Hyperzincemia and hypercalprotectinemia is a rare inflammatory disease caused by a mutation in the PSTPIP1 gene, with a dysregulation of calprotectin metabolism. Calprotectin is a zinc-binding protein with antimicrobial properties and pro-inflammatory action. The authors report the case of a 20 year-old girl with cutaneous ulcers comparable with pyoderma gangrenosum, growth failure and chronic anemia, who was given the diagnosis of hyperzincemia and hypercalprotectinemia. Measurement of serum zinc and calprotectin concentrations are indicated in these cases.
Hyperzincemia and hypercalprotectinemia (Hz/Hc) is an autoinflammatory disorder characterized by chronic systemic inflammation, cutaneous lesions, arthralgia/arthritis, hepatosplenomegaly, pancytopenia, and growth failure, first described in 1985.1 The cause of this disease is related to a mutation in the proline-serine-threonine phosphatase-interacting protein 1 (PSTPIP1) gene, leading to dysregulation of the metabolism of calprotectin. This protein has zinc-binding capacity, as well as antimicrobial and proinflammatory activity. The literature presents few cases, and even fewer describe the dermatological aspects; furthermore, none of them are from Latin America (Tables 1 and 2).2–4
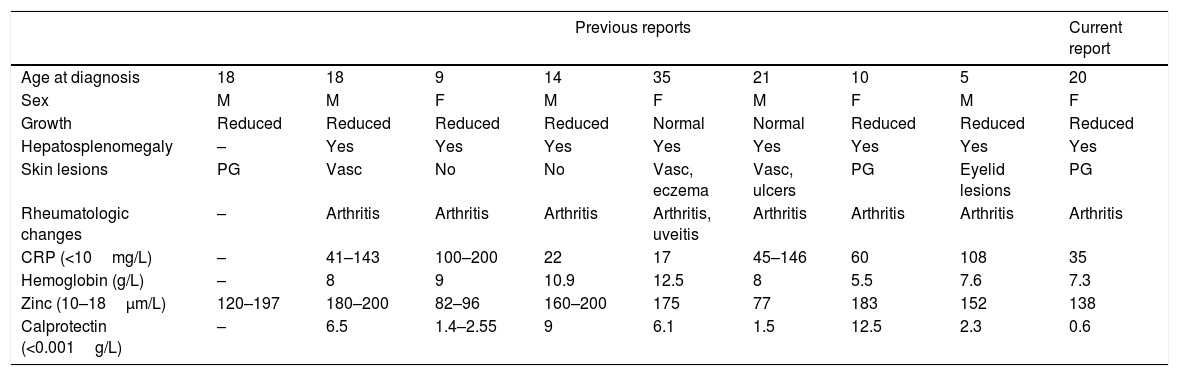
Reports of Hz/Hc cases described in the literature with dermatological evaluation.1,3,4
| Previous reports | Current report | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Age at diagnosis | 18 | 18 | 9 | 14 | 35 | 21 | 10 | 5 | 20 |
| Sex | M | M | F | M | F | M | F | M | F |
| Growth | Reduced | Reduced | Reduced | Reduced | Normal | Normal | Reduced | Reduced | Reduced |
| Hepatosplenomegaly | – | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Skin lesions | PG | Vasc | No | No | Vasc, eczema | Vasc, ulcers | PG | Eyelid lesions | PG |
| Rheumatologic changes | – | Arthritis | Arthritis | Arthritis | Arthritis, uveitis | Arthritis | Arthritis | Arthritis | Arthritis |
| CRP (<10mg/L) | – | 41–143 | 100–200 | 22 | 17 | 45–146 | 60 | 108 | 35 |
| Hemoglobin (g/L) | – | 8 | 9 | 10.9 | 12.5 | 8 | 5.5 | 7.6 | 7.3 |
| Zinc (10–18μm/L) | 120–197 | 180–200 | 82–96 | 160–200 | 175 | 77 | 183 | 152 | 138 |
| Calprotectin (<0.001g/L) | – | 6.5 | 1.4–2.55 | 9 | 6.1 | 1.5 | 12.5 | 2.3 | 0.6 |
PG, pyoderma gangrenosum; Vasc, vasculitis; CRP, C-reactive protein.
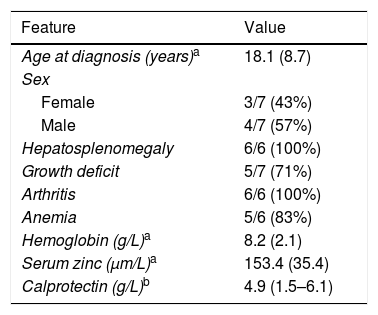
Summary of clinical characteristics of the cases of Hz/Hc with reported cutaneous lesions.
