Melkersson-Rosenthal syndrome (MRS)/orofacial granulomatosis is characterized by the triad of recurrent orofacial edema, recurrent peripheral facial palsy, and fissured tongue.1 The triad is found in 8% to 45% of cases; most patients present with the oligosymptomatic or monosymptomatic forms of the disease.1 The most common clinical manifestation is lip swelling (granulomatous cheilitis).1 The disease mainly affects young adults; pediatric cases are rarely described. A recent series described three cases and reviewed 116 previously published ones.2
The cause of MRS is unknown. The authors of the present study demonstrated an increase in the expression of HLA A*02, HLA DRB1*11 to HLA DQB1*03 and a decrease in the levels of HLA A*01, HLA DRB1*04, HLA DRB1*07, and HLADQB1*02 in patients with MRS when compared to the control group, indicating genes that may predispose to or protect against the disease.3 An association between MRS and Crohn's disease (CD) has been reported by some authors.4
The histopathological findings of MRS include non-caseating granulomas similar to CD, which may suggest that MRS and CD might be part of the same clinicopathological spectrum.1,4
The present report describes seven cases of MRS in children and adolescents, drawing attention to a possible association with CD.
The analyzed data from the cases diagnosed with granulomatous cheilitis/MRS/orofacial granulomatosis were: sex, age, lesion location, neurological impairment, and colonoscopy exams (Figs. 1–7 and Table 1). The diagnosis was confirmed by the histopathological analysis.5
(A), Patient 4 ‒ granulomatous gingivitis.10 (B), Same patient after gingivoplasty.
Characteristics of the seven patients with pediatric MRS.
| Case/ Sex/ Ethnicity | Age at symptom onset | Age at diagnosis | Affected site | Intraoral involvement | Tongue involvement | Facial palsy | Systemic involvement | Treatment | Follow-up |
|---|---|---|---|---|---|---|---|---|---|
| 1/M/C | 30 m | 43 m | Upper lip | No | No | No | Normal colonoscopy | Thalidomide, 50 mg/day, good response | 2 y |
| 2/M/C | 14 y | 15 y | Upper lip | No | No | No | Normal colonoscopy | Dapsone, 100 mg/day | Lost to follow-up |
| 3/M/C | 11 y | 12 y | Upper and lower lip | No | No | No | Normal colonoscopy | Dapsone, 100 mg/day, good response | 9 m |
| 4/M/C | 10 y | 11 y | Lips and face | Granulomatous gingivitis | Geographic tongue | No | Colonoscopy- Crohn’s disease at 21 years | Dapsone, 100 mg/day (failure) | 14 y |
| Thalidomide, 100 mg/day (failure) | |||||||||
| Azathioprine, 150 mg/day (good response) gingivoplasty | |||||||||
| 5/M/AB | 8 y | 9 y | Upper and lower lip | No | Fissured tongue | No | Non-epileptic seizures | Thalidomide, 100‒200 mg/day (poor result) | |
| Normal colonoscopy | Intralesional Triamcinolone (failure), three cheiloplasties | ||||||||
| 6/M/C | 11 y | 12 y | Granulomatous gingivitis | Geographic and fissured tongue | Yes | Colonoscopy- Crohn’s disease at 17 years | Thalidomide, 100 mg/day, good response | 6 y | |
| 7/F/MR | 15 y | 16 y | Lips and face | Granulomatous gingivitis and palatitis | Fissured tongue | No | Colonoscopy not performed | Dapsone, 100 mg/day | 4 y |
| Prednisone, 40 mg/day | |||||||||
| Intralesional Triamcinolone (all failed) |
M, Male; F, Female; m, months; y, years; C, Caucasian; AB, African-Brazilian; MR, Mixed-race.
This sample represents the largest case series of children with MRS in Latin America.6 The authors’ oral mucosa diseases group conducts 900 medical consultations per year and, over a period of 20 years, only five pediatric MRS cases were seen (Cases 1 and 4 through 7); Cases 2 and 3 came from the private practice of one of the authors.
