Background: Body dysmorphic disorder is a relatively common psychiatric disorder in the context of dermatology and cosmetic and plastic surgery but is underdiagnosed and underreported in Africa.
Objectives: To evaluate the prevalence of body dysmorphic disorder and symptoms of anxiety/depression and determine their sociodemographic and clinical correlates.
Methods: A systematic random sampling design was made to recruit 114 patients with skin diseases. Sociodemