Harlequin syndrome is a rare condition in which one half of the face fails to flush and sweat due to damage of the sympathetic fibers on the ipsilateral side. The majority of cases are idiopathic, but may be iatrogenic or caused by space-occupying lesions or brainstem infarction. We report a case of idiopathic harlequin syndrome in a 34-year-old man with a 5-month history of unilateral facial flushing and sweating after exercise. Despite the rarity of this syndrome, dermatologists should be aware of this condition in order to diagnose properly and provide multidisciplinary assistance.
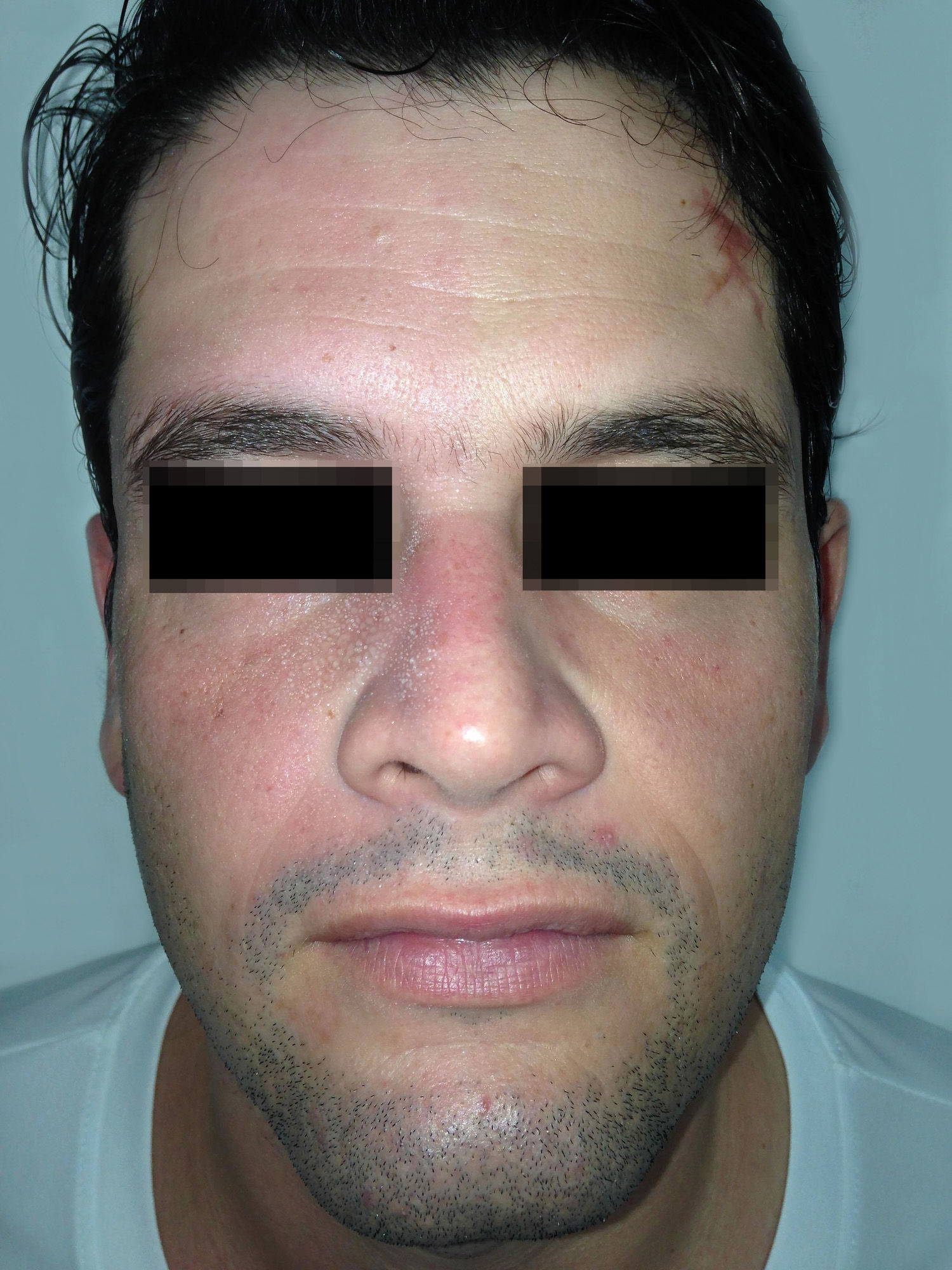
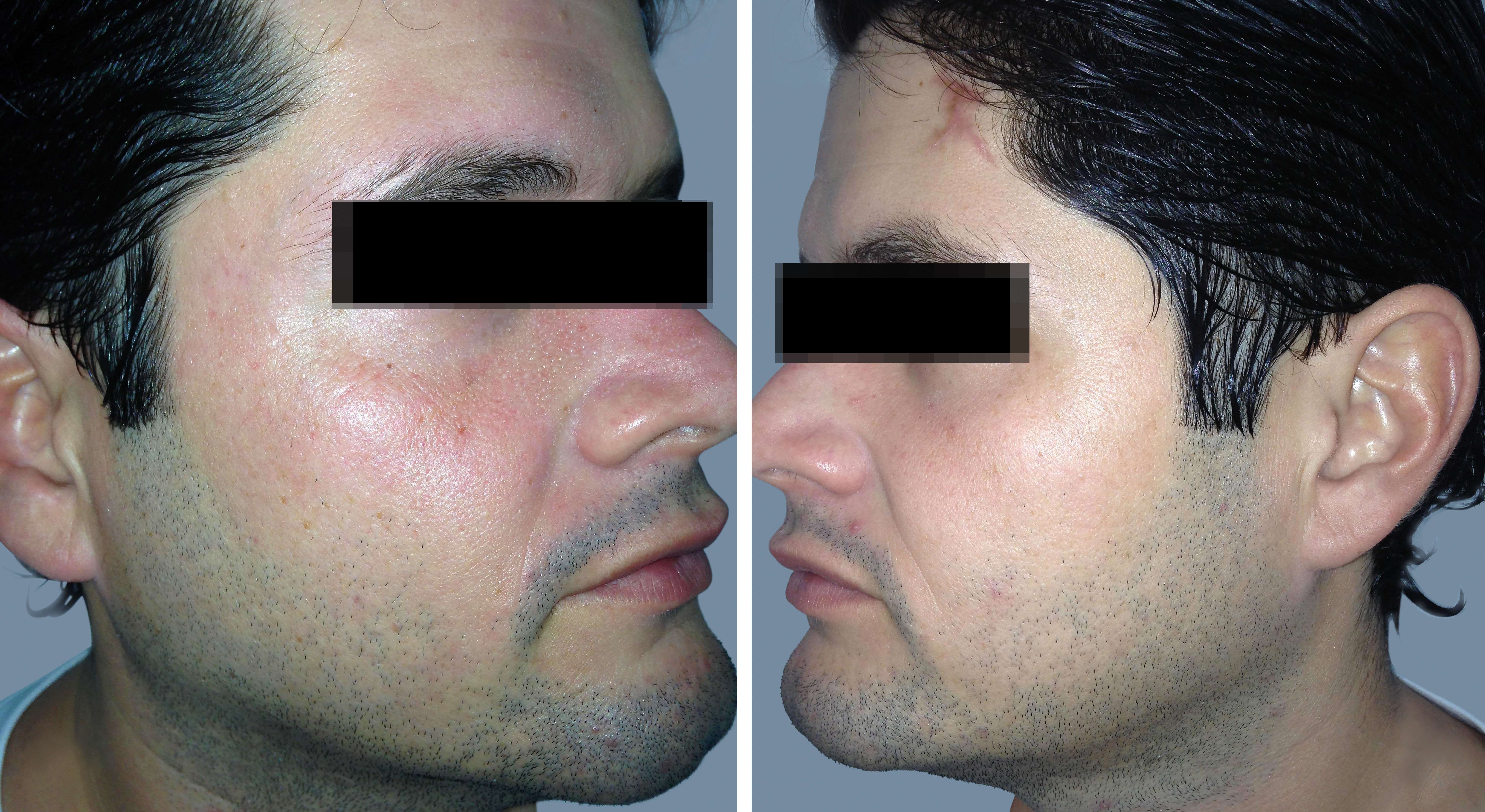
A 34-year-old male patient presented with a 5-month history of unilateral flushing and sweating affecting the right side of his face when submitted to prolonged physical exercise, causing him social embarrassment. These skin changes could be reproduced during examination, a few minutes after exercising, with flushing and sweating (Figure 1). The opposite side of the face remained pale and anhidrotic (Figure 2). No pupil abnormalities were found.
Previous medical history included an anxious personality disorder, which has been treated with medication (escitalopram, sodium valproate, naltrexone and zolpidem). The patient had no other diseases or history of traumatic accidents.
Neurological and ophthalmological evaluations were normal. Magnetic resonance imaging of the head and neck, as well as computed tomography of the chest, were normal. A diagnosis of idiopathic harlequin syndrome was made.
DiscussionHarlequin syndrome, first described by Lance et al. in 1988, is a term reserved for patients with an autonomic disturbance due to an hemifacial cutaneous sympathetic denervation,1,2 leading to unilateral anhidrosis and reduced or absent facial flushing on the affected side of the face.2 Paradoxically, patients present with compensatory flushing and sweating on the unaffected, sympathetic innervated side of the face.3 Arms and trunk may also be affected. Although rare, it is a remarkable disease.2
