Dermoscopic examination allows visualization of horizontal images on the skin, showing well-defined patterns. The authors propose ex vivo dermoscopic visualization using a vertical view of skin sections. The new image clearly distinguishes the stratum corneum, epidermis, and dermis as well as the anatomical location of the pigment. Will this new approach be useful in dermoscopic diagnosis? Further studies are needed.
Dermoscopy is an essential tool for diagnosis of melanocytic lesions. Its use with contact non-polarized light or polarized light allows visualization of the skin’s horizontal plane. Diagnostic accuracy may increase by up to 49% if the dermoscopy is performed by an experienced professional.1 The technique thus enhances the dermatologist’s ability to differentiate between benign and malignant lesions.2
In some cases, the correct diagnosis is made after a more extensive search for subtle clues in the biopsy specimen, driven by valorization of dermoscopic findings communicated to the pathologist.3 The structures seen under dermoscopy have specific correlates in histopathologic studies. Understanding these histopathologic correlates allows clinicians to better assess the dermoscopic features of pigmented lesions.4
Scope et al.3 analyzed the role of dermoscopy in clinical practice1 and proposed the use of ex vivo dermoscopic examination to identify areas of greatest concern and orient tissue sections by the pathologist. The methodology led to optimal correlation between clinical presentation and histopathology. This is essential, since gaps between the clinical presentation and histopathology could lead to diagnostic discordance.5,6
In a previous article, the current authors used horizontal ex vivo dermoscopy to correlate clinical and histopathologic findings in lesions and demonstrated that the areas of greatest concern in dermoscopy corresponded to those with disruption of the cytoarchitecture.6 While processing sections in suspicious areas, dermoscopy was performed on the section’s vertical side, allowing clear identification of the stratum corneum, epidermis, and the limit with the dermis, regardless of the presence or absence of pigment (chromophores), probably due to the structures’ different refractive indices. Surprisingly, it was also possible to observe the dermoscopic images of the chromophores, including identification of their anatomical location.
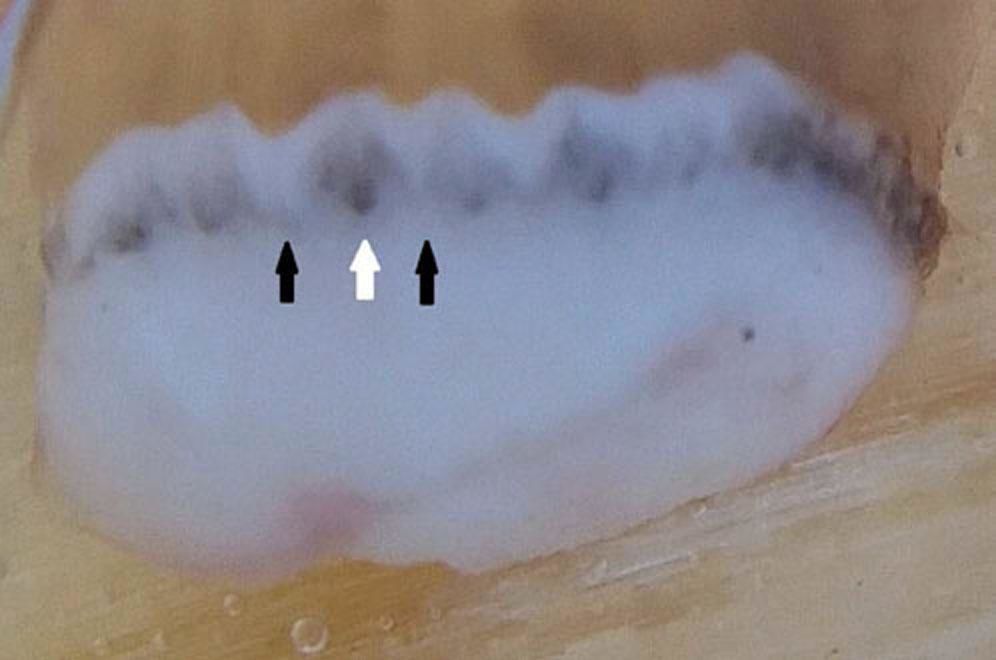
To better demonstrate this technique of ex vivo dermoscopy applied to the vertical plane, we selected a phototype-IV patient presenting a pigmented lesion on the left plantar region, with several years’ evolution (Figure 1). First, dermoscopic examination was performed, allowing visualization of the parallel ridge pattern, supporting the suspicion of an acral lentiginous melanoma (Figure 2).
