In spite of the frequency of chronic urticaria, there are no epidemiological studies on its prevalence in Argentina.
ObjectiveThe objective of this study was to define the prevalence and epidemiological characteristics of chronic urticaria patients in Buenos Aires.
MethodsThe population studied were the members of the Italian Hospital Medical Care Program, a prepaid health maintenance organization located in the urban areas around the Autonomous City of Buenos Aires, Argentina. All patients with diagnosis of chronic urticaria members of the Italian Hospital Medical Care Program, and with at least 12 months of follow up were included in the study. All medical records obtained between January 1st, 2012 and December 31, 2014 were analyzed. The prevalence ratio for chronic urticaria per 100,000 population with 95% CI for December 31, 2014 was calculated. The prevalence rate for the entire population and then discriminated for adults and pediatric patients (less than 18 years old at diagnosis) was assessed.
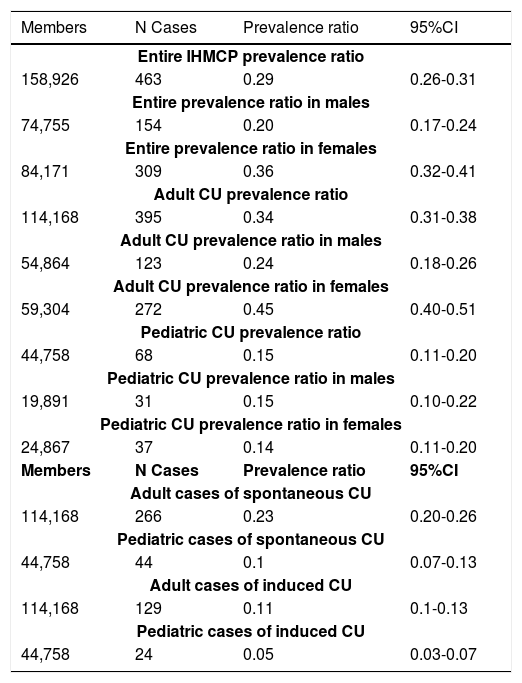
Results158,926 members were analyzed. A total of 463 cases of chronic urticaria were identified on prevalence date (68 in pediatrics, 395 in adults), yielding a crude point prevalence ratio of 0.29% (CI 95% 0.26-0.31%). The observed prevalence of chronic urticaria in the adult population was 0.34 % (95% CI 0.31-0.38%), while in pediatrics it was 0.15 % (95% CI 0.11-0.20%).
Study limitationsthe main weakness is that the results were obtained from an HMO and therefore the possibility of selection bias.
Conclusionschronic urticaria is a global condition. Its prevalence in Buenos Aires is comparable with other countries.
Chronic urticaria (CU) is a common condition of the skin defined by the presence of wheals, angioedema or both daily or almost daily for more than six weeks.1 The condition affects approximately between 0.5 and 1% of the total population with a predominance in females and, in general, all age groups as well as all socioeconomic classes of the population can be affected.2,3 An incidence peak has been found in the third and fourth decades with a lifetime prevalence ratio of 8.8% (95% CI 7.9–9.7%) for all types of urticaria.2,4 The condition is one of the most frequent causes of ambulatory consultation in daily clinical practice for allergists, dermatologists and general practitioners.5 It has been reported 0.27 - 2.1% in family practice consultation, 1- 4% in dermatological outpatient department and > 10% were identified in preselected patients in allergy or dermatology clinics.6,7 The duration of the disease in adults is variable and long lasting: 6–12 weeks in 52.8%, 3-6 months in 18.5%, 7-12 months in 9.4%, 1-5 years in 8.7%, and over 5 years in 11.3% of the patients.1,2
CU types include spontaneous chronic urticaria and inducible urticaria. Spontaneous chronic urticaria shows lesions that are not triggered by consistent or identifiable environmental factors while induced urticaria is due to physical or chemical identifiable factors.8,9
Despite the frequency of the disease, scarce information exists regarding CU and its frequency as well as the burden of the disease, and its consequences in Argentina.
In order to better understand the characteristics of CU patients in our geographical area – Buenos Aires, the largest populated area in Argentina – this study assess epidemiological, demographic, clinical, treatment and health care aspects of CU. The information supplied helps to understand how the disease behaves worldwide aiding the application of best common standards.
