Dear Editor,
Tinea faciei is a relatively uncommon superficial dermatophyte infection limited to the glabrous skin of the face.1 Studies define its classical presentation as single or multiple blemishes and circular erythematous-scaling patches with central clearing.2 On the other hand, clinical manifestations are defined as atypical when the inflammatory component is more severe, presenting follicular papules and pustules.2 When atypical clinical manifestations are present, the disease is known to mimic several disorders, such as cutaneous lupus erythematosus, rosacea, and granuloma annulare.1,3,4 Additionally, treatment with corticosteroids makes its presentation incognito, becoming a great diagnostic challenge.5 We report the case of a patient with follicular tinea faciei incognito, an atypical presentation of the disease, in which the diagnosis required a skin biopsy and successful treatment required the use of systemic antifungals.
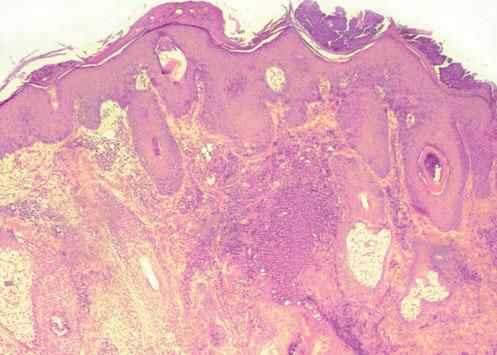
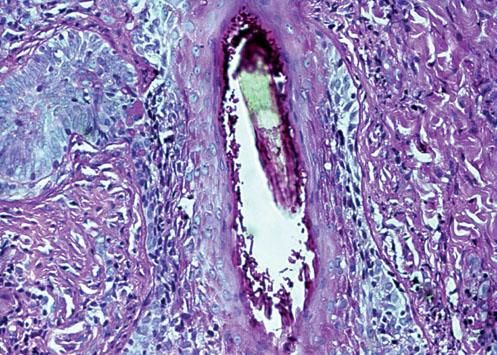
A 31-year-old woman with no relevant medical history was referred to our university hospital with a facial dermatosis that compromised nose, cheeks, periocular region, and forehead. The lesion was characterized by an extensive erythematous and desquamative plaque of about 10 centimeters in diameter in which pustules were found in the central region and an inflammatory edge in the peripherical region (Figure 1). The lesion had appeared 4 months earlier, after the patient underwent a biopsy of a benign nasal nevus. The physical examination revealed no other remarkable findings and there was no evidence of tinea pedis or unguium. The lesion grew progressively until reaching the size described above. The patient received multiple topical treatments, including corticosteroids, antibiotics, and antifungal drugs without obtaining successful results. Laboratory tests showed no relevant information, and serologies for human immunodeficiency virus, hepatitis B and C viruses were non-reactive. Bacterial and fungal cultures of superficial skin were also negative. A deep surgical biopsy was performed, providing biological material for a follicular fungal culture, which was positive for Trichophyton rubrum. Histopathology with hematoxylin-eosin (HE) staining also supported the diagnosis, showing neutrophils within the corneal layer and an extensive inflammatory process -edema, vasodilatation, and a dense lymphohistiocytic infiltrate in the reticular dermis (Figure 2). PAS staining showed abundant septate filaments on the outer layer of the hair shaft compatible with ectothrix follicular tinea (Figure 3). According to these findings, the diagnosis of follicular tinea faciei incognito was confirmed and treatment with oral terbinafine (250 mg/day) was initiated. After eight weeks of treatment our patient showed total regression of the disease with mild post-inflammatory hyperpigmentation.
This clinical case reveals an atypical presentation of tinea faciei indicated by the large size of the lesion and the presence of pustules in the central region. The disease most likely initiated after a physical trauma that served as gateway for the pathogen. In this case, a skin biopsy was necessary to achieve proper diagnosis, as it allowed follicular samples for fungal culture, and a systemic antifungal was required to successfully treat the disease. In conclusion, tinea faciei can be a great diagnostic challenge when there are atypical clinical manifestations as it usually presents a wide variety of symptoms, especially after the application of topical corticosteroids. Thus, the authors recommend that fungal infections should always be suspected in scaly eruptions on the face.