We report the case of a 47-year-old male patient with S100 negative granular cell tumor of the oral cavity, focusing on dermoscopic features as well as surgical approach, not previously reported in the literature. The study contributes to the literature on dermoscopy and surgical treatment for this tumor and provides a practical approach to differentiating non-neural granular cell tumors and granular cell tumors.
Granular cell tumors (GCT), also known as Abrikossoff tumors, are uncommon benign neoplasms probably derived from Schwann cells. They are usually located in the oral mucosa, specifically the tongue.1 Non-neural granular cell tumor (NNGCT) is a rare and recently described tumor. Only five cases have been reported with involvement of the oral mucosa, with no reports of dermoscopy or surgical treatment. The current case report contributes to the literature on dermoscopy and surgical management of this tumor and provides a practical approach to differentiating between non-neural granular cell tumors and granular cell tumors.
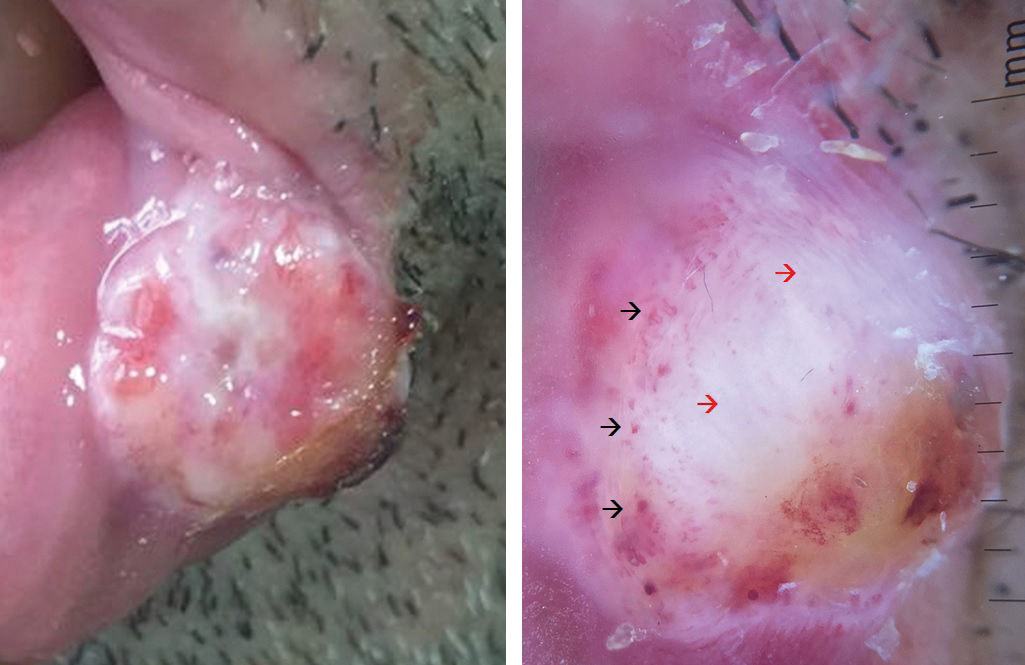
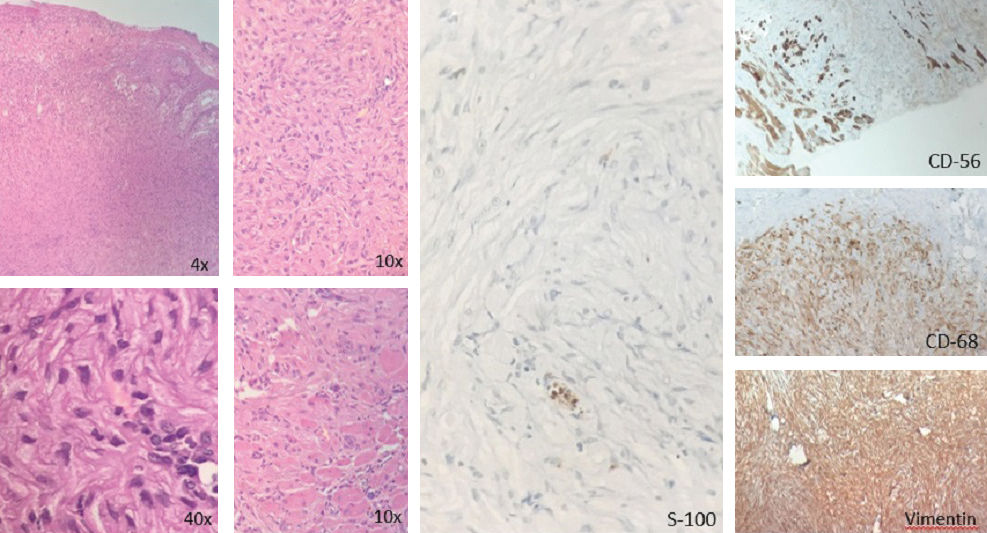
Case ReportA 47- year- old male patient presented with a 5-month history of a rapidly growing solitary lesion on the mucosa and semimucosa of the lower lip. Physical examination showed a painful solid exophytic bleeding ulcerated pink tumor measuring 12x13mm, with telangiectasias and yellowish hue in the center involving the mucosa, semimucosa, and linea alba of the left third of the lower lip (Figure 1A). Dermoscopy showed a structureless heterogeneous yellowish and white central zone and an apple jelly hue in the lower lateral portion of the tumor with multiple polymorphous vessels in the periphery (dotted, coiled, and looped) (Figure 1B). Histological examination revealed an exophytic ulcerated lesion consisting of cells with granular cytoplasm and homogeneous nuclei with low mitotic rate and no cellular atypia, located on the lamina propria and with skeletal muscle infiltration, without lymphatic involvement. (Figure 2A). On immunohistochemistry, the lesion was negative for S100, CD57, EMA, CD34, and neuron-specific enolase and positive for vimentin, CD68, and calretinin, weakly positive for CD56, with Ki67 proliferation index of approximately 3% (Figure 2B and 2C). Based on these findings, a diagnosis of non-neural granular cell tumor was made. Further imaging exams were performed, finding no visceral involvement of the tumor. The surgical approach consisted of a full-thickness V-shaped excision with a 5mm margin under tumescent anesthesia. A 3-layer closure (oral mucosa, orbicularis oris muscle, and overlying skin) was performed, and peripheral and deep margins were clear (Figure 3). After one year of follow-up, no evidence of recurrence or metastasis was seen.
