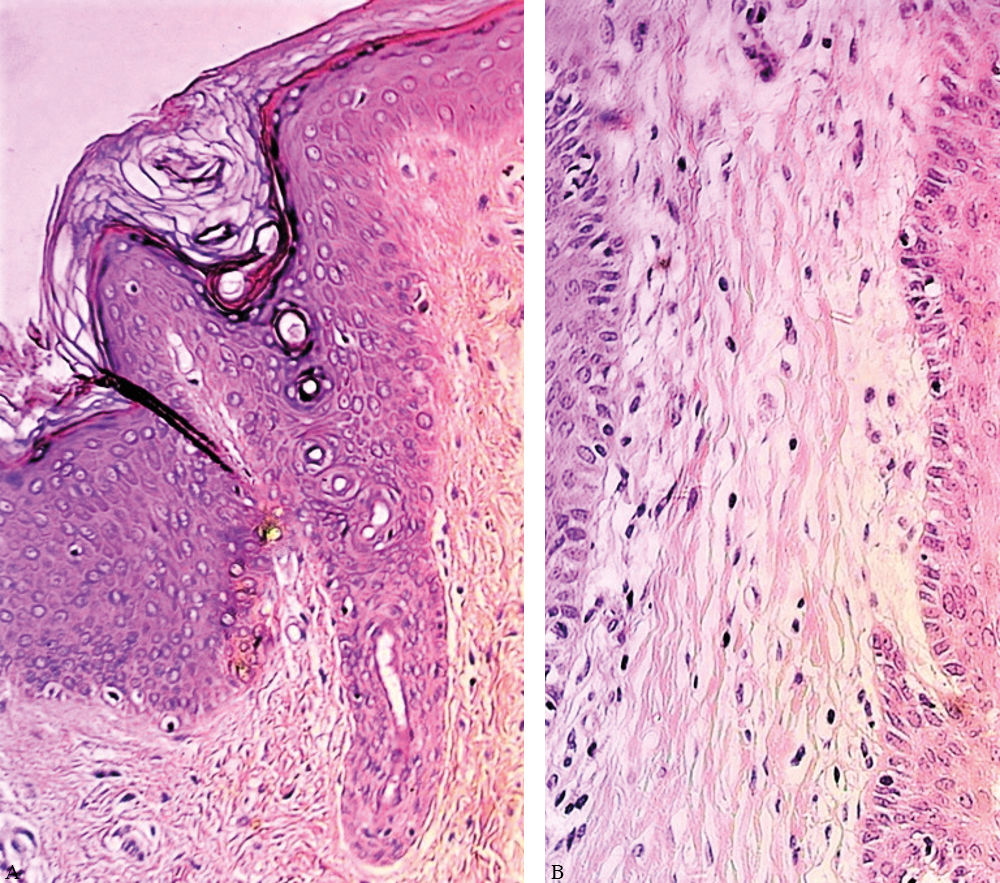
Histopathological examination with H&E staining showed dilation of the follicular infundibulum with corneal plug, as well as inflammatory lymphohistiocytic infiltrate with xanthomatous cells surrounding the infundibulum (Figure 2). Intrafollicular and apocrine gland mucin deposits were observed with Alcian blue staining.
Immunohistochemistry showed perifollicular cells strongly positive for CD68. Carcinoembryonic antigen and epithelial membrane antigen were negative in the xanthomatous cells (Figure 3).
FFD was confirmed and topical clindamycin was initiated, with improvement of the symptoms.
Case 2A 24-year-old female patient, resident of León, Guanajuato, Mexico, presented intensely pruritic papules in both armpits and the genital area with two years’ evolution. Patient had received prior treatment with antihistamines and emollients with no improvement. Patient reported that other females in her family had presented this skin condition in the armpits, although less severe.
Patient had a 12-year history of comedogenic acne on the face and trunk as well as menstrual alterations with amenorrhea of up to 2 months. Therefore, pelvic ultrasound was ordered, showing polycystic ovaries.
Physical examination showed a disseminated dermatological condition affecting the axillae and genitalia, in hairy areas, characterized by skin-colored punctate papules 1 to 2 mm in diameter with follicular distribution and some crusts (Figure 4).
Histopathology showed dilated follicular infundibula with hyperkeratosis, as well as xanthomatous histiocytes with perifollicular distribution and discrete inflammatory lymphocytic infiltrate. Intrafollicular mucin deposits were also observed (Figure 5).
FFD was diagnosed, and combined oral contraceptives (cyproterone with ethinylestradiol) and topical hydrocortisone were prescribed, with partial improvement of lesions and pruritus.
DiscussionFox-Fordyce disease was first described in 1902 by American authors George Henry Fox and John Addison Fordyce.1,2 The pathogenesis of this condition remains unknown, although proposed theories suggest that hormonal factors, hair removal, and inheritance may be involved in the apocrine obstruction, sweat retention, and inflammation.3,4
This disease entity presents characteristic clinical data, affecting areas of the body where apocrine glands are found, such as armpits, pubis, and the anogenital region. However, less frequent locations on the thorax, areolas, abdomen, and legs have been described.5 The disease occurs mainly in women 15 to 35 years of age and usually remits in menopause.6 In the current cases, we report typical lesions affecting the axillary region and genitals, with no lesions on other parts of the body surface. Both patients were childbearing-age women.
Clinically, FFD is characterized by the presence of multiple skin-colored follicular papules, slightly yellowish or brown, dome-shaped, with a smooth surface, which may be accompanied by mild to moderate pruritus or even be asymptomatic. Exacerbating symptoms include heat, moisture, physical activity, friction with clothing, and excessive sweating.7 Laser hair removal and intense pulsed light have also been described as triggers.4,8 The lesions tend to display chronic evolution, described as lasting weeks to years.7
Differential diagnoses include Graham-Little-Piccardi-Lasseur syndrome, trichostasis spinulosa, Darier’s disease, syringomas, lichen nitidus, lichen amyloid, and papular mucinosis.9,10
Definitive diagnosis is made by histopathological examination in which nonspecific findings such as intrafollicular corneal plug, hyperkeratosis, spongiosis, retention vesicles, glandular dilation with mucin deposits, and perifollicular lymphohistiocytic inflammatory infiltrate can be observed.11,12 The presence of infundibular dyskeratotic cells, vacuolar changes, and parakeratosis similar to cornoid lamella have also been described.13 However, Bormate et al. recently described the presence of foamy or xanthomatous histiocytes (perifollicular xanthomatosis) as a distinctive, consistent, and more specific feature of this pathology.13 This was corroborated in the histopathology of our cases, as both presented the previously described findings and xanthomatous histiocytes as well as the presence of intrafollicular mucin.
Treatment response tends to be limited or partial; the lesions and symptoms may recur or persist. First-line treatments include topical and oral retinoids, benzoyl peroxide, topical calcineurin inhibitors, clindamycin, intralesional or topical steroids, and oral contraceptives, the latter reported with complete resolution of lesions.14 In our first case, the patient was treated with topical clindamycin, achieving partial improvement of the lesions and symptoms. In the second case, the patient was treated with combined oral contraceptives and topical hydrocortisone, achieving partial improvement of lesions and pruritus.
Alternative therapies as second-line treatment or in severe cases, such as botulinum toxin, phototherapy, electrocoagulation, copper vapor and CO2 laser, liposuction, curettage, and microwave have been described with favorable results.10,15
We have reported two cases here, both with perifollicular xanthomatosis on histology, supporting the position that this is the most specific and distinctive feature of this relatively rare disease.
Financial Support: None.
Conflict of Interest: None.