MethodsSettingThe population studied was the members of the Italian Hospital Medical Care Program (IHMCP), a prepaid health maintenance organization. IHMCP provides comprehensive medical and health services to 158,000 members approximately, primarily located in the urban areas around the Autonomous City of Buenos Aires, Argentina. Buenos Aires City is the capital city of Argentina and has a population of 2,965,403 inhabitants.10 Ninety-seven percent of the population is Caucasian and of European ancestry, and 3% belongs to other ethnicities. Argentina has a segmented health system consisting of three large sectors: Public, private, and social security (the last two covering a population of approximately 18.3 million people, distributed amongst nearly 300 entities of varying scope and size). Beneficiaries of the private system may freely choose their HMO. Approximately 5% of the population in these geographic areas is affiliated to the IHMCP.
Case definitionAll patients with diagnosis of CU (ICD-9-CM 708.1, 708.8, or 708.9) members of the IHMCP and with at least 12 months of follow up were included in the study.
Patient identification as clinical case in the Health SystemMultiple methods were used to find the patients suffering from CU to ensure complete ascertainment: a) patients included in allergist databases; b) patients with an ICPC (International Classification of Primary Care) code in the IHMCP computer-based patient record system; and c) patients with an ICD 9 (International Classification of Diseases) codification on admission to Hospital. Each potentially eligible subject underwent a standard procedure to confirm the diagnosis by urticaria experts who determined if patients fulfilled CU diagnosis.
Data collectionData regarding demographic characteristics (gender, age at onset, and age at diagnosis) were obtained from medical records for each patient. Drug prescriptions and the number of consultations with primary care or specialist during the 12 months previous to the inclusion in the study were evaluated.
Information about spontaneous or induced CU as well as its associated comorbidities as other autoimmune or allergic disorders was registered. Special care of the treatment habits was taken.
Statistical analysisAnalysis was performed using STATA version 10.1 (Stata Corporation, TX, USA).11 All medical records obtained from January 1, 2012 to December 31, 2014 were analyzed to calculate the prevalence ratio for CU per 100,000 populations with 95% CI. The day selected for prevalence calculation was December 31, 2014 and the denominator was the number of total affiliates of IHMCP. Prevalence ratio was calculated for the entire population and then discriminated for adult and pediatric members (less than 18 years old at diagnosis). The prevalence ratio for spontaneous and induced chronic urticaria and between gender was also analyzed per 100,000 populations with 95% CI. Baseline characteristics of the patients evaluated were reported as percentages for categorical data and mean with its standard deviation (SD) for continuous data.
This study was approved by the Ethics Committee prior to the initiation of the study.
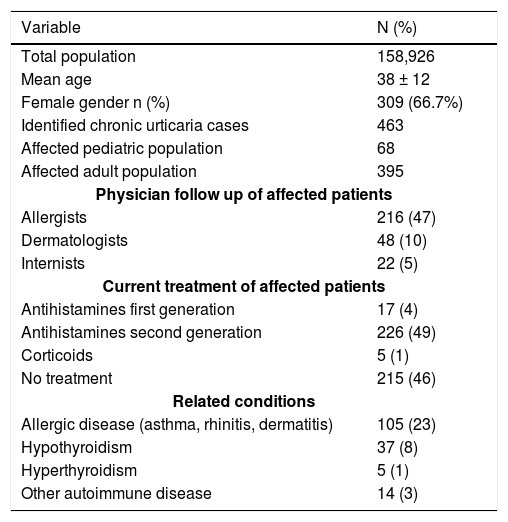
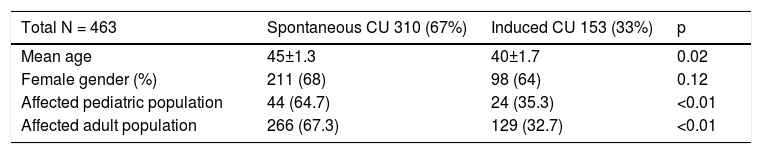
ResultsDuring the study period, 158,926 members were reviewed and included in the analysis. A total of 463 cases of CU were identified (68 pediatric, 395 adult) with a mean age of 38 ±12 years (mean age 13± 4 years for pediatrics and 42± 10 years for adults) (Table 1). A 47% of patients had allergists as their usual source of care, 10% had dermatologists and 58% internists. Almost 50% of the patients analyzed were under specific treatment for their chronic condition. Baseline characteristics are displayed in table 1. We stratified the affected patients in those with spontaneous and induced CU. An increase in the frequency of spontaneous CU was observed in pediatric as well as in adult patients compared with induced urticaria (Table 2). On December 31, 2014, the