Pigmented lesions on acral sites are common; clinical differentiation of nevi and early melanoma can be challenging. In these cases, dermoscopy can provide a more accurate diagnosis. Most dermoscopic patterns on acral skin have been described in Asian and European populations, while there are few studies in Latin American populations.
Objectives:To determine the frequency of pigmented lesions in volar skin and their dermoscopic patterns in a Mexican population. Methods: An observational, descriptive, cross-sectional study was performed in Hispanic patients with the presence of at least one pigmented lesion on acral skin. Clinical and dermoscopic images were obtained. These were subsequently evaluated independently by two dermatologists trained and experienced in dermoscopy.
Results:A total of 582 pigmented lesions on volar skin were diagnosed in 321 patients. Overall, prevalence of acral pigmented lesions on volar skin was 6.8%. For both observers, parallel furrows were the most frequent pattern described, but for observer 2, a lattice-like pattern was prevalent on the toes and a homogeneous pattern on the sides of the feet. There was lower inter-observer agreement, with a kappa index of 0.144.
Study limitations:The lesions were not biopsied, so clinical-histological correlation could not be performed. The study did not correlate dermoscopic patterns with age.
Conclusions.As previously reported by other authors, parallel furrows were the most frequently found dermoscopic pattern on palmoplantar skin.
Pigmented lesions on acral areas are common and can have different etiologies: skin trauma, post-inflammatory pigmentation, lentigo simplex, melanocytic nevus, and cutaneous melanoma.1-3 The differential diagnosis with incipient cutaneous melanoma is often challenging and has increased with this tumor’s growing incidence.4 From the 1950s to the 2000s, the total number of melanoma cases increased by 619% in the United States.5 There are no precise epidemiological data in Latin America. Estimates from the International Agency for Research on Cancer show incidence rates from 0/100,000 inhabitants in Belize to 7.6/100.000 inhabitants in Uruguay.6 In Mexico, the Instituto Nacional de Cancerología (INCAN) reported a 500% increase in incidence in recent years, based on retrospective data from the Histopathological Registry of Malignant Neoplasms, plus an estimated overall incidence of melanoma of 1.01/100,000 inhabitants.7,8
Palmoplantar melanocytic nevi are common, thus emphasizing the importance of knowledge of the characteristics that differentiate them from melanoma in the same region.9 Dermoscopy (epiluminescence microscopy, surface microscopy) is a non-invasive in vivo test used to study pigmented skin tumors, allowing to increase the diagnostic sensitivity and specificity of cutaneous melanoma.10,11
The clinical and dermascopic features of acral pigmented lesions have been obtained from European and Asian populations.2-4,12,13 The current study aimed to identify the dermascopic features of melanocytic lesions located on the palmoplantar region in the Latin American population of Mexico. We describe the dermascopic patterns found by two observers with experience in dermoscopy and determined the frequencies and inter-observer agreement.
MethodsThis was an observational cross-sectional study that included Hispanic patients up to 99 years of age with palmoplantar melanocytic lesions.
Patients were seen at the Dermatology Outpatient Clinic of Hospital Universitário Dr. José Eleuterio González in Monterrey, Mexico from June to August 2014. The study sample excluded patients with acral pigmented lesions with dermoscopic features of acral lentiginous melanoma (ALM), as well as subungual lesions.
The sample also excluded patients with a history of use of immunosuppressants (azathioprine, biological agents, prednisolone, methotrexate, mofetil mycophenolate), current or previous use of alpha-MSH (Melanotan®), human immunodeficiency virus (HIV) infection, organ transplants, phototherapy, acral skin burns, palmoplantar involvement in psoriasis, pityriasis rubra pilaris, Stevens-Johnson syndrome, erythema multiforme, and bullous diseases.