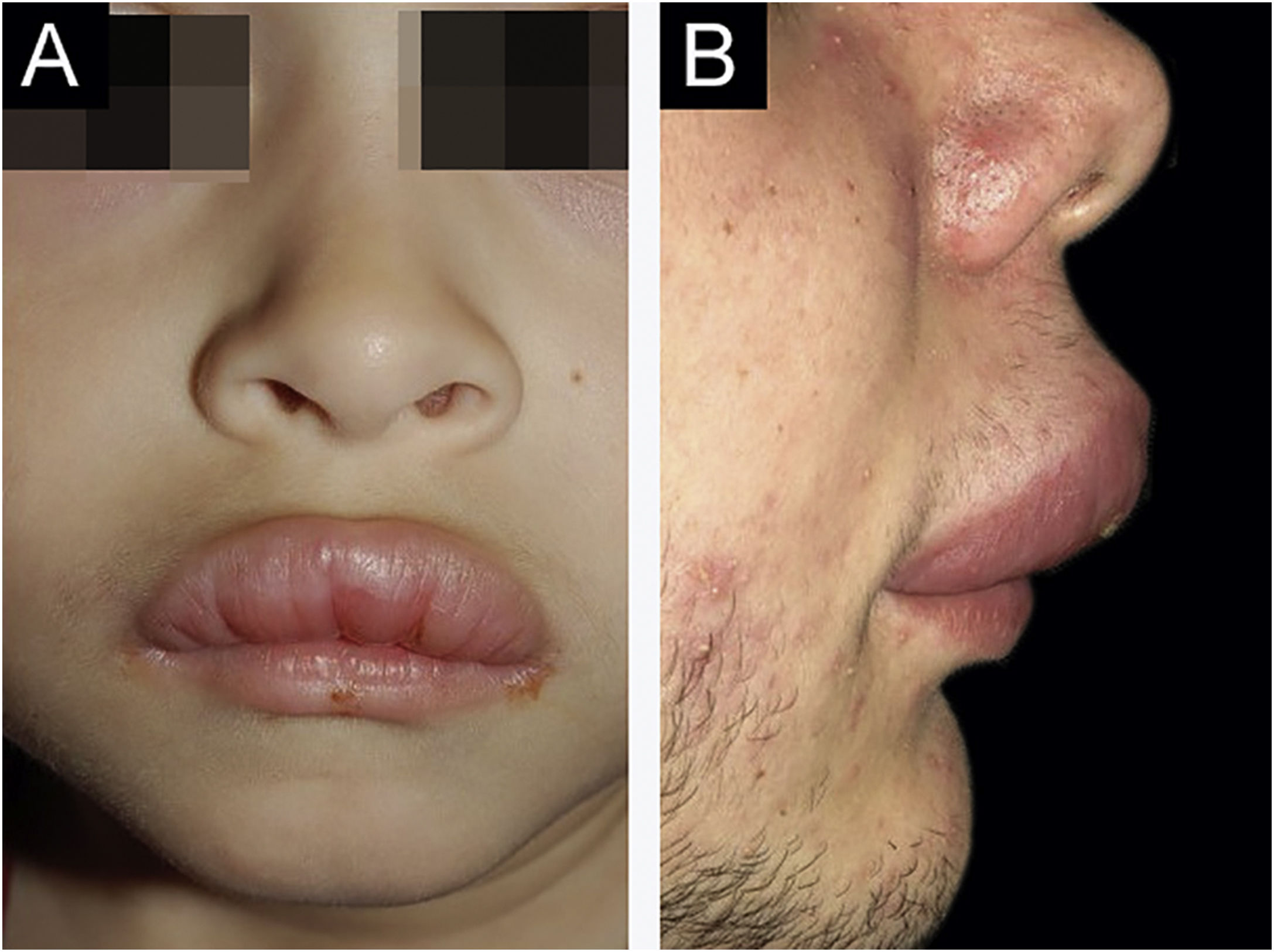
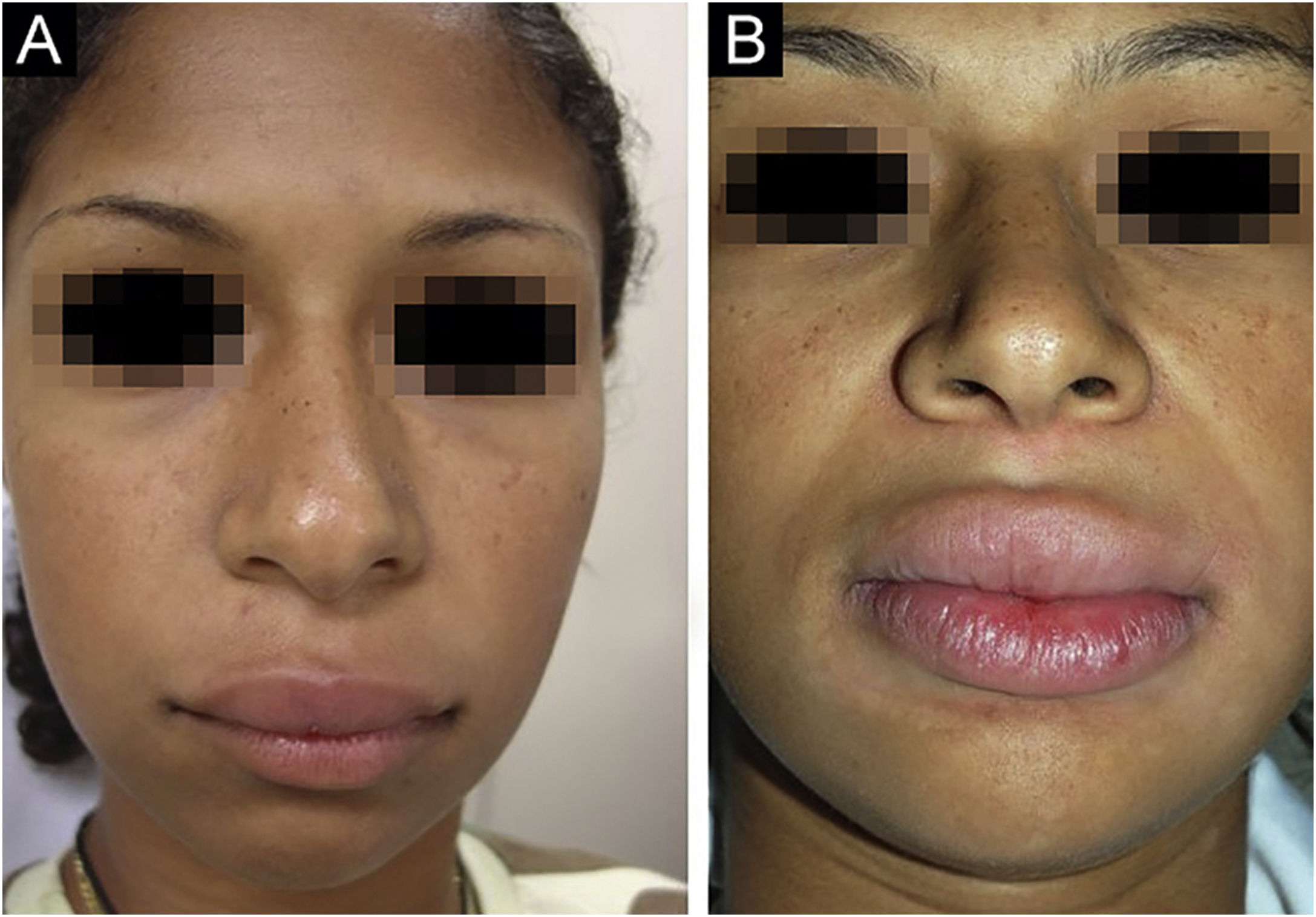
There was a predominance of male patients; the only female patient noticed symptoms at age 15. The cases reviewed by Savasta et al. showed a prevalence of female patients.2 Patient 1 is one of the youngest subjects ever reported (Fig. 1A).