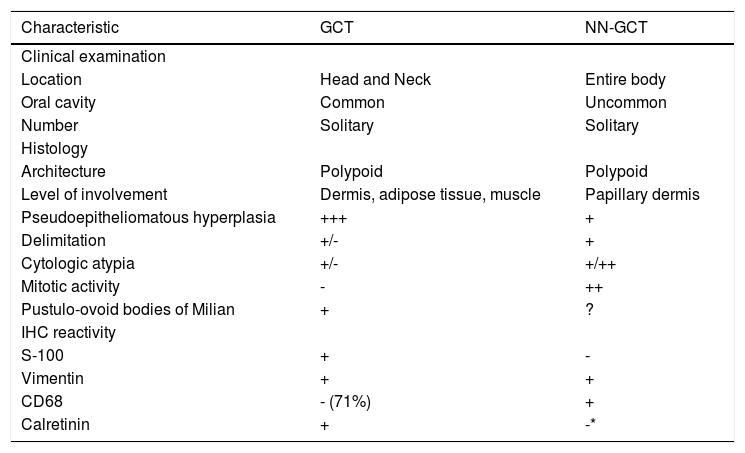
NNGCT or S100 negative granular cell tumor is one of the tumors of the oral cavity histologically composed of granular cells.2 Histologically, GCT and NNGCT are indistinguishable, and they are usually differentiated by immunohistochemistry.3 However, there are some clinical, histological, and immunohistochemical differences that may help distinguish between these unusual tumors (Table 1).2,4 As recently described, the NNGCT IHC profile is not well defined; however, vimentin and CD68 positivity is well established.3 In the literature, the only five cases of this tumor in the oral cavity report surgical excision as the treatment of choice, but there are no details on margins or any suggested surgical approach.2,3,5,6 Full-thickness V excision with 5mm margin and primary closure is a feasible approach with excellent functional and cosmetic results as observed in our patient.
Differences between granular cell tumor and non-neural granular cell tumor
| Characteristic | GCT | NN-GCT |
|---|---|---|
| Clinical examination | ||
| Location | Head and Neck | Entire body |
| Oral cavity | Common | Uncommon |
| Number | Solitary | Solitary |
| Histology | ||
| Architecture | Polypoid | Polypoid |
| Level of involvement | Dermis, adipose tissue, muscle | Papillary dermis |
| Pseudoepitheliomatous hyperplasia | +++ | + |
| Delimitation | +/- | + |
| Cytologic atypia | +/- | +/++ |
| Mitotic activity | - | ++ |
| Pustulo-ovoid bodies of Milian | + | ? |
| IHC reactivity | ||
| S-100 | + | - |
| Vimentin | + | + |
| CD68 | - (71%) | + |
| Calretinin | + | -* |
NNGCT dermoscopy had never been reported before. Polymorphous vascular structures in the periphery such as dotted, coiled, and looped vessels and structureless yellowish zone were some of the findings observed in the tumor dermoscopy, similar to those in cutaneous GCT.7 Additional dermoscopy reports are needed to better characterize this type of tumors and possibly define dermoscopic characteristics that could guide the clinician to an accurate clinical diagnosis.
Financial support: None.
Conflict of interest: None.