Primary cutaneous CD4+ small/medium T-cell lymphoproliferative disorder is a rare disease, with an indolent evolution and benign course. The classic presentation is a solitary nodule on the face or trunk. The disorder’s rarity and clinical and histopathological characteristics, can make the diagnosis difficult. We present the case of a 36-year-old Caucasian woman with a purplish erythematous nodule, hardened, shiny, asymptomatic, on the left nasal ala, which had grown progressively for 45 days. Histopathological examination and immunohistochemistry panel demonstrated alterations consistent with primary cutaneous CD4+ small/medium T-cell lymphoproliferative disorder. There was complete remission of the condition within 60 days of treatment with potent occlusive corticosteroids.
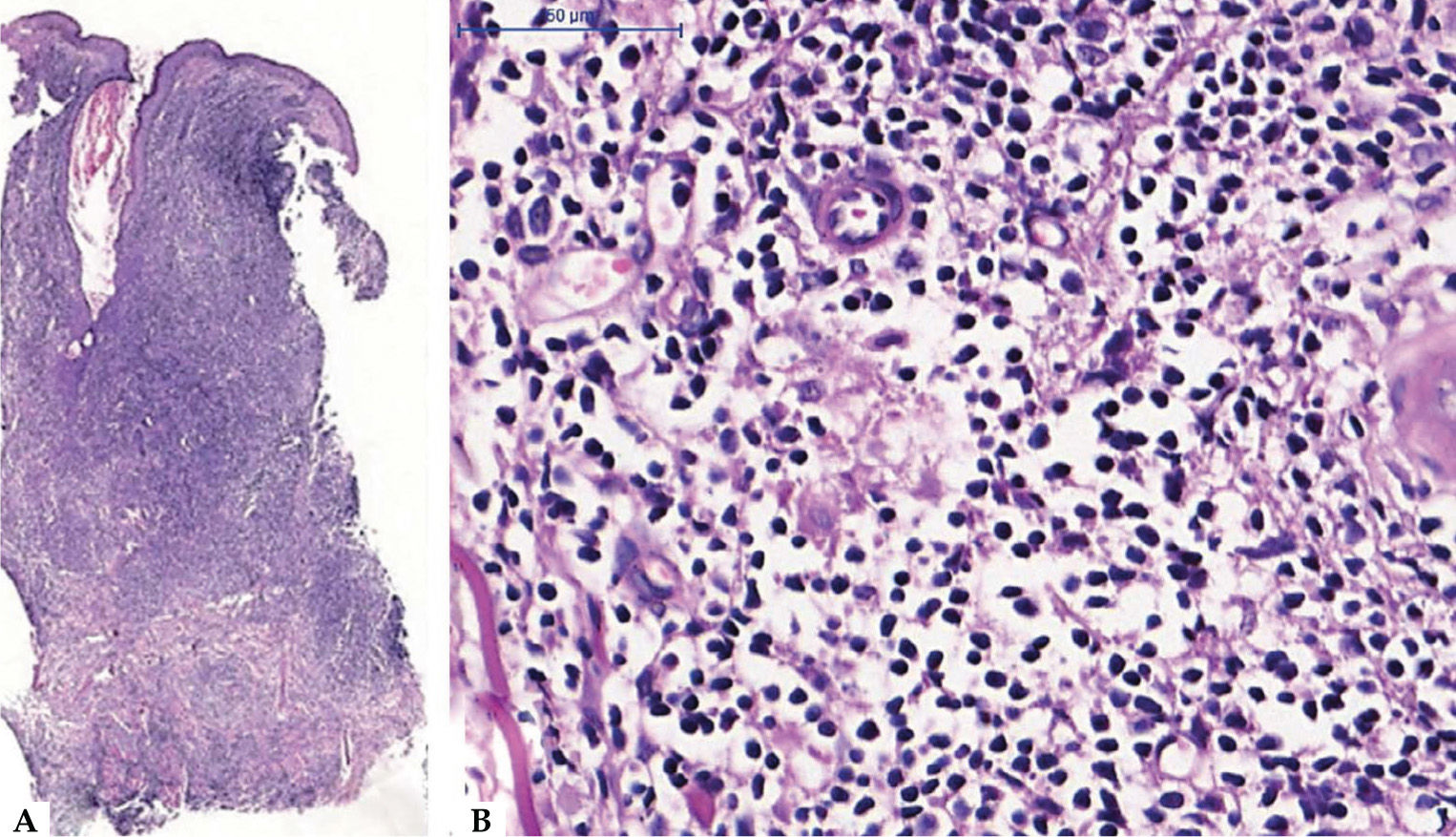
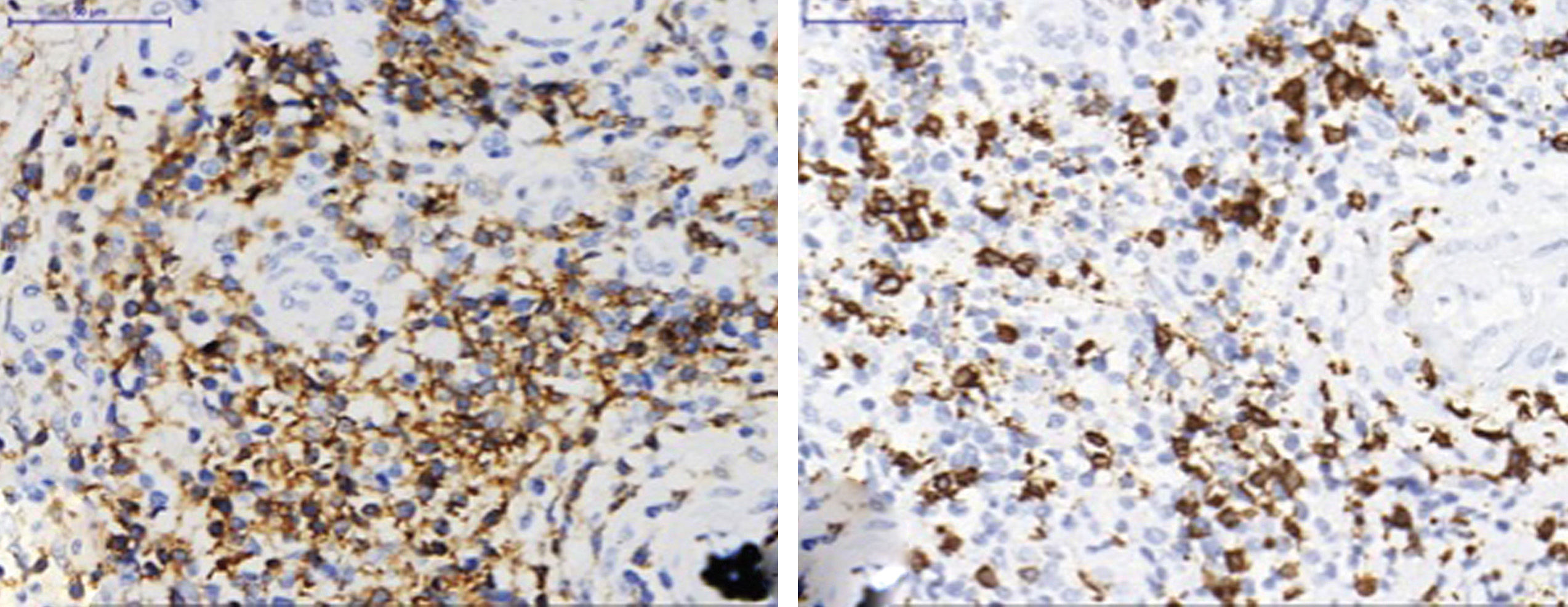
The patient was a 36-year-old female, Caucasian, schoolteacher, who reported a single purplish erythematous nodule with a firm consistency and shiny surface, with telangiectasias, clear contour, non-pruritic, located on the left nasal ala, approximately 1.5 cm in diameter, which had grown progressively for 45 days (Figure 1). No lymphadenopathy, visceromegaly, or other associated signs were identified. Histopathological examination showed atypical and diffuse lymphocytic infiltrate in the dermis, reaching the subcutaneous layer and involving the perivascular tissue. Lymphocytes were small to intermediate in size (Figure 2). Immunohistochemistry revealed a predominance of CD3+ T lymphocytes, with CD4+ immunopositivity (Figure 3). The cell proliferation index (Ki-67) was estimated at 10-15%, and there were rare CD30+ cells. Populations of plasma cells, histiocytes, and CD8+ T lymphocytes were observed in the background. Further tests such as CT scan, biochemical tests, blood count, lactate dehydrogenase, and β2-microglobulin levels were normal.
