A hospital-based cross-sectional study was performed, including 117 psoriatic patients and 117 controls matched for age, gender, and body mass index. Psoriatic patients had higher levels of serum uric acid (6.25 ± 1.62 vs 5.71 ± 1.35 mg/dl; P=0.019) and significantly greater prevalence of hyperuricemia (31.6% vs 16.2%; P=0.009) than individuals without psoriasis. Psoriatic patients had significantly higher serum uric acid than controls in subjects without metabolic syndrome. Multivariate logistic regression analysis showed that psoriasis can be a strong predictor of hyperuricemia (odds ratio 2.61; 95% confidence interval 1.34-5.00; P=0.004).
Psoriasis is a chronic inflammatory and immune-mediated disease that affects the skin and involves several other organs and systems.1 Recent studies have linked psoriasis to metabolic syndrome.2,3 Similarly, it is generally accepted that hyperuricemia frequently accompanies psoriasis and psoriatic arthritis.4 The present study investigated the correlation between hyperuricemia and psoriasis by comparing serum uric acid (SUA) levels and prevalence of hyperuricemia in psoriatic patients and controls.
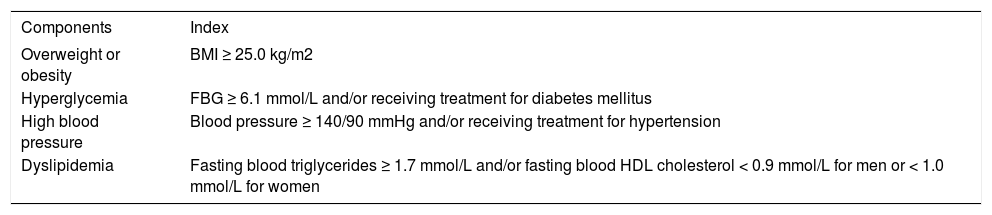
This descriptive, cross-sectional study included 117 adult psoriatic patients from the Department of Dermatology at Peking Union Medical College Hospital. Exclusion criteria were systemic antipsoriatic treatment within 3 months of enrolment and use of medications known to affect SUA level. Disease severity was scored using the Psoriasis Area and Severity Index (PASI). The control group consisted of 117 adult individuals selected in a 1:1 ratio matched for age, sex, and body mass index (BMI) with psoriatic patients from the Department of Physical Examination Centre.5 Metabolic syndrome was defined according to the criteria of the Chinese Diabetes Society (CDS) in 2004, which was more suitable for Chinese individuals (Table 1). 6 Hyperuricemia was defined as SUA level ≥7 mg/dl in men and ≥6 mg/dl in women, or allopurinol use. Statistical analysis was performed using SPSS 20 (IBM, Armonk, NY, USA) and GraphPad Prism software packages.
Diagnostic criteria for metabolic syndrome recommended by the Chinese Diabetes Society (.3 of the following criteria are required)
| Components | Index |
|---|---|
| Overweight or obesity | BMI ≥ 25.0 kg/m2 |
| Hyperglycemia | FBG ≥ 6.1 mmol/L and/or receiving treatment for diabetes mellitus |
| High blood pressure | Blood pressure ≥ 140/90 mmHg and/or receiving treatment for hypertension |
| Dyslipidemia | Fasting blood triglycerides ≥ 1.7 mmol/L and/or fasting blood HDL cholesterol < 0.9 mmol/L for men or < 1.0 mmol/L for women |
FBG: fasting blood glucose; HDL: high-density lipoprotein
Source: Advice, 2004.6
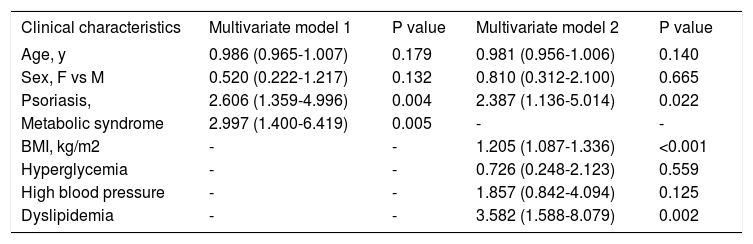
Patients with psoriasis had a higher prevalence of dyslipidemia (57.3% vs 39.3%, p=0.006), whereas high blood pressure, hyperglycemia, and metabolic syndrome did not differ significantly between the two groups. SUA levels were significantly higher in psoriatic patients compared to controls (6.25±1.62 vs 5.71±1.35mg/dl; p=0.019), and hyperuricemia was significantly more common in psoriatic patients than in control subjects (31.6% vs 16.2%; p=0.009). Male and female psoriatic patients had significantly higher SUA levels than their control counterparts (6.61±1.6 vs 6.06 ±1.2 mg/dl in men and 5.12±1.1 vs 4.58±1.0mg/dl in women). However, the results changed when participants were further stratified according to presence of metabolic syndrome. In subjects with metabolic syndrome, SUA levels were similar between