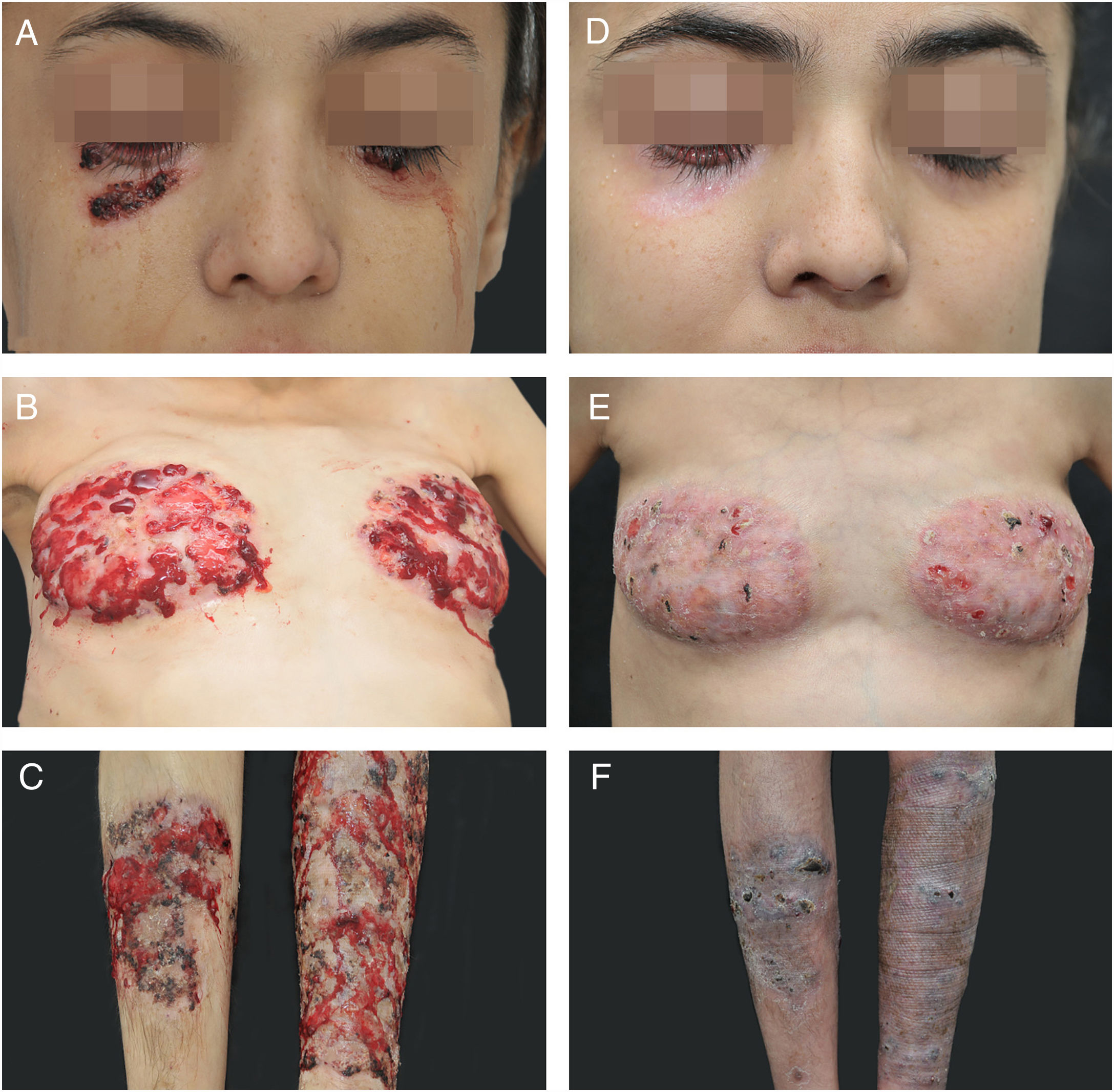
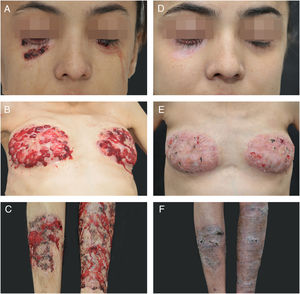
A 20 year-old woman reported persistent ulcerated skin lesions with variable severity for five years, recurrent abdominal pain with episodes of diarrhea and joint pain in both knees accompanied by edema and local erythema since childhood. She reported chronic anemia that was unresponsive to several treatments. On the physical examination, the patient had short stature (percentile<3%), cutaneous ulcerations with violaceous edges, interspersed by scar tissue and pustules with friable, bleeding and granular central area, together with the presence of purulent exudate and hematic crusts, affecting both lower eyelids, breast, and legs, in addition to a pronounced hepatosplenomegaly (Fig. 1A–C). The histopathological examination of the skin lesions was nonspecific, but compatible with pyoderma gangrenosum (PG). Initial investigations revealed pancytopenia, inversion of the albumin/globulin pattern (0.55; normal: 1.9–1.63), elevated C-reactive protein (CRP=35; normal<10mg/L) and hepatosplenomegaly on ultrasonography, which also evidenced preserved parenchyma with extramedullary hematopoiesis in the liver biopsy histopathologic analysis. The patient also had portal hypertension with esophageal varices and pronounced osteoporosis, with a pathological T12.