prevalence rate observed was 0.29 % (CI 95% 0.26-0.31%). When we split the population into pediatric (less than 18 years) and adult populations, the prevalence of CU in the adult population observed was 0.34% (95% CI 0.31-0.38%) while in pediatrics it was 0.15% (95% CI 0.11-0.20%) (Table 3). The prevalence of spontaneous and induced chronic urticaria is shown in table 3. We observed a higher frequency of CU in women compared with men in adult population (0.45%, CI95% 0.40-0.51 vs. 0.24%, CI95% 0.18-0.26 respectively, proportion 2/1) (Table 3). A total of 8% of patients had hypothyroidism and 23% had an allergic disease (asthma, rhinitis or dermatitis) as a related condition. We also observed that allergists follow CU patients in 47% of cases, dermatologists follow in 10% of cases and the main treatment used was second generation antihistamines, being the first line treatment recommended by current guidelines.9
Demographics at baseline of the population included
| Variable | N (%) |
|---|---|
| Total population | 158,926 |
| Mean age | 38 ± 12 |
| Female gender n (%) | 309 (66.7%) |
| Identified chronic urticaria cases | 463 |
| Affected pediatric population | 68 |
| Affected adult population | 395 |
| Physician follow up of affected patients | |
| Allergists | 216 (47) |
| Dermatologists | 48 (10) |
| Internists | 22 (5) |
| Current treatment of affected patients | |
| Antihistamines first generation | 17 (4) |
| Antihistamines second generation | 226 (49) |
| Corticoids | 5 (1) |
| No treatment | 215 (46) |
| Related conditions | |
| Allergic disease (asthma, rhinitis, dermatitis) | 105 (23) |
| Hypothyroidism | 37 (8) |
| Hyperthyroidism | 5 (1) |
| Other autoimmune disease | 14 (3) |
Spontaneous and induced chronic urticaria patient’s analysis
| Total N = 463 | Spontaneous CU 310 (67%) | Induced CU 153 (33%) | p |
|---|---|---|---|
| Mean age | 45±1.3 | 40±1.7 | 0.02 |
| Female gender (%) | 211 (68) | 98 (64) | 0.12 |
| Affected pediatric population | 44 (64.7) | 24 (35.3) | <0.01 |
| Affected adult population | 266 (67.3) | 129 (32.7) | <0.01 |
CU= chronic urticaria
Estimated prevalence of chronic urticaria in the members of the health maintenance organization stratified by gender, age and spontaneous or induced condition
| Members | N Cases | Prevalence ratio | 95%CI |
|---|---|---|---|
| Entire IHMCP prevalence ratio | |||
| 158,926 | 463 | 0.29 | 0.26-0.31 |
| Entire prevalence ratio in males | |||
| 74,755 | 154 | 0.20 | 0.17-0.24 |
| Entire prevalence ratio in females | |||
| 84,171 | 309 | 0.36 | 0.32-0.41 |
| Adult CU prevalence ratio | |||
| 114,168 | 395 | 0.34 | 0.31-0.38 |
| Adult CU prevalence ratio in males | |||
| 54,864 | 123 | 0.24 | 0.18-0.26 |
| Adult CU prevalence ratio in females | |||
| 59,304 | 272 | 0.45 | 0.40-0.51 |
| Pediatric CU prevalence ratio | |||
| 44,758 | 68 | 0.15 | 0.11-0.20 |
| Pediatric CU prevalence ratio in males | |||
| 19,891 | 31 | 0.15 | 0.10-0.22 |
| Pediatric CU prevalence ratio in females | |||
| 24,867 | 37 | 0.14 | 0.11-0.20 |
| Members | N Cases | Prevalence ratio | 95%CI |
| Adult cases of spontaneous CU | |||
| 114,168 | 266 | 0.23 | 0.20-0.26 |
| Pediatric cases of spontaneous CU | |||
| 44,758 | 44 | 0.1 | 0.07-0.13 |
| Adult cases of induced CU | |||
| 114,168 | 129 | 0.11 | 0.1-0.13 |
| Pediatric cases of induced CU | |||
| 44,758 | 24 | 0.05 | 0.03-0.07 |
CU= chronic urticaria
Global knowledge of CU epidemiology and characteristics is an unmet need. This work shows new data because is the first study performed in Argentina and in the region to evaluate the prevalence of CU as well as other epidemiological aspects. Despite the fact that the disease is not life-threatening, several studies over the last decade have shown that it has a significant impact on quality of life (QoL) and resource consumption in affected patients.5,12,13 Therefore, epidemiologic studies provide information concerning the burden of a society’s particular disease, which may contribute to improve public health planning.