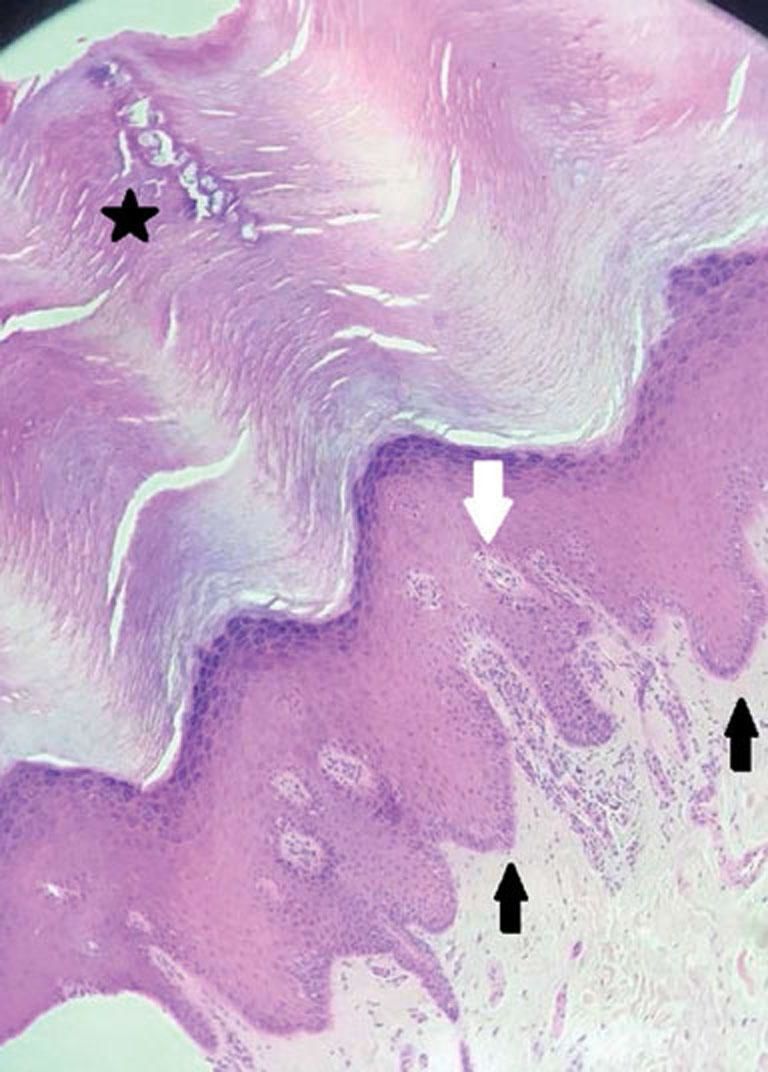
This was followed by a biopsy, and with the aid of the dermoscope, the dermatopathologist performed a perpendicular slice to the parallel ridges (Figure 3). The aim of this plane was to better observe the anatomical characteristics of the plantar region, whose epithelial ridges are longitudinal and interspersed by the intermediate ridges, where the adnexal duct of the sweat glands is located.7 Dermoscopic examination of the vertical plane allowed visualization of the thick stratum corneum and the epidermis and its clear limit with the dermis. Based on the type of section, it was also possible to identify the border ridges, including the intermediate ridges. The location of the chromophores (melanin) was circumscribed to the intermediate ridges and often marked the intraepithelial duct of the sweat glands, reaffirming the parallel ridge pattern (Figure 4). Anatomopathological examination, usually performed on the same plane as this dermoscopic method, showed perfect correlation between the vertical dermoscopic image and histopathology (Figure 5). Anatomical pathology revealed acral melanoma. The areas of greatest concern in dermoscopy matched those with the greatest cytoarchitectural disruption. Ex vivo examination allowed determining the exact sites for sections and correlation with pathology.
Histologic section of plantar skin shows hyperparakeratosis with melanocytic atypia in the basal layer of epidermal ridges with pleomorphism and oriented upwards, characterizing malignant melanocytic lesion/acral melanoma. White arrow shows the intermediate ridge. Black arrow shows the limiting ridges. The star represents the glandular duct
This dermoscopic technique applied to a case of acral lentiginous melanoma led to more accurate diagnosis, suggesting its potential usefulness for other diagnoses such as melanocytic nevi.
The longitudinal biopsy section combined with dermoscopy improved the correlations between the in vivo lesion and the ex vivo dermoscopy for both clinicians and pathologists, thus aiding identification of the lesions’ typical features. Vertical plane ex vivo dermoscopy is intended to better correlate the lesions’ clinical information with their distinctive histopathologic features in order to optimize diagnosis and reduce possible misunderstandings that may occur in the diagnosis of benign versus malignant melanocytic lesions, potentially with better outcomes in both situations.
In summary, vertical plane ex vivo dermoscopy supported the suspicion of clinical and horizontal dermoscopic features of a lesion through the precise anatomical localization of the pigmentary process and its anatomopathological correlation. New observations are needed to assess whether this new approach will add value to the diagnosis and characterize new dermoscopic patterns on the skin’s vertical plane.
Financial support: None.
Conflict of interest: None.