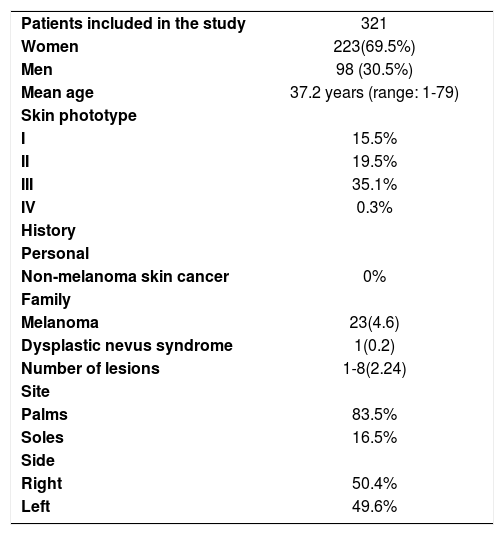
The clinical and demographic data obtained for the patients included in the study were expressed as percentages: age, sex, skin phototype, personal history of melanoma or non-melanoma skin cancer, presence of dysplastic nevus syndrome, number of melanocytic lesions, site, and dermoscopic pattern (Table 1).
Demographic characteristics of the study population
| Patients included in the study | 321 |
| Women | 223(69.5%) |
| Men | 98 (30.5%) |
| Mean age | 37.2 years (range: 1-79) |
| Skin phototype | |
| I | 15.5% |
| II | 19.5% |
| III | 35.1% |
| IV | 0.3% |
| History | |
| Personal | |
| Non-melanoma skin cancer | 0% |
| Family | |
| Melanoma | 23(4.6) |
| Dysplastic nevus syndrome | 1(0.2) |
| Number of lesions | 1-8(2.24) |
| Site | |
| Palms | 83.5% |
| Soles | 16.5% |
| Side | |
| Right | 50.4% |
| Left | 49.6% |
Each pigmented lesion was examined with a DermLite II Pro HR polarized light dermatoscope (3Gen, San Juan Capistrano, CA, USA). A clinical photographic and dermoscopic record was taken with an HP Photosmart R 707 5.1 MP digital camera (Hewlett-Packard Development Company, LP, Palo Alto, CA, USA). The palms were divided anatomically into five areas: thenar, hypothenar, mid-palmar, volar surface of fingers, and lateral surfaces of hands. The soles were divided as follows: plantar arch, volar surface of toes, heel, metatarsal heads, and sides of feet.
The resulting clinical and dermoscopic images were evaluated independently by two dermatologists with experience in dermoscopy (RG and VG), who analyzed and classified the lesions according to the predominant dermoscopic pattern.
The dermoscopic findings were classified in nine different patterns, as described previously in the literature: parallel furrow pattern (PFP), fibrillar, nontypical, lattice-like, homogeneous, globular, reticular, reticulo-globular, and transition.12,13 Data were expressed as means, frequencies, and percentages. The McNemar test was used to compare proportions between observers. Kappa index was calculated as the measure of inter-observer agreement. Statistical significance (alpha value) was set at 5%. Statistical analysis used Microsoft Excel 2013 (Microsoft, Redmond, Washington, USA).
ResultsA total of 4,718 patients with various skin conditions, including those different from the ones included in the study, were evaluated at the Dermatology Outpatient Clinic. Of these patients, 321 (6.8%) had palmoplantar pigmented lesions. From this population, a total of 582 pigmented lesions were evaluated clinically and dermoscopically. Eighty images from 21 patients were excluded due to their low photographic quality. One lesion was excluded from the study because the image presented dermoscopic features of ALM, later confirmed by histopathological examination. The final data resulted in a total of 300 patients with 502 acral melanocytic lesions. Table 1 shows the demographic data.