In this study, we report a prevalence ratio of 0.29% in the entire population evaluated. Our findings are in line with previous studies. Hellgren et al. found a point prevalence of around 0.1% in the total population of Sweden.14 More recently Gaig et al. reported a prevalence of CU in Spain of 0.6% in a population-based study in adults with a significantly higher frequency of the disease in women than in men (OR=3.82, 95% CI 1.56-9.37) and with an average age of onset of 40 years in affected patients similar to our study.8 Zuberbier et al. found in a cross-sectional study performed in a general population by a questionnaire survey to 13,300 inhabitants of Berlin, Germany, a lifetime prevalence for CU of 1.8% (95% CI 1.4-2.3%), and prevalence for the 12 months before assessment of 0.8% (95% CI 0.6-1.1%), in which 70.3% of cases found were female.4 Possible explanations for this data variability can be due to differences in methods employed, geographic zone, genetics, and cultural characteristics.
Our results showed a higher prevalence of adult CU compared with data from Hellgren et al. (0.35%), but lower when compared with Gaig and Zuberbier (0.6% and 0.8%, respectively).4,8 Scarce information is available for pediatric population. Bruske et al. in a recent study described a cumulative prevalence of CU in the pediatric population (less than 10 years old) of 14.5% for males and 16.2% for females.3 Nevertheless, we observed that pediatric prevalence of CU was 0.15% for all CU cases. Some methodological differences that exist between studies could explain such observation (mainly hospital based studies and time of follow up), so direct comparisons are difficult to perform.
In our study, we also observed a higher frequency of CU in females than in males in the entire population and also in adult cases (Table 3). The previous is in line with other studies that showed a female/male ratio of almost 2/1 for CU the difference being more important mainly in the adult population, compared with the pediatric.3
Regarding related conditions, because many autoimmune diseases overlap, it was suggested that CU might be related to other autoimmune diseases. Thyroid disease is the most frequently investigated disease in CU.15 The mechanism of this association is currently unknown. We observed that 8% of patients had hypothyroidism. Allergic diseases (asthma, rhinitis or dermatitis) are also described as related conditions. Zuberbier et al. reported a higher frequency of allergic diseases compared to our population (53% vs. 23% in our study).4
We also observed that allergists follow CU patients in 47% of cases, dermatologists follow in 10% of cases and more than a half of included patients were followed by specialists probably due to the specific management that patients should have in order to control the disease.16
The main treatment used was second generation antihistamines, being the first line treatment recommended by current guidelines. First generation antihistamines have demonstrated major side effects, such as sedation and anticholinergic effects and should not be currently used in the treatment of urticaria.17 We did not observe significant differences regarding the treatment of CU (spontaneous and induced) in the adult and pediatric population, however, almost in 50% of the included patients, the information of treatment received was not available.
Undoubtedly, a weakness of the study is its retrospective design. Another weakness is that the results were obtained from an HMO and therefore contain a selection bias. Consequently, caution should be exercised if data are to be extrapolated.
ConclusionIn conclusion we observed that CU affects a significant number of patients in our population and despite the prevalence being slightly lower compared with studies from other regions, the clinical presentation and demographic characteristics do not seem to be different to previous data.
We considered that the present study emphasizes the burden of CU in an important populated region, Buenos Aires (Argentina), where no information about demographic, clinical and management characteristics of CU has been previously reported. The data shown in this study are good baseline information, showing how CU is presented in a developing country, therefore offering the opportunity to improve its management. The paper answers to an unmet global need. Increasing the global knowledge will help define common standards for CU management.
Financial support: None.
Conflict of interest: None