Dear Editor,
American cutaneous leishmaniasis (ACL) is a dermatozoonosis of wide distribution and great incidence in the Brazilian territory. It is caused by several protozoa of the genus Leishmania and is transmitted by the bite of phlebotomine sandflies.1
It typically affects individuals who work in forests such as geologists, farmers, miners, and forest technicians. Therefore, it is characterized as an occupational disease. However, over the last years, ACL has been undergoing urbanization.1
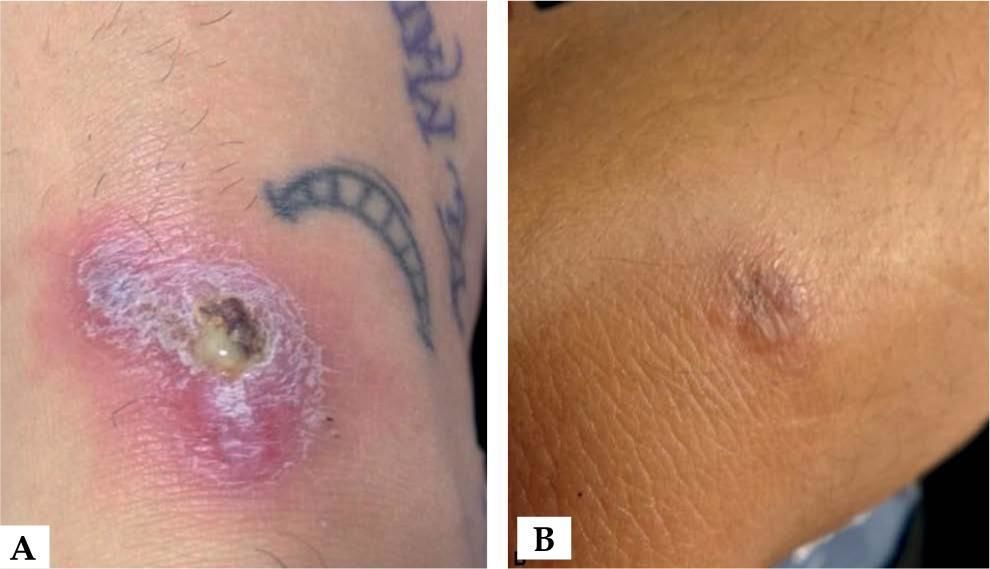
We describe two cases that occurred in the urban area of Belém: a 26-year-old military man, who had been presenting with an erythematous-infiltrated plaque of approximately 1.5 cm in the right elbow for 8 months; and a 22-year-old female dentist, who had been presenting with an erythematous-infiltrated plaque with scaling and a central serohematic crust, measuring approximately 3.0 x 1.5 cm on the dorsum of the right foot for 5 months (Figure 1).
Both lived in the urban area of Belém. The man lived in the Val-de-Cans neighborhood and the woman at Parque Verde. These neighborhoods are close to each other and they both show forest fragments (Figure 2). The patients denied having gone on recent trips and having been to forests.
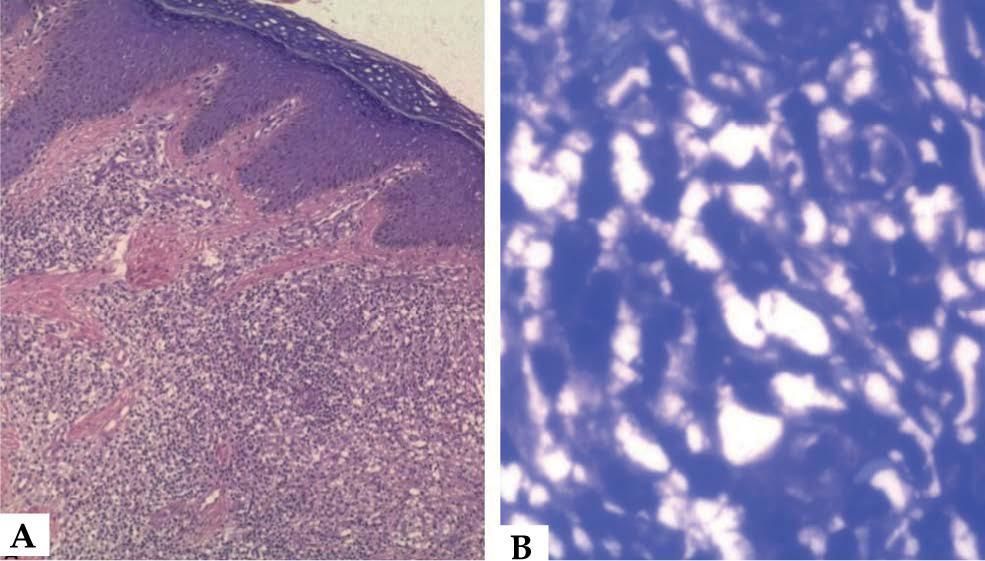
They underwent biopsy of the lesions and the histopathological results showed hyperplastic epidermis, with orthokeratosis, hypergranulosis, irregular acanthosis, and spongiosis on the dermis with moderate inflammatory infiltrate formed by lymphocytes, histiocytes, rare plasmocytes and eosinophils, arranged around the superficial capillaries and between the dermal collagen fibers. We observed presence of structures similar to leishmanias in the infiltrate and inside macrophages (Figure 3).
A: Hyperplastic epidermis with orthokeratosis, hypergranulosis, irregular acanthosis, and spongiosis on the dermis with moderate inflammatory infiltrate formed by lymphocytes, histiocytes, rare plasmocytes, and eosinophils (Hematoxylin & eosin, X4)
B: Leishmania inside macrophages (Hematoxylin & eosin, X40)
Patients were treated with 15mg Sb +5/kg/day of N-methyl glucamine for 20 consecutive days, evolving with lesion regression.
Cases of autochthonous ACL in the urban areas of Brazilian municipalities have been described, such as those of two individuals in the Caju neighborhood, in the city of Rio de Janeiro. These cases indicate a change in the epidemiological pattern of ACL.2
The urbanization of ACL probably results from the domestication of the components of its transmission cycle due to deforestation, with the spread of disease-transmitting insects and host mammals to intra or peridomicillary sites.3
A study in a municipality of Minas Gerais indicated rodents of the species Rattus rattus and Mus musculus (species usually associated with human dwellings) as possible reservoirs of the disease in the urban area, after the detection of specimens infected with Leishmania brasilienses.4
In a recent survey conducted in Manaus, it was observed that patients with urban ACL often resided near areas of residual forest within the city boundaries.3
The metropolitan area of Belém has been undergoing an accelerated process of urbanization since the middle of the 20th century, which has caused a decrease in natural vegetation and possibly in the fauna of ACL vectors. However, some forest fragments still remain in the city.5
A survey conducted between 2014 and 2016 found phlebotomine sandflies infected with L. (L.) amazonensis in a forest fragment in the metropolitan area of Belém, which allows us to conclude that forest fragmentation does not prevent the maintenance of the Leishmania cycle.5
We report these cases to reinforce the importance of continuing with the diagnostic investigation of ACL, even though the epidemiology presented by the patient may not be the classic one.