Dear Editor,
Melanoma is a cancer that has great importance due to its aggressive and invasive features of tissues and organs, being the main cause of death by skin-related diseases. It arises from melanocytes, skin cells responsible for the production of melanin mainly as a result of the ultraviolet radiation (UV).1
Ocular melanoma (OM) is a primary intraocular malignant tumor, more common in adults. It is a primary neoplasm in the majority of cases but can occur as metastasis from a primary cutaneous site. It presents in two forms: uveal and conjunctival, the former being the most frequent.2
The uveal form is characterized by pigmented dendritic cells in a variable shape that are distributed in the iris’s stroma, ciliary body and choroid. The conjunctival form has spindle-shaped and polyhedral pigmented epithelioid cells with the presence of intrusive and feeding vessels, commonly located in the bulbar conjunctiva.2
Diagnosis is made with ophthalmoscopy and digital returography but the confirmation is with histological analysis of the lesion.3
Treatment depends on the size of the tumor, of the presence of extraocular and/or systemic involvement, of the condition of the contralateral eye, of the patient’s age, among other factors.3
A female 71-year-old Caucasian patient, housewife, had a lesion detected in the nasal conjunctiva of the right eye during a routine consultation with the ophthalmologist, which was growing quickly for about 1 year. The lesion was brown, had irregular borders, smooth surface and was elastic, measuring approximately 1.0×0.5×0.4cm.
The patient had hypertension and diabetes, was using metformin, acetylsalicylic acid, atenolol, losartan, hydrochlorothiazide and simvastatin. She denied alcohol intake or smoking and confirmed frequent exposure to UV radiation. She reported family history of breast cancer and skin cancer.
The lesion was biopsied with the diagnostic hypothesis of melanoma. Histopathology revealed a pigmented, epithelioid malignant neoplasm, consistent with the diagnosis of conjunctival melanoma, confirmed by immunohistochemistry with the positivity for the markers HMB45, Melan A, Ki-67 and protein S-100 in neoplastic cells.
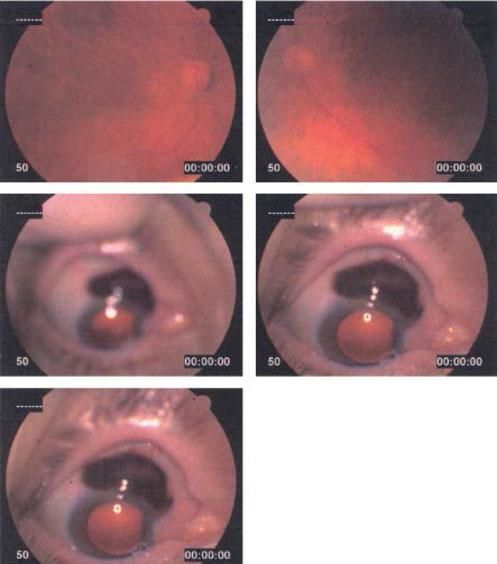
The patient was referred to the specialized center AC Camargo for a more thorough evaluation of the case. Digital retinography and ultrasound biomicroscopy demonstrated a homogeneous well-defined lesion close to the limbus, with medium reflectivity, extending over the cornea and with conjunctival thickening over the peripheral cornea, suggestive of fibrovascular proliferation (Figures 1 and 2).
Treatment was surgical, with the removal of the right eyeball and adjacent tissues. Histopathologic examination of the surgical specimen demonstrated conjunctival melanoma, pT3 staging, with metastases for the palpebral and nasal subconjunctival regions, near the caruncle, associated to conjunctivitis and chronic dacryoadenitis; the margins were not affected. Systemic investigation did not show signs of distant metastases. She was discharged from hospital and continues being followed up as an outpatient.
According to the literature, the incidence of OM is of approximately 4 to 6 cases per million people, with uveal melanoma the most common of intraocular melanomas. They are more frequent in men of 50 to 70 years of age and is uncommon in dark-skinned people. Conjunctival melanoma is the least frequent, representing only 2% of malignant neoplasms in the world and its annual incidence in the Western countries is between 0.2 and 0.5 per 1,000,000 people. It is even rarer in children, with only 29 cases described in the literature.4
Approximately half of patients with OM develops metastatic disease within the first five years after treatment. Conjunctival melanoma is more aggressive, with a rate of metastasis of 16% in five years and 26% in ten years of follow-up, with a mortality rate of 12% to 20% in five years and 30% in ten years.5
Metastases of conjunctival melanoma occur through lymphatic and hematogenous spread but they can also directly affect the eyeball, orbit and sinuses. Prognosis is very poor for patients with advanced disease with the mean survival of approximately eight months.5
As prevention, any melanocytic lesion in the conjunctiva should be removed. In the case of extensive lesions, these should be closely followed and, if there is any change, intervention should be immediate. Thus, an important role of the dermatologist is to carefully examine not only the skin, but also mucous membranes and, in case a melanocytic lesion is detected in the conjunctival mucosa, advise the patient to see an ophthalmologist for a more thorough examination. This practice avoids mutilating surgeries and saves the patient’s life.
Financial support: None.
Conflict of interest: None.