Only patient 6 reported a previous bout of facial palsy, having also had an episode observed by the authors. Facial palsy affected 61/116 (52.6%) of the previously reported pediatric cases.2 Patient 5 had seizures of unknown cause; the neurology team associated them with MRS.1
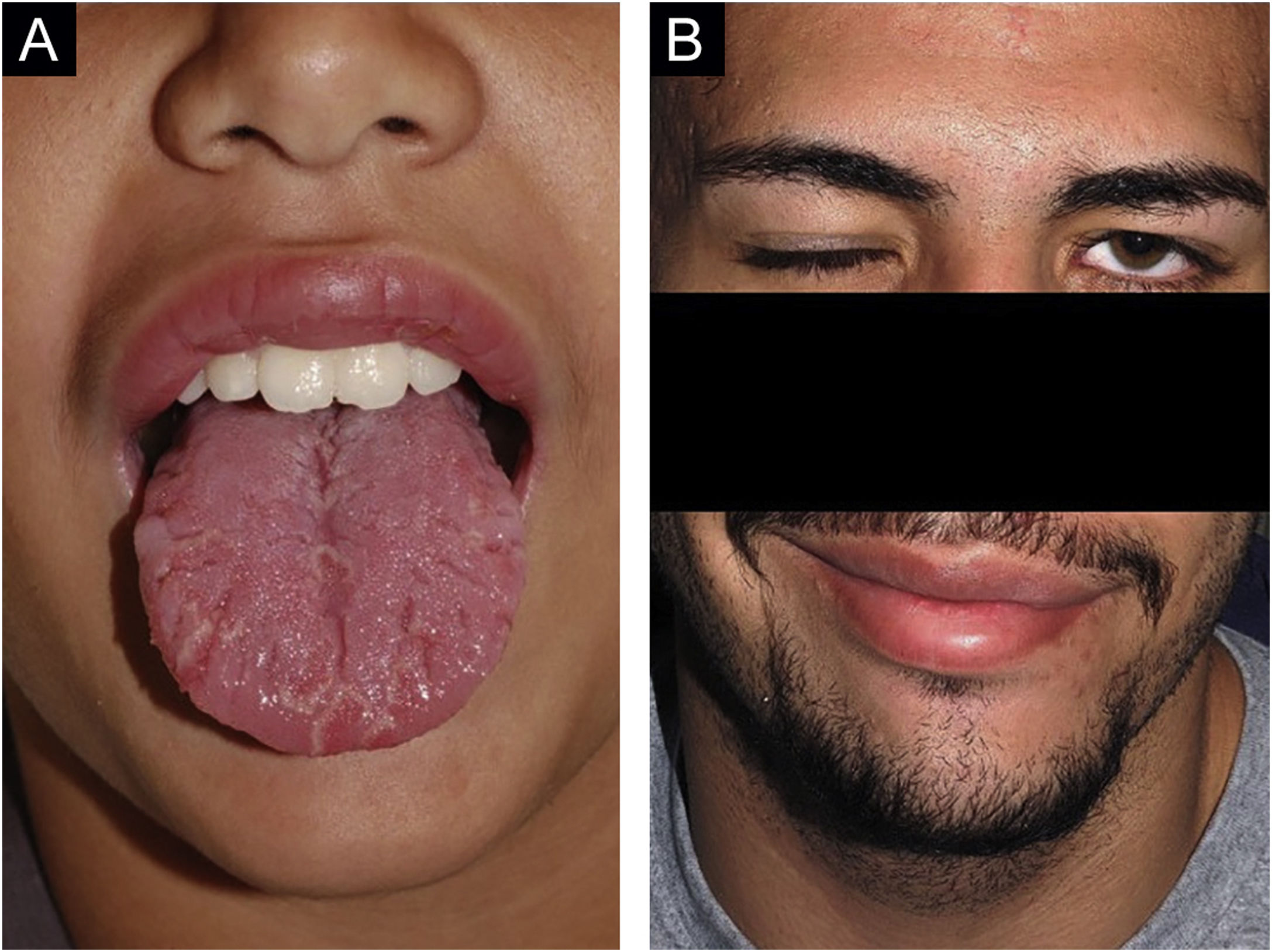
Cases 4, 5, 6 and 7 had fissured tongue; cases 4 and 6 had geographic tongue (Fig. 5A; Case 6 had concomitant fissured tongue). Geographic tongue is characterized by the presence of migrating areas of depapilation surrounded by a serpiginous edge. Histopathology is identical to that of psoriasis and is currently considered a mucosal manifestation of the latter. There is a significant association between psoriasis and Crohn's disease.7 A fissured tongue usually occurs in cases of persistent geographic tongue; the two findings often coexist and represent the same process at different stages.8
Cases 3 and 6 were diagnosed with CD, which was detected many years after the diagnosis of MRS, after controlling for orofacial symptoms. The routine investigation of MRS at the authors’ service currently includes periodic colonoscopy exams.