Considering the diagnostic hypothesis of Hz/Hc, serum levels of zinc and calprotectin were measured: 869μg/L (normal 70–120μg/L) and 642μg/L (normal<1.6μg/L), respectively.
Cyclosporin A (3.5mg/kg/day) and prednisolone (1.5mg/kg/day) were initiated, leading to wound healing, weight gain, and partial improvement of anemia, but the therapeutic response worsened after an attempt of waning, evolving with aggravation of preexisting lesions and development of an ulcerated lesion in the point of transcutaneous hepatic biopsy, compatible with pathergy (Fig. 1D–F). Immunosuppressive levels were restored, including a biweekly infusion of adalimumab 40mg, with a significant but partial improve in the cutaneous lesions.
In the genetic assessment of the patient, the c.748G>A variant (Glu250Lys) was found in heterozygosis in the exon 1 of the PSTPIP1 gene. This variant is constituted by a substitution of glutamic acid for lysine at the codon 250 of the translated protein, which has been described as pathogenic in the Infervers and Clinvar databases (rs28939089) when associated with pyogenic arthritis, PG, and acne (PAPA) syndrome (MIM 604416).
DiscussionHz/Hc is a rare autoinflammatory condition, clinically characterized by pustular and ulcerative inflammatory cutaneous lesions, recurrent arthritis, hepatosplenomegaly, pancytopenia, and growth failure, with no predilection for gender, and usually diagnosed during youth. The disease is characterized by laboratory findings, such as extremely high serum levels of zinc and mostly calprotectin (500–12,000 times the normal levels).3
Calprotectin is formed by a complex of two MRP8/14 proteins that are endogenous activators of the toll-like receptor 4 (TLR-4) and belong to the family of the alarmins. This protein is found in the neutrophil cytosol and has intense pro-inflammatory properties.5,6 Recently, a specific mutation resulting in a single amino acid substitution in the gene of the PSTPIP1 protein, a cytoskeleton-associated protein that modulates T-cell activation and IL-1b release, has been identified in these patients. Other mutations in this same gene had already been associated with other autoinflammatory diseases, such as PAPA syndrome, that has clinical similarities with Hz/Hc, but none of them present high levels of calprotectin and zinc.2
To date, no treatment has been fully effective, with reports of the use of corticosteroids, cyclosporine, tacrolimus, TNF, and IL-1 inhibitors. Hz/Hc is a chronic multisystem disease with nonspecific symptomatology and is present since childhood in most cases.2,4–7 Extremely high levels of serum zinc and calprotectin are strongly suggestive of the diagnosis; therefore, in suspected cases, serum level assessments should be considered.
The skin changes reported in Hz/Hc are vasculitis, eczemas, furuncle-like ulcers, and necrotic lesions. They tend to be inflammatory and ulcerated, sometimes pruritic, with clinical and histopathologic similarities to PG, usually affecting the lower limbs symmetrically, with reports of facial lesions, particularly on the eyelids. The observation of chronic lesions in young children and adults with hepatosplenomegaly, arthralgia/arthritis, high CRP, and microcytic anemia is suggestive of Hz/Hc.
Financial supportNone declared.
Author's contributionLudimila Oliveira Resende: Elaboration and writing of the manuscript.
Marilia Formentini Scotton Jorge: Elaboration and writing of the manuscript; intellectual participation in propaedeutic and/or therapeutic conduct of the cases studied.
Juliano Vilaverde Schmitt: Effective participation in research orientation; intellectual participation in propaedeutic and/or therapeutic conduct of the cases studied.
Conflicts of interestNone declared.
How to cite this article: Resende LO, Jorge MFS, Schmitt JV. Extensive pyoderma gangrenosum-like lesions revealing a case of hyperzincemia and hypercalprotectinemia: when to suspect it? An Bras Dermatol. 2019;94:713–6.
Study conducted at the Hospital das Clínicas, Faculdade de Medicina de Botucatu, Universidade Estadual Paulista, Botucatu, SP, Brazil.