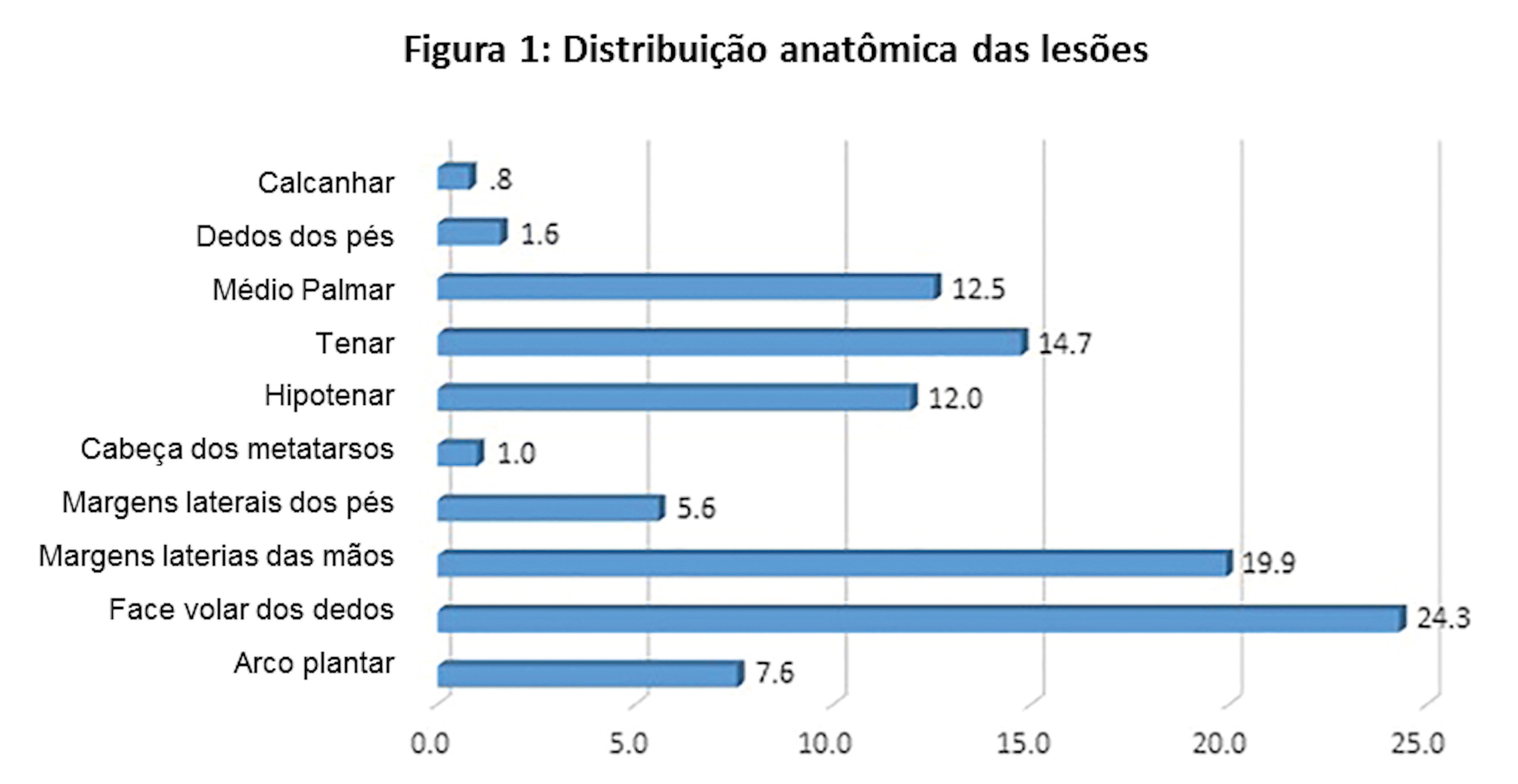
As for the anatomical location, the majority of the lesions were located on the volar surface of the fingers (24.3%), followed by the sides of the hands – Wallace line (WL) (19.9%); thenar region (14.7%), hypothenar (12.0%), mid-palmar (12.5%); plantar arch (7.6%), sides of feet - WL (5.6%), volar surface of toes (1.6%), metatarsal heads (1%), and heel (0.8%) (Figure 1).
