Dear Editor,
By definition, sarcomas are malignant tumors of tissues, derived from mesoderm and involve the oncogenic transformation of mesenchymal stem cells. The two main types of sarcoma are bone and soft tissue sarcomas. Soft tissue sarcomas generally manifest as deep lesions, but they may affect the skin and subcutaneous tissue.1 They are grouped according to similarities in their clinical presentation and histopathological appearance. However, they have different cellular origins.2
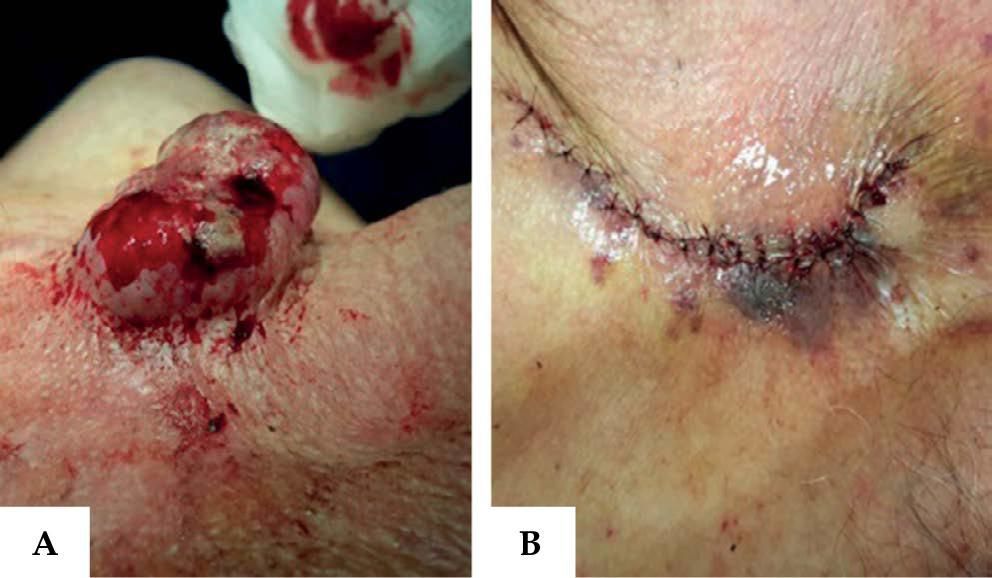
Undifferentiated pleomorphic sarcoma is a tumor whose histogenesis is not yet clearly defined.1 We describe a case of undifferentiated pleomorphic sarcoma with cutaneous presentation and review some aspects of the disease, describing the main differential diagnoses and the clinical and histopathological findings of this rare tumor in its exuberant form, based on the current literature. We report the case of a 74-year-old male patient who sought treatment due to a rapid-onset skin lesion in the thoracic region after two months of disease evolution. He denied having any associated systemic symptoms. Dermatological examination revealed a vegetative and ulcerated tumor, friable, measuring 6cm in diameter, located in the right upper thoracic area (Figure 1). The patient underwent surgery with complete resection of the lesion and wide safety margins (Figure 1).2
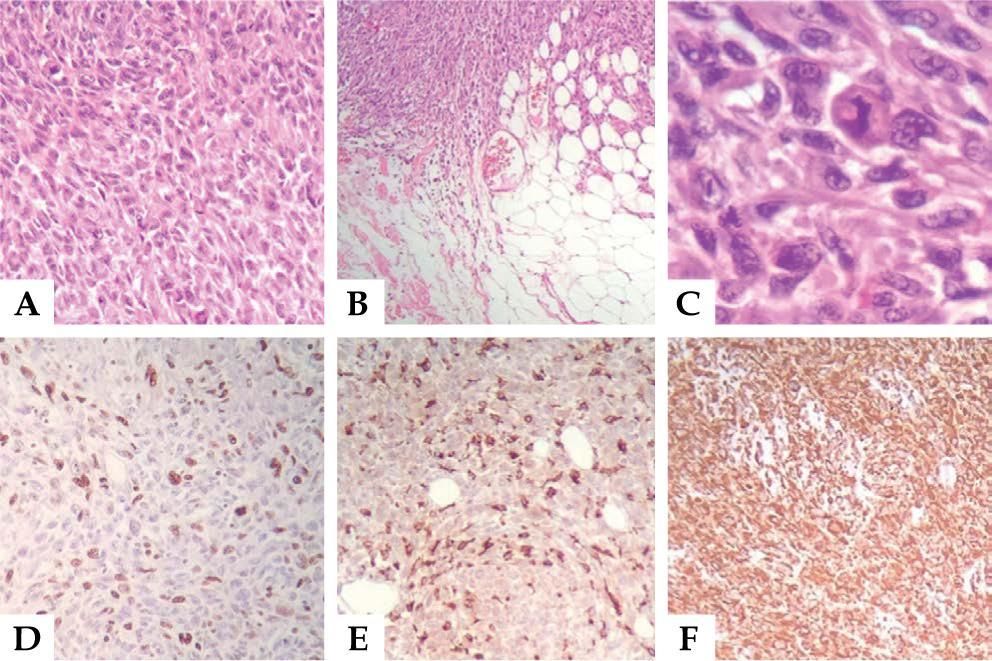
Histopathological examination associated with immunohistochemical (IHC) profile (Vimentin and CD68 positive) were compatible with undifferentiated pleomorphic sarcoma (malignant fibrous histiocytoma), but negative for other markers, such as high molecular weight cytokeratin, CD45, S100 protein, MELAN-A, HMB45, CD56, CD24, desmin, CD31, and Bcl2, which excluded other cancers, such as amelanotic melanoma, Merkel cell carcinoma, and lymphoma (Figure 2). The patient was referred to the oncology department for staging. Imaging tests showed no signs of metastatic disease. He is in outpatient follow-up without signs of lesion recurrence. The reclassification of soft tissue sarcomas based on the 2002 World Health Organization requires the identification of the lineage of origin for the categorization of the tumor.1
