Nodular vasculitis is an uncommon type of panniculitis. It was firstly associated to the infection by Mycobacterium tuberculosis and named erythema induratum of Bazin, however nowadays it has been associated with several other underlying disorders and it is better described as nodular vasculitis. Concerning its relationship with malignant conditions, there is only one reported case, in association with metastatic colon adenocarcinoma. We report a case of nodular vasculitis as the first manifestation of lung adenocarcinoma. To the best of our knowledge, this is the first reported association of both diseases.
Nodular vasculitis (NV) is an uncommon form of panniculitis characterized by erythematous nodules or plaques located preferentially on the calves, which may ulcerate and drain. It has been regarded as a delayed hypersensitivity response to an antigenic stimulus, being originally associated with tuberculosis.1 However, some cases in association with both non-tuberculous infections, such as hepatitis B and C virus,1-2 and non-infectious conditions, such as autoimmune diseases,2 inflammatory bowel disease3 and drugs4 were reported. NV has rarely been associated with malignant diseases, with only one case reported in the literature related to metastatic colon adenocarcinoma.5 Histopathologic features include a septal/lobular panniculitis with a mixed inflammatory infiltrate containing lymphocytes, plasm cells, histiocytes forming granulomas, neutrophils, eosinophils and vasculitis.6
Case ReportA 63-year-old woman was seen with tender, erythematous lesions on both legs that appeared 8 days before. Patient denied other symptoms such as fever, weight loss, asthenia or cough. Past medical history included arterial hypertension, type 2 diabetes mellitus, acute ischemic stroke without sequelae and venous insufficiency of lower limbs. She was not a smoker. Her brother was a heavy smoker and had had lung cancer.
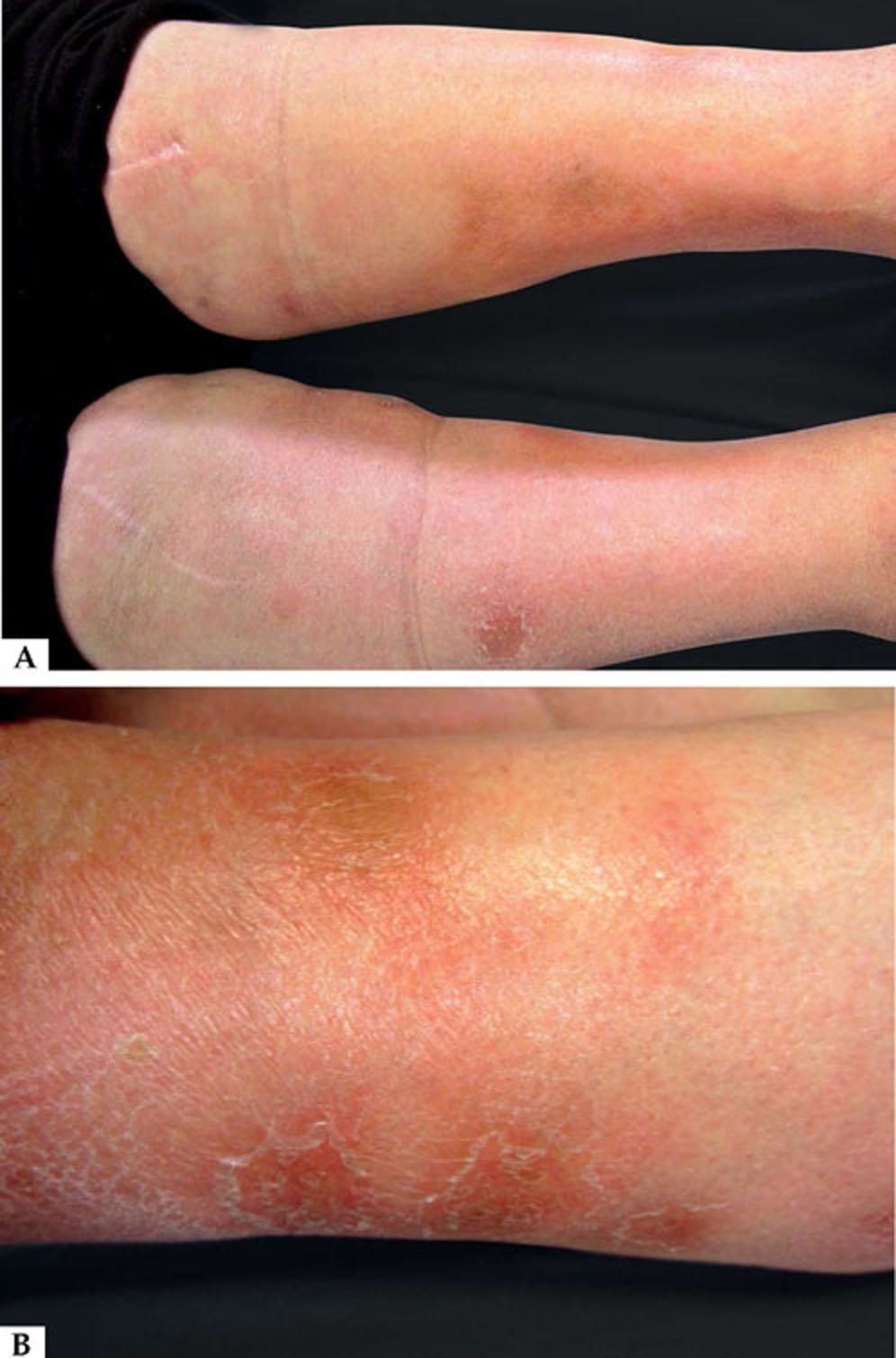
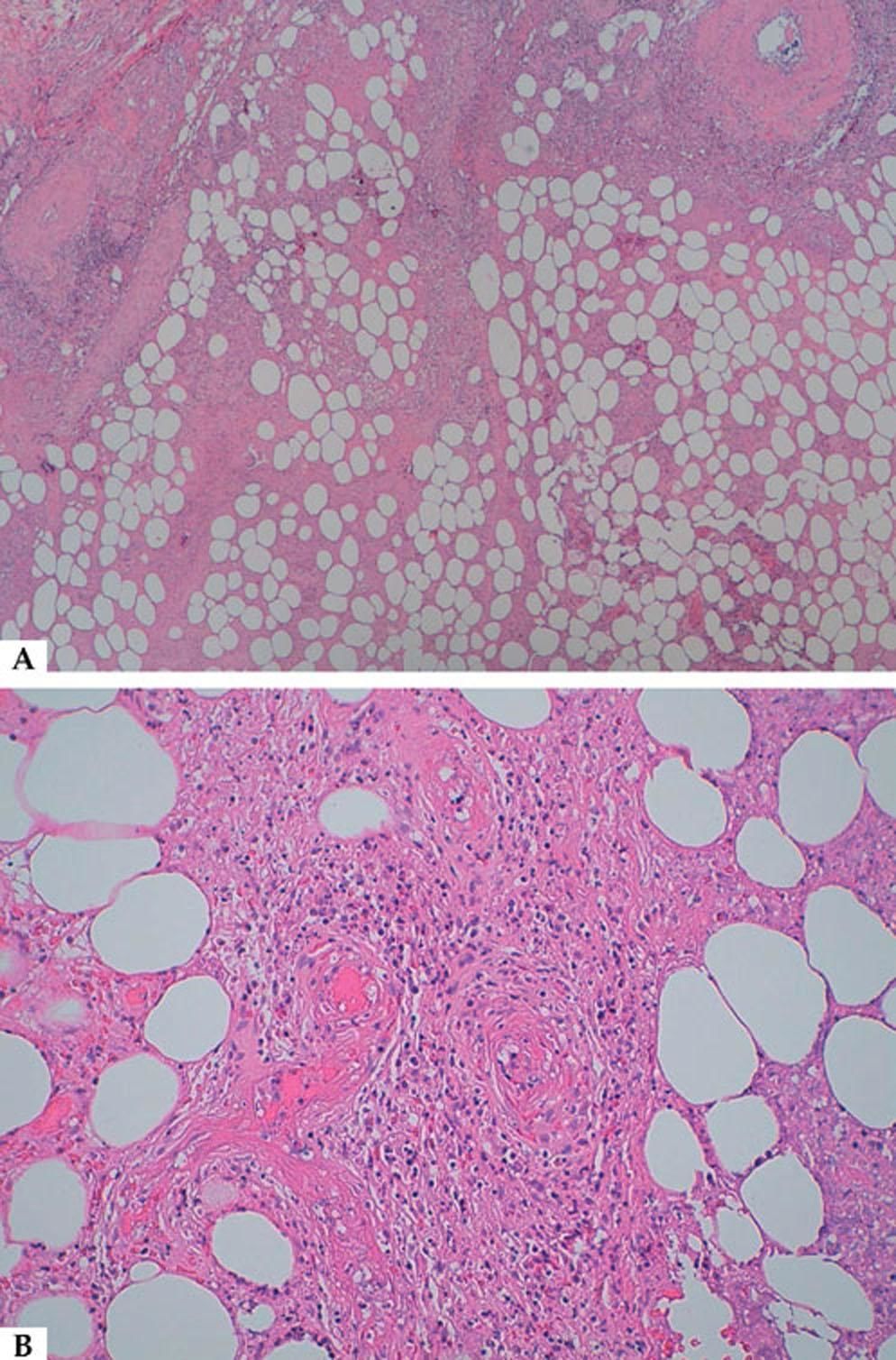
Physical examination revealed a symmetrically distributed dermatosis, with several ill-defined non-ulcerated bilateral tender erythematous subcutaneous nodules with 2-4 cm located on the legs (Figure 1). On histopathologic examination, there was a predominantly lobular panniculitis with vasculitis and necrosis (Figure 2A). The inflammatory infiltrate contained mononuclear cells and neutrophils (Figure 2B).
Complementary investigation was performed, with a negative tuberculin skin test; on chest X-ray a suspicious pulmonary nodule was observed, which presence was confirmed by computed tomography. A transbronchial aspiration biopsy identified a lung adenocarcinoma. Appropriate staging exams were compatible with T3N2M1 (stage IV).
The patient was submitted to the indicated chemotherapy, with partial response followed by disease relapse without response to second and third line chemotherapy. The patient died 3 years after the diagnosis. As for this dermatosis, the lesions followed the disease course, with slight initial improvement and relapse along with the oncologic disease.