An association between MRS and CD has been reported.1 The authors’ group published the results of a study with HLA in 36 adult and pediatric cases3 and confirmed the association between MRS and CD in five cases (all had MRS HLA alleles and three had DC alleles). The genetic results obtained by the authors suggest that MRS and CD are distinct diseases, but they may be associated.
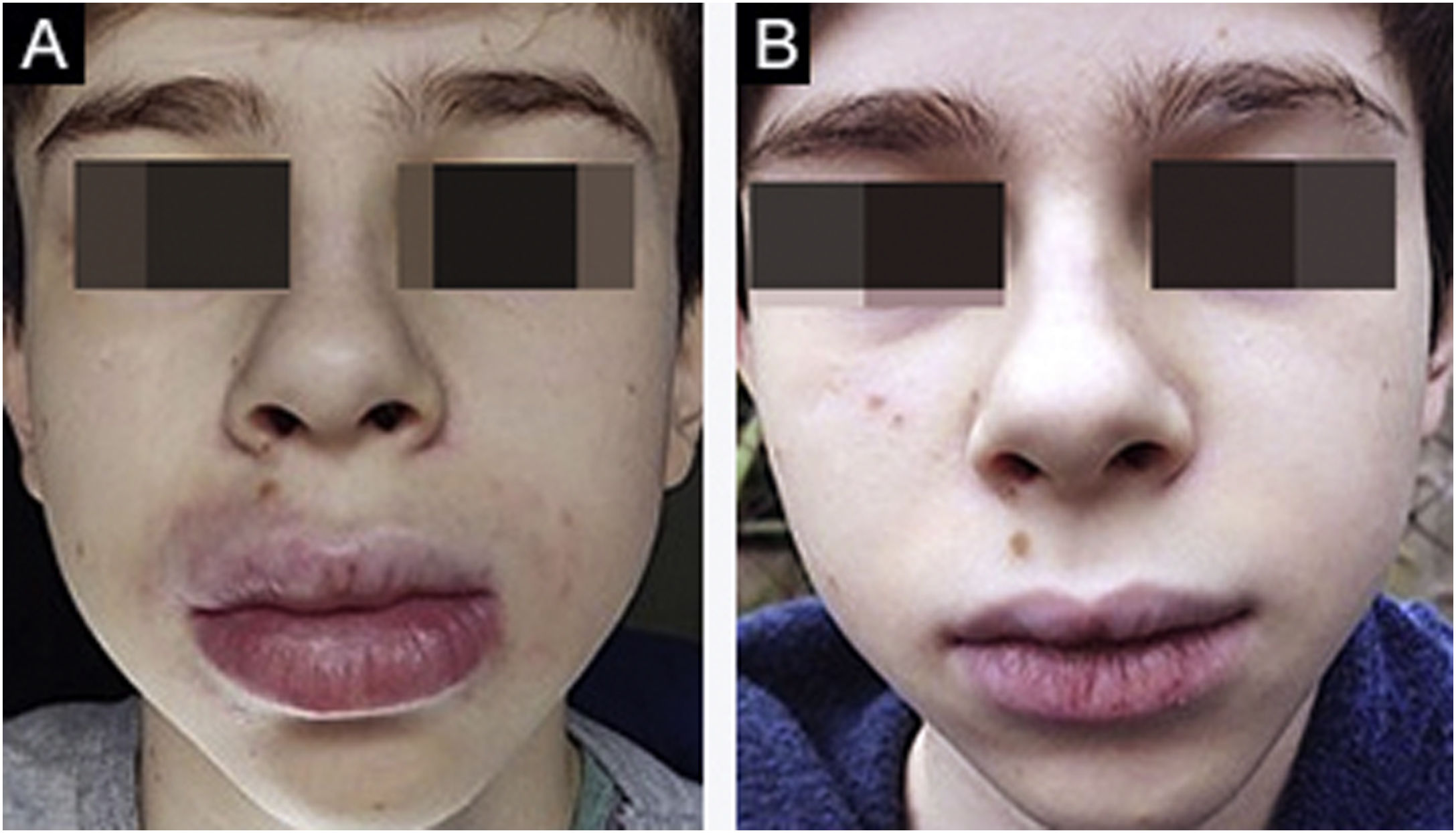
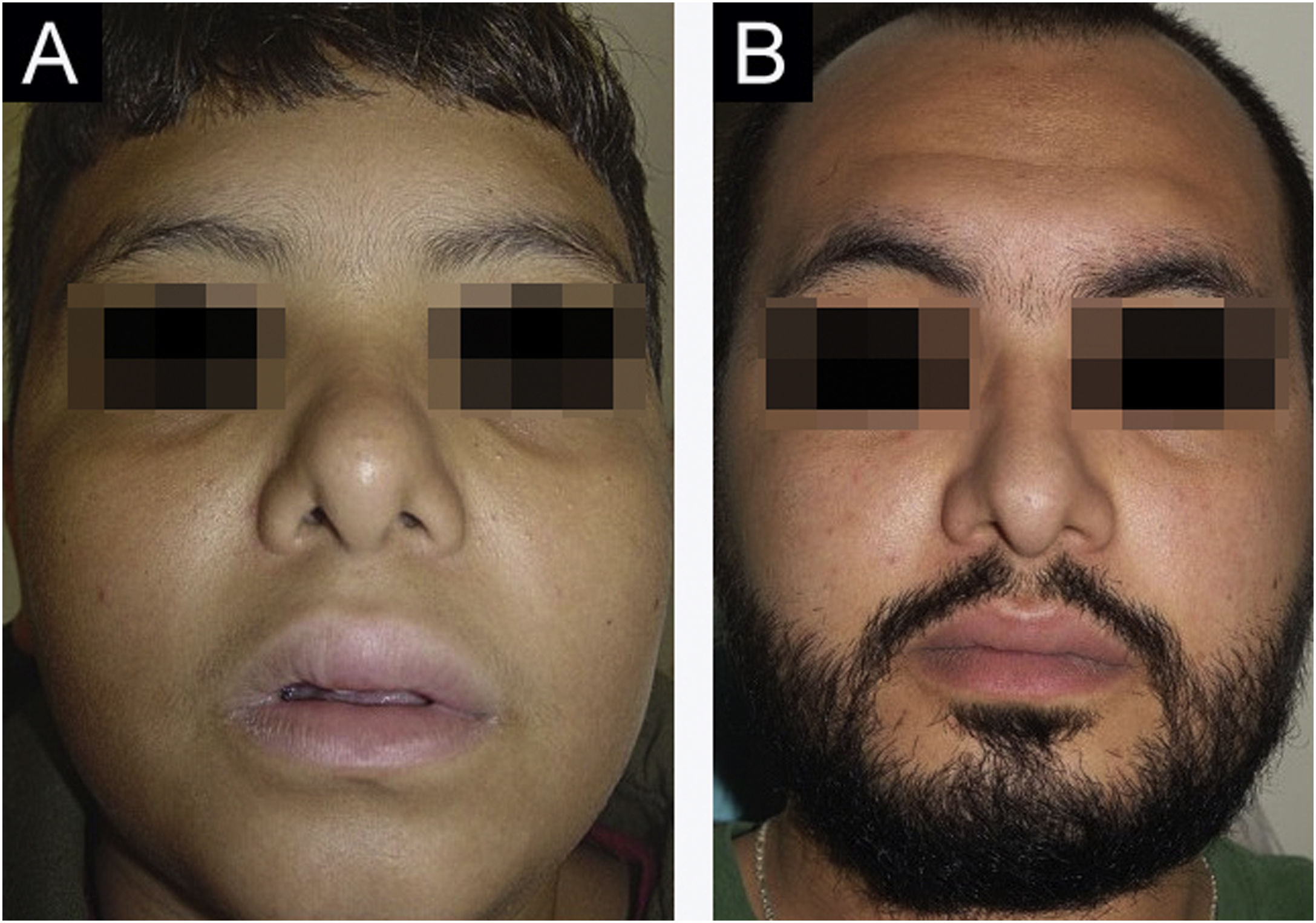
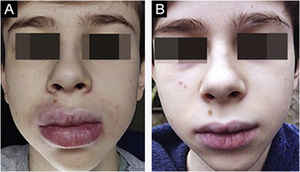
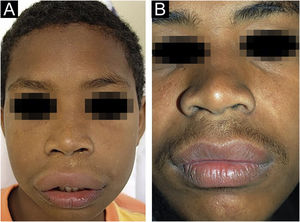
No treatment is effective for all cases of MRS; there are no controlled studies. There are no clinical elements that indicate the choice of a particular drug. It is believed that the selected drug should be used for at least three months before being considered a failure, as the response is slow. The authors’ preferred drug is thalidomide, based on their experience with adult patients.9 Five patients received thalidomide and two received dapsone. Only one patient (Case 6) showed significant improvement with thalidomide. Patient 1 is slowly improving after one year of follow-up. Cases 4 and 5 only improved when they became adults, despite treatment with different drugs. It is not known whether the improvement occurred due to the last drug used or if it occurred spontaneously. Case 3 showed a good response to dapsone; some subsequent recurrences were controlled with short cycles of oral corticosteroids (Fig. 2A‒B). Case 4, after several attempts, only improved