A: Intense proliferation of pleomorphic cells in the dermis (Hematoxylin & eosin, X200); B: Infiltration of adipose tissue with neovascularization (Hematoxylin & eosin, X100); C: Fusiform and polygonal pleomorphic multinucleated cells with hyperchromasia of the nucleoli and mitotic figures (Hematoxylin & eosin, X400); D: Immunohistochemistry 90% highly positive for Ki-67 antibody, a cell proliferation marker, CD-68; E: A macrophage marker (IHC, X200); and F: Vimentin, a mesenchymal cell marker, IHC X100).
In many cases, a careful and detailed immunohistochemical and ultrastructural evaluation leads to the possible or conclusive classification of the tumor into the histogenetic subtypes of sarcoma.2 With the most current classification in mind, two tumors are most likely to affect the skin: undifferentiated pleomorphic sarcoma (formerly storiform-pleomorphic malignant fibrous histiocytoma) and myxofibrosarcoma (formerly myxoid malignant fibrous histiocytoma).3 Both tumors are more common in the elderly and may present themselves as a subcutaneous mass, more commonly affecting the limbs.4 In the skin, they usually present themselves as skin-colored nodules, ranging in texture from elastic to firm. Their growth is sometimes fast.1 Clinically and histopathologically, they may resemble malignant melanoma, squamous cell carcinoma, dermatofibrosarcoma protuberans, atypical fibroxanthoma, and leiomyosarcoma.2 The extremities are the most common sites of involvement, especially the lower limbs. However, any area of the body can be affected, and approximately 10-15% are located in the tissue of the head and neck.5 For diagnosis, histopathology study associated to the immunohistochemistry are necessary.5 The basis of treatment is total surgical resection of the tumor with wide safety margins. An adjuvant radiotherapy is important to improve local control, especially in high-grade lesions and in patients with compromised surgical margin after broad excision. Even 50% of cases show distant metastasis (usually lung and lymph nodes) with common recurrence.1