Dear Editor,
Amelanotic melanomas are characterized by absence of pigment.1 They are an infrequent variant of classically described clinical and pathological subtypes, estimated occur in between 2 and 8% of all cases.1,2 Amelanotic melanomas may present as erythematous maculae on sun-exposed areas, with epidermal alterations, normochromic dermal plaques, without epidermal changes or papulonodular lesions.1 The most common form is the nodular variant, but any other clinicopathological form can be found.2 Dermoscopy may serve as a valuable tool for elucidating the suspicion of this entity.2 Although structures that suggest the presence of melanin are absent, it is possible to visualize vascular patterns and residual pigmentation that are not visible to the naked eye.3 The predominant vascular pattern in melanocytic and hypomelanotic melanomas depends on tumor thickness.2 Diagnosis is also hampered by the absence of well-established criteria.4 In addition, they do not differ from pigmented melanomas in terms of prognosis or treatment.1
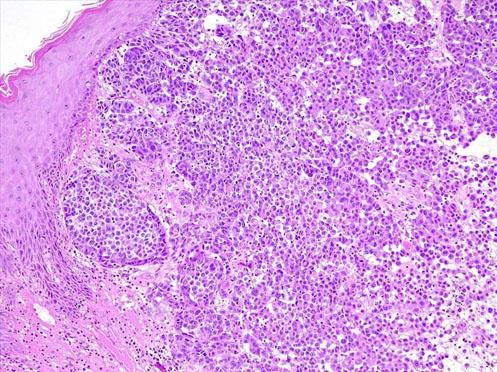
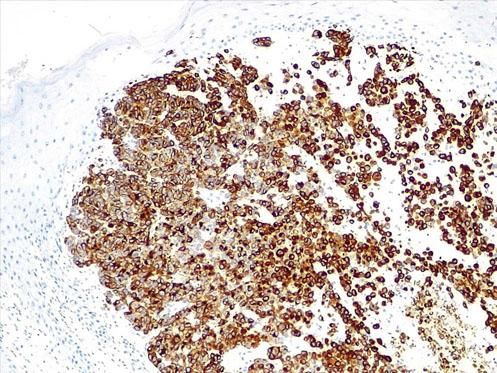
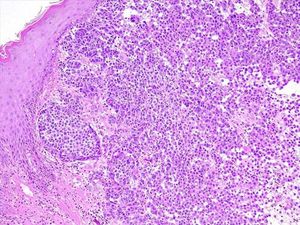
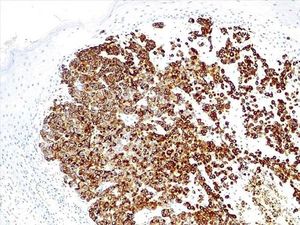
Male patient, 60 years old, with diagnosis of schizophrenia, presented a tumoral lesion approximately 4cm in diameter, pedunculated, in the lumbar region, with a peritumoral erythematous area (Figure 1). The lesion was excised with 2mm margins. Anatomopa-thological examination evidenced an extensive area of ulceration, covered by fibrinous exudate. The dermis showed a malignant neoplasm composed of large epithelioid and fusiform cells, forming cohesive and extensively infiltrative blocks and areas of necrosis. The cells exhibited intense hyperchromasia and pleomorphism, with numerous typical and atypical mitotic figures, evident nucleoli and eosinophils, and presence of brownish pigment (Figure 2). Immunohistochemistry was positive for Melan A, S100, SOX10, and HMB45, confirming the diagnosis of malignant melanoma, nodular type, with Breslow thickness 1.5cm and mitotic index of 15 mitoses/mm2 (Figure 3). Lymphatic, blood, and perineural invasion were not detected. Surgical margins were free, 2.6 mm away from the neoplasia.
Pgmentation is one of the guiding criteria for the diagnosis of melanocytic lesions, and lack of pigmentation often makes the diagnosis of amelanotic melanoma challenging.1,2 In such cases, dermoscopy is important for the evaluation of morphological types of vascular structures.3 The vascular pattern may not be sufficient, and it is essential to associate the clinical findings and patient’s history.3 The definitive diagnosis can only be established by histopathology, and immunohistochemistry is often necessary.2,4 The present report highlights the importance of histopathology and immunohistochemistry for diagnostic elucidation. The lack of defined criteria can delay the suspicion and diagnosis, fundamental to prognosis in this highly aggressive and potentially lethal entity.4
AcknowledgmentsThe authors wish to thank Dr. Geise Rezende Paiva for her collaboration and dedication in preparing the histopathology and immunohistochemistry images.