with azathioprine and gingivoplasty (Fig. 3A‒B). Case 5 only improved with surgical treatment (Fig. 4A‒B). Patient 7 was refractory to all therapies and, after several years and crises, was lost to follow-up (Fig. 6A‒B). The authors’ group does not use immunobiologicals, although there are grounds for their use.9–11
Surgical treatment is an option for localized and refractory disease. Three cheiloplasties were performed in Case 5.
Cases 4, 6, and 7 had granulomatous gingival infiltration that has been rarely reported.12 This manifestation should be actively looked for and treated, as it can lead to periodontal involvement. These lesions are resistant to pharmacological treatment; gingivoplasty is an excellent therapeutic option (Fig. 7).
In conclusion, with the exception of Case 2, all the others presented herein were followed for several years, highlighting the variability of their evolution and the difficulty in managing this disease.
Financial supportFAPESP ‒ (2017/26990-8) and FUNADERSP ‒ (29/2016).
Authors' contributionsCamila Fátima Biancardi Gavioli: Statistical analysis; approval of the final version of the manuscript; design and planning of the study; drafting and editing of the manuscript; collection, analysis, and interpretation of data; effective participation in research orientation; intellectual participation in the propaedeutic and/or therapeutic conduct of the studied cases; critical review of the literature; critical review of the manuscript.
Yasmin da Silva Amorim City: Statistical analysis; approval of the final version of the manuscript; drafting and editing of the manuscript; collection, analysis, and interpretation of data; effective participation in research orientation; critical review of the literature.
Giovanna Piacenza Florezi: Design and planning of the study; collection, analysis, and interpretation of data; intellectual participation in the propaedeutic and/or therapeutic conduct of the studied cases; critical review of the literature.
Silvia Vanessa Lourenço: Statistical analysis; approval of the final version of the manuscript; design and planning of the study; drafting and editing of the manuscript; collection, analysis, and interpretation of data; effective participation in research orientation; intellectual participation in the propaedeutic and/or therapeutic conduct of the studied cases; critical review of the literature; critical review of the manuscript.
Marcello Menta Simonsen Nico: Statistical analysis; approval of the final version of the manuscript; design and planning of the study; drafting and editing of the manuscript; collection, analysis, and interpretation of data; effective participation in research orientation; intellectual participation in the propaedeutic and/or therapeutic conduct of the studied cases; critical review of the literature; critical review of the manuscript.
Conflicts of interestNone declared.
Study conducted at the Department of Dermatology, Faculty of Medicine, Universidade de São Paulo, São Paulo, SP, Brazil.