In patients with hemifacial cutaneous sympathetic denervation, heat stress, exercise, or sudden emotion may elicit a dramatic alteration in facial appearance, in which a distinct line divides the denervated, pale, and dry half from the intact, red, and moist half.1,4
Oculosympathetic paresis may be associated but is not always present.2 The literature lacks consensus regarding what, if any, pupillary abnormalities belong with the diagnosis of harlequin syndrome.4 Although most patients have normal pupils, the abnormality most frequently described by Bremner and Smith is Horner syndrome, characterized by ptosis, miosis and enophthalmus.2
The majority of cases of this rare condition are primary in nature. In about one-sixth of the patients, however, the disorder is caused by an underlying disease or a structural lesion (i.e., secondary harlequin syndrome). The iatrogenic type, occurring after surgical procedures, has been reported with an increasing frequency.5 The neurological damage can occur anywhere along the sympathetic outflow to the face.1,3
The syndrome is most common in women, and social embarrassment is the main complaint of the affected individuals.5 Thorough investigation is required to rule out underlying structural lesions, some of which may require surgical correction.1,3
Most patients do not require medical or surgical treatment unless there is an underlying disease. Where embarrassment is significant and there is a need for psychological support, contralateral sympathectomy should be considered.1,2
Despite the rarity of harlequin syndrome, dermatologists should be aware of this condition in order to diagnose properly and provide multidisciplinary assistance.
Financial support: None.
Conflict of interest: None.