psoriatic patients and controls (p=0.3537). Meanwhile, SUA levels were significantly higher in psoriatic patients than controls in subjects without metabolic syndrome (p=0.0035). Multivariate logistic regression showed that both psoriasis and metabolic syndrome, independently of each other, were risk factors for hyperuricemia (Table 2). Additionally, SUA level was positively correlated with BMI (r = 0.46; p <0.001), serum triglycerides (r = 0.30; p<0.001), and sex (r = 0.42; p<0.001) but was not significantly correlated with age or the duration of psoriasis. Among psoriatic patients, mean SUA was higher in patients with PASI ≥10 (n=112) than in those with PASI <10 (n=5) (SUA: 5.5±1.1 vs 6.3±1.6mg/dl). However, SUA was not significantly associated with PASI.
Predictors of hyperuricemia in the total sample of participants: multivariate logistic regression models
| Clinical characteristics | Multivariate model 1 | P value | Multivariate model 2 | P value |
|---|---|---|---|---|
| Age, y | 0.986 (0.965-1.007) | 0.179 | 0.981 (0.956-1.006) | 0.140 |
| Sex, F vs M | 0.520 (0.222-1.217) | 0.132 | 0.810 (0.312-2.100) | 0.665 |
| Psoriasis, | 2.606 (1.359-4.996) | 0.004 | 2.387 (1.136-5.014) | 0.022 |
| Metabolic syndrome | 2.997 (1.400-6.419) | 0.005 | - | - |
| BMI, kg/m2 | - | - | 1.205 (1.087-1.336) | <0.001 |
| Hyperglycemia | - | - | 0.726 (0.248-2.123) | 0.559 |
| High blood pressure | - | - | 1.857 (0.842-4.094) | 0.125 |
| Dyslipidemia | - | - | 3.582 (1.588-8.079) | 0.002 |
Model 1 = age, sex, presence of psoriasis, and metabolic syndrome;
Model 2 = age, sex, presence of psoriasis, BMI, hyperglycemia, high blood pressure, and dyslipidemia.
In this study, the prevalence of asymptomatic hyperuricemia was approximately twice as high in psoriatic patients than in matched controls. Moreover, psoriasis was a significantly positive predictor of hyperuricemia after adjusting for associated baseline characteristics such as age, sex, BMI, and other features of metabolic syndrome. To date, convincing evidence has indicated that psoriasis is independently associated with hyperuricemia.5,7-9 In line with the previous studies, our findings also demonstrated that psoriasis itself might contribute directly to hyperuricemia. However, our study did not find a correlation between serum uric acid levels and severity of psoriasis.
Our findings can have clinical implications, since elevated SUA independently predicts the development of cardiovascular disease events and mortality in nonpsoriatic populations.5 Some studies have suggested that psoriatic patients with hyperuricemia show remarkable improvement in their psoriasis when treated for hyperuricemia.7 Wei et al.10 concluded that higher doses of allopurinol contributed to lower risks of both cardiovascular events and mortality. We recommend that SUA should be routinely measured in patients with psoriasis, especially in those with obesity, hypertension, or dyslipidemia; drug treatment of hyperuricemia might be a useful strategy for psoriasis.
The limitation of our study was that the patients enrolled were biased toward having higher disease severity, since the study population was based in a tertiary medical center. Large interventional clinical trials are needed to confirm the association between hyperuricemia and psoriasis and the efficacy of high-dose allopurinol treatment in psoriatic patients with hyperuricemia.
Financial support: The present study was supported by the Medical and Health Science and Technology Innovation Project of the Chinese Academy of Medical Sciences (NO.2017-12M-3-020).
Conflict of interest: None.