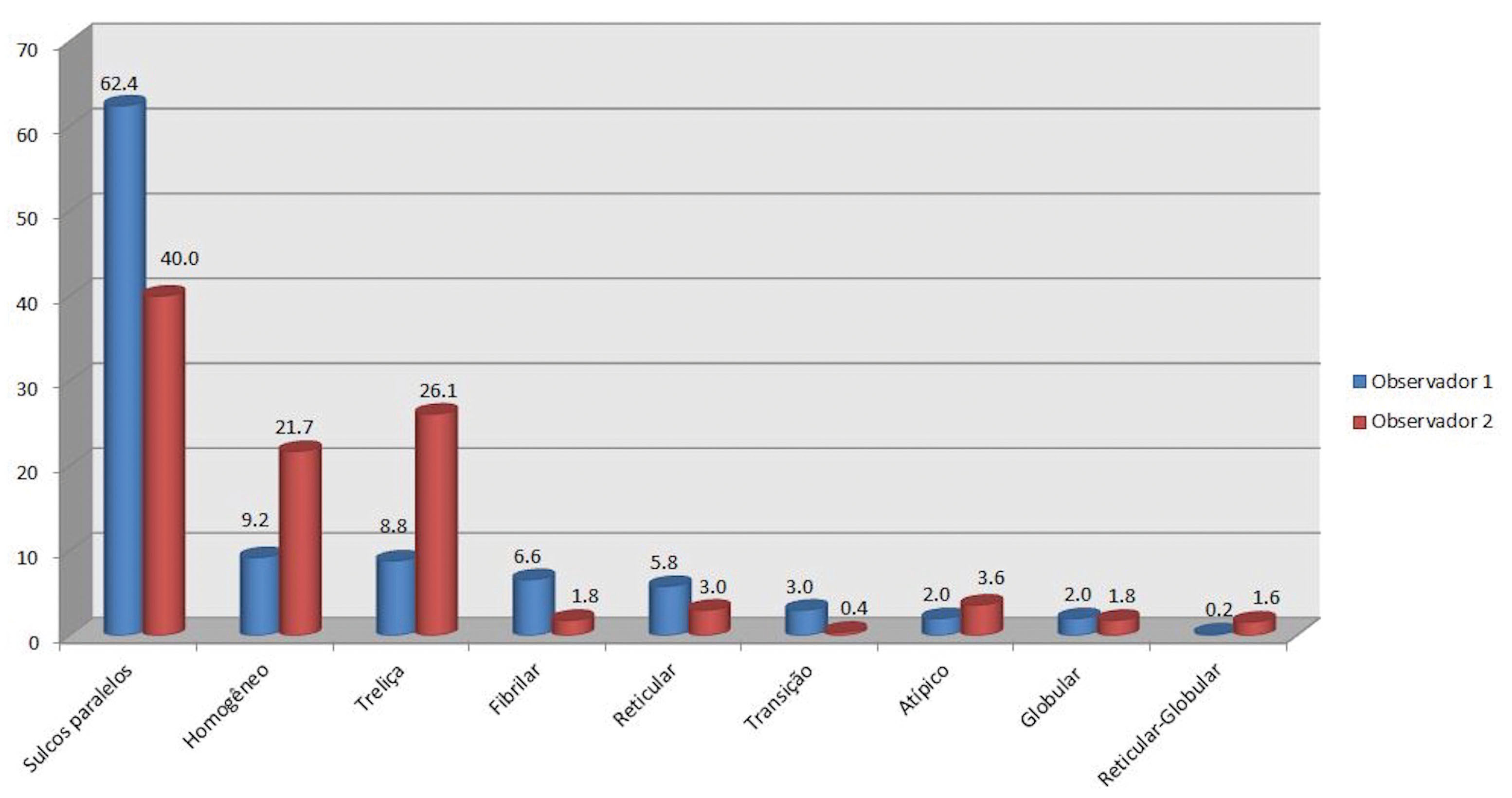
Dermoscopic patternsThe predominant patterns found by observer 1 were: PFP (62.4%), homogeneous (9.2%), lattice-like (8.8%). fibrillar (6.6%), reticular (5.8%), transition (3%), nontypical (2%), globular (2%), and reticulo-globular) (0.2%). When the lattice-like and fibrillar patterns are included as variants of PFP (model 2), the proportion of lesions classified as PFP increases to 77.8%, followed by the homogeneous (9.2%) and reticular (5.8%) patterns.