A - Histological skin section of dense lymphocytic infiltrate in the dermis (Hematoxylin & eosin, x50)
B - Histological skin section demonstrating the nuclear pattern of the lymphocytes in the lesion: small to medium-sized nuclei, predominantly regular karyotheca, hyperchromasia and perivascular and periadnexal arrangement, with no foci of epidermotropism (Hematoxylin & eosin, x400)
Primary cutaneous CD4+ small/medium T-cell lymphoproliferative disorder, previously called CD4+ small/medium pleomorphic T cell lymphoma, is a rare disease with indolent and insidious evolution, classically presenting as a solitary nodule on the face, neck, or trunk.1 Cases have been described in patients with some degree of immune compromise such as transplanted patients and those in use of immunobiologicals.2,3
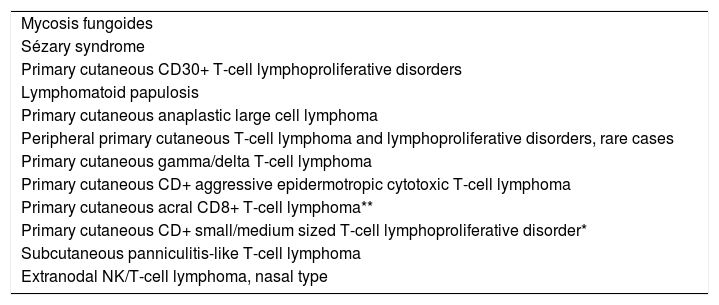
Despite the benign and favorable course of this disease, both the diagnosis and therapeutic approach remain challenging for dermatologists and pathologists.4 In 2017, the World Health Organization reviewed the classification of lymphomas and reclassified this primary cutaneous lymphoma (2005) as a lymphoproliferative disease (2017) (Chart 1).5,6
Classification of primary cutaneous T and NK cell lymphoproliferative disorders
| Mycosis fungoides |
| Sézary syndrome |
| Primary cutaneous CD30+ T-cell lymphoproliferative disorders |
| Lymphomatoid papulosis |
| Primary cutaneous anaplastic large cell lymphoma |
| Peripheral primary cutaneous T-cell lymphoma and lymphoproliferative disorders, rare cases |
| Primary cutaneous gamma/delta T-cell lymphoma |
| Primary cutaneous CD+ aggressive epidermotropic cytotoxic T-cell lymphoma |
| Primary cutaneous acral CD8+ T-cell lymphoma** |
| Primary cutaneous CD+ small/medium sized T-cell lymphoproliferative disorder* |
| Subcutaneous panniculitis-like T-cell lymphoma |
| Extranodal NK/T-cell lymphoma, nasal type |
Source: Swerdlow SH, et al, 2017.5
The distinction between cutaneous T-cell lymphoproliferative disorder and its differential diagnoses is extremely important, modifying the prognosis and treatment approach, particularly in relation to primary cutaneous CD8+ epidermotropic cytotoxic T-cell lymphoma, which has an aggressive clinical course and presents with morphological necrosis and ulceration. Other differential diagnoses include: mycosis fungoides and subtypes, which can be distinguished from each other based on clinical history and rapid evolution; primary cutaneous acral CD8+ T-cell lymphoma, which may overlap in its topography and clinical presentation but with a different immunophenotype and better prognosis; and primary cutaneous gamma/delta T-cell lymphoma, with highly aggressive clinical and morphological features.1,4,7
Markers of poor evolution and worse prognosis in cutaneous T-cell lymphoproliferative disorders include: disseminated lesions, rapid growth, and presence of more than 30% of large pleomorphic CD30+ T lymphocytes and/or high rates of cell proliferation, similar to that observed in high-grade lymphomas.1,7
The medical literature includes case reports showing efficient treatments, such as oral doxycycline, corticosteroids (topical, intralesional, and/or oral), surgical excision, and radiotherapy. However, there is no consensus on the best therapeutic approach for these cases.1,5, 7-10
The proposed treatment for this patient was occlusive fluocinolone (in patches), leading to the complete remission of the lesion within 60 days and no relapse in 90 days of follow-up. Potent corticosteroids have a lympholytic effect, promoting rapid involution of the infiltrate in localized forms, with low cost and high tolerability.
Financial support: None
Conflict of interest: None