DiscussionParaneoplastic syndromes are signs or symptoms that occur as a result of organ or tissue damage at locations remote from the site of the primary tumor or metastases. A wide variety of paraneoplastic syndromes are associated with lung adenocarcinoma. The symptoms often precede the diagnosis of the associated lung cancer, especially when the symptoms are neurologic or dermatologic, and the improvement generally occurs with targeted treatment of the underling tumor.7
Considering the rarity of the dermatosis in the general population, the concurrent onset and similar clinical course of both conditions, this case of NV is suggestive of a paraneoplastic manifestation of the lung adenocarcinoma.
The physiopathology of paraneoplastic syndromes is not clear, however, some authors proposed an aberrant release of humoral mediators, hormones and hormone-like peptide by the tumor as the main pathogenic mechanism.7 Additionally, NV should be regarded as a delayed hypersensitivity response to a variety of agents, in which vasculitis, a histologic hallmark, could be the consequence of a cell-mediated cytotoxicity target to circulating immune complexes. Such findings support the hypothesis that NV could be a paraneoplastic skin manifestation due to circulating tumoral antigens.
The early recognition of paraneoplastic syndromes may contribute to the detection of a highly treatable, early-stage tumor. Therefore, the identification of NV as the initial presentation of a tumor could be very important for the prognosis of the patient. On the other hand, this case reported emphasizes the need for more studies to understand the pathogenesis of NV.
Financial support: None.
Conflict of interest: None.