According to observer 2, the predominant patterns were: PFP (40%), lattice-like (26.1%), homogeneous (21.7%), nontypical (3.6%), reticular (3.0%), fibrillar (1.8%), globular (1.8%), reticulo-globular (1.6%), and transition (0.4%). When lattice-like and fibrillar are included as variants of PFP (model 2), the distribution is as follows: PFP (67.9%), homogeneous (21.7%), nontypical (3.6%), reticular (3%), retículo-globular (1.6%), and transition (0.4%).
For both observers, PFP predominated on the various anatomical sites, but according to observer 2, the lattice-like pattern predominated on the toes and the homogeneous pattern on the sides of the feet (Figure 2).
As mentioned, PFP was the most frequent dermoscopic pattern according to both observers. When the lattice-like and fibrillar patterns were included as variants of PFP, the homogeneous pattern was the second most frequent. The third most common pattern was reticular (5.8%) for observer 1 and nontypical (3.6%) for observer 2.
When PFP was subdivided (pure PFP, lattice-like, and fibrillar), there was slight agreement (39.8%) between the observers, with a kappa index of 0.144; however, when the fibrillar and lattice-like patterns were classified as variants of PFP, the agreement increased to 64.5%, with a kappa of 0.204. These data are acceptable, according to Landis and Kochs.14
When analyzed by anatomical site, the most frequent pattern on the hands according to both observers was PFP, followed by lattice-like and homogeneous. However, observer 1 classified more lesions as PFP (65.4%) when compared to observer 2 (41.1%). This difference was statistically significant (p=0.017). Observer 2 classified more lesions as lattice-like (28.6%) and homogeneous (19.8%), compared to observer 1 (9.1% and 6.9%, respectively), which was also statistically significant (p<0.05%).
No statistically significant difference (p> 0.05) was seen in the classification of lesions on the soles. PFP was the most frequent pattern, followed by the homogeneous and lattice-like patterns.
DiscussionAcral lentiginous melanoma (ALM) is the most common variant of melanoma in the non-white population (Asians and African Americans). Radial growth is the predominant component in this type of neoplasm, which may explain why changes in the size of pigmentation are the first sign noticed by patients and physicians. ALM is frequently located on the palms, soles, and nails, most specifically on the nails of the halluces and thumbs.15 Incidence is estimated at 0.3 cases per 100,000 inhabitants/year, accounting for an estimated 4.5-7% of all melanomas.16,17 In the black population, ALM accounts for 50-70% of cases.18 In Mexico, 24-31% of melanomas are acral lentiginous.7 A previous study by De la Fuente et al.19 reported 23% prevalence of ALM cases in our outpatient clinic.
One of the main challenges in daily dermatology practice is early diagnosis of cancers on clinical examination, which is difficult even for experienced dermatologists. Dermoscopy increases the diagnostic accuracy of malignant melanocytic lesions, and the different dermoscopic patterns allow the identification of benign lesions, avoiding unnecessary biopsies.2-4,12,13,20-23
The aim of this study was to determine the prevalence of palmoplantar pigmented lesions. We also sought to determine whether the palmoplantar patterns described in our population were similar to those in other populations. Finally, we assessed the correlation between the dermoscopic findings of two experienced observers.
