Inflammatory breast cancer is an aggressive and infiltrative malignancy that is often misdiagnosed as an infection because of its symptoms and signs of inflammation, delaying proper diagnosis and treatment. We report a case of inflammatory breast cancer showing correlation between dermoscopic and histopathological diagnoses. We highlight the utility of dermoscopy for skin biopsy site selection.
A 46-year-old woman with personal history of schizophrenia consulted for an erythematous plaque with diffuse borders covered by grouped translucent papular lesions and some rounded erosions on the inferior and external aspects of the left breast for 6-months (Figure 1). She had been using topical antibiotics and steroids on the lesions for months without medical prescription. Physical examination revealed an underlying 4-cm indurated nodule on the lower portion of the breast and other nodules of similar characteristics on the left axilla.
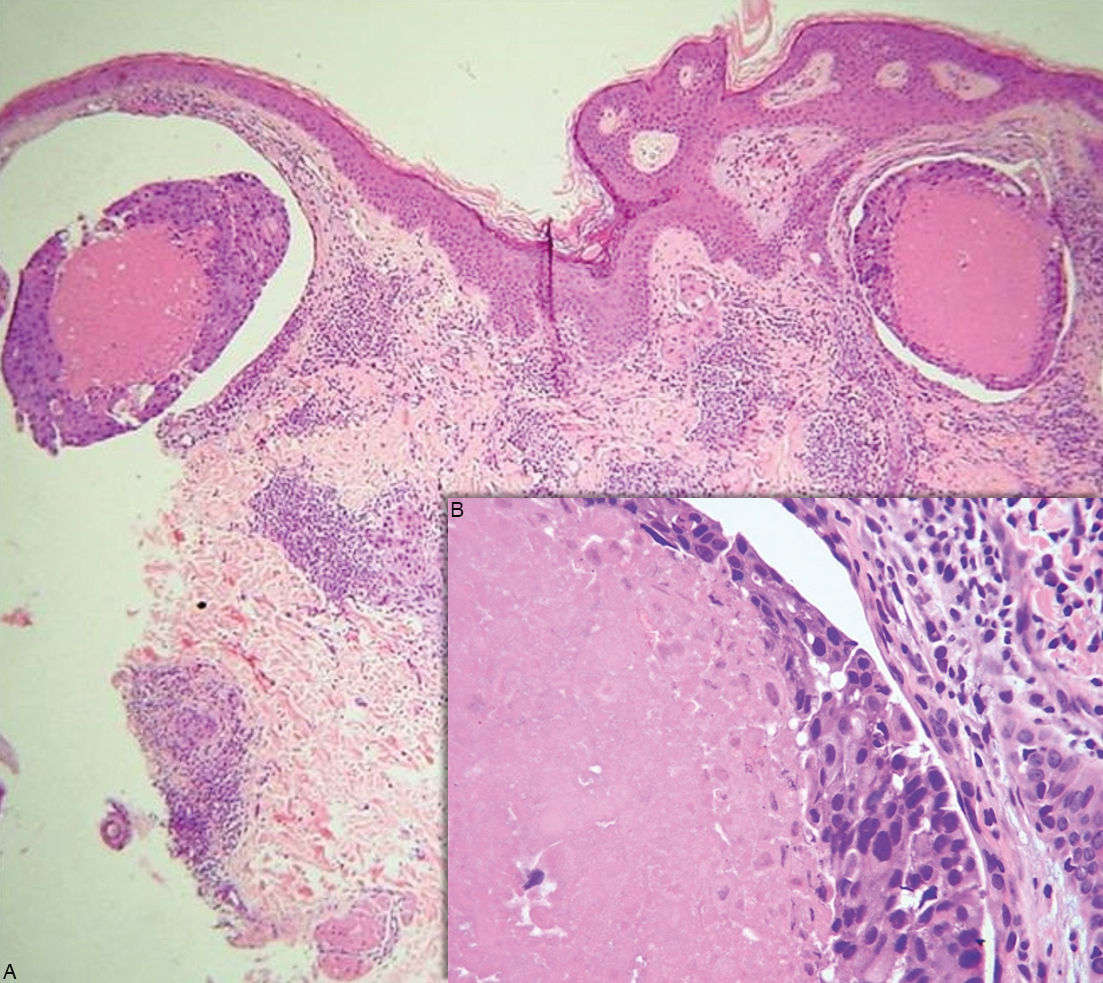
Dermoscopy showed multiple grouped white-to-yellow rounded milia-like cysts over an erythematous background and irregular linear vessels over and between them (Figure 2). A skin biopsy of one of these milia-like cysts was performed. Microscopic examination showed multiple dermal intralymphatic emboli of a primary comedo-type ductal breast carcinoma (inflammatory carcinoma). Therefore, we reached the diagnosis of inflammatory breast cancer (IBC) (Figure 3).
Breast nodules and axilla lymph nodes were biopsied confirming the diagnosis of invasive ductal carcinoma of the left breast with axillary lymph node involvement. Both samples were positive for hormone receptors and negative for human epidermal growth factor receptor 2 (HER2). Computed tomography revealed lung and liver metastasis. Systemic chemotherapy consisting of doxorubicin and cyclophosphamide was indicated.
IBC is a rare and very aggressive type of locally advanced breast cancer with a poor prognosis.1,2 Patients present with rapid onset of erythema and edema of the breast skin (peau d’orange).2 Because of its clinical signs and symptoms, sometimes IBC is misdiagnosed as a bacterial infection. It also may be misdiagnosed as mastitis, abscess of the breast, metastasis from another cancer, postradiation dermatitis, or even breast edema from congestive heart failure. Presumptive diagnosis of cellulitis or mastitis and treatment with a trial of antibiotic therapy is the leading cause of delay in diagnosis and treatment of IBC and can be deadly.3
Minimum criteria required for the diagnosis of IBC include the following: rapid onset of breast erythema, edema and/or peau d’orange, and/or warm breast, with or without an underlying palpable mass; duration of history of no more than 6 months; erythema occupying at least one-third of the breast; and pathological confirmation of invasive carcinoma.4
The inflammatory skin changes of a breast afflicted with IBC represents the presence of dermal lymphatic invasion (DLI), a state in which dilated dermal lymphovascular spaces are filled with tumor emboli that are often retracted away from the surrounding endothelial lining.4,5 Considered to be a histological hallmark of IBC, DLI subsequently leads to lymphatic obstruction and is ultimately responsible for the highly metastatic potential of IBC.4,5 Therefore, although pathological evidence of dermal lymphatic involvement is not considered a definitive diagnostic criterion for IBC, it is strongly recommend that every patient who meets the diagnostic criteria for IBC undergo at least two skin punch biopsy.4 This helps not only determining the presence of DLI but will also help in confirming the diagnosis of an invasive carcinoma in the absence of an underlying intraparenchymal lesion or regional metastases.4
As shown in the present case, the milia-like cysts revealed by dermoscopy correlated with DLI. Therefore, the identification of these dermoscopic structures, when present, could be an aid for accurate clinical diagnosis and also a useful guide for skin biopsy, avoiding sampling errors.
To the best of our knowledge, this is the first report that describes the clinical-dermoscopic-histopathological correlation of the DLI characteristic of IBC.
Financial support: None.
Conflict of interest: None.