For both observers, the predominant dermoscopic pattern was PFP (62.4% for observer 1 and 40% for observer 2), similar to the findings in other studies (42-59%).13,22,24,25 For observer 1, the second most frequent pattern was homogeneous (9.2%). This pattern has not been reported as the second most frequent one on volar skin. For Ozdemir et al.25, the homogeneous pattern was only present in 6.4% of the cases studied. The third most frequent pattern for observer 1 was lattice-like (8.8%). For observer 2, the second most common pattern was lattice-like, found in 26.1% of the cases. The frequency of this pattern in our study (26.1%) was higher than in other studies (13-15% of cases).2,13,22 The homogeneous pattern was the third most frequent. These data are very similar to those of Elwan et al., who detected PFP in 66.1% of cases, followed by the lattice-like pattern (8.9%) and the homogeneous pattern (7.6%).26
Inter-observer agreement was low, with a kappa index of 0.144. The explanation may be that there was a statistically significant difference between the observers in classifying the lesions. For example, observer 1 classified more lesions as PFP (62.5%), while observer 2 classified more lesions as lattice-like (26.1%) and homogeneous (21.7%).
When disaggregating by anatomical sites, the two observers differed in their classification of palmar lesions. Observer 1 found the following frequencies: PFP 65.4%, lattice-like 9.1%, and homogeneous 6.9%. Observer 2 found 41.1%, 28.6%, and 19,8%, respectively. The difference was statistically significant. There was no statistically significant difference on the plantar region. There was no statistically significant distribution of dermoscopic patterns within the plantar region. Miyazaki et al. found the majority of lattice-like nevi on the plantar arch.27
The low inter-observer agreement may have been due to classification bias, since some nevi can display a combination of two or three patterns in the same lesion. Thus, the classification criterion may have varied according to the observer.21 Observer 1 classified more lesions than observer 2 as PFP. This may be explained by the fact that the fibrillar and lattice-like patterns are variants of PFP, which would hinder discrimination between these patterns. Braun et al. observed a low level of agreement in difficult or challenging lesions.28
The transition pattern described by Altamura et al.22 consists of a combination of a brownish black network in an area of the lesion with parallel furrows or fibrillar pattern in another part of the lesion. It is observed mainly on the sides of the fingers, where the volar skin becomes glabrous. Observer 2 in our study identified these same results, with lesions classified as transition pattern on the sides of the fingers.
One limitation to our study was that no biopsies were performed, thus impeding any clinical-histopathological correlation. Another limitation was that no correlation was performed between the different dermoscopic patterns and age. Minagawa et al. reported a significant correlation between the frequency of dermoscopic patterns and age.29 In their study, the fibrillar and “peas-in-a-pod” patterns (described in acral congenital nevi) were significantly prevalent in individuals under 20 years of age. The nontypical pattern was prevalent in the group over 59 years of age. No significant differences were observed in the frequency of PFPs in the different age brackets.29
The current study is one of the few that not only identifed the dermoscopic features of palmoplantar lesions, but also studied their prevalence jointly and separately in a large population of patients. We found a prevalence of 6.8%, similar to that reported in other studies, ranging from 6% to 8%.2,22 A recent study published by Madankumar R30, with cases from a highly heterogeneous population in New York and Miami, found a prevalence of 36%, far higher than previously reported. This may have been due to the inclusion of patients with skin phototypes V and VI, who are more prone to presenting pigmented lesions on the volar skin.30
We found a similar prevalence to that reported in populations from Europe and Japan, with predominantly fair-skinned individuals. In our study, 35.4% of the patients had skin phototypes III and IV, showing that phototype does not influence the frequency of dermoscopic patterns on palmoplantar skin. Our findings are very similar to those reported in the Latin American literature, but we also determined the correlation in dermoscopic patterns between the two observers.21
As mentioned previously, ALM is a particular subgroup of melanoma, rare and potentially fatal, which requires specific treatment.31 Performing dermoscopy in all patients with pigmented lesions on the palmoplantar region could make all the difference in prognosis.
ConclusionOur study found very similar numbers to those from previously published studies. The prevalence of palmoplantar lesions in the Mexican population is similar to that reported by other authors. The parallel furrow pattern was also the most common pattern on acral skin.
Financial support: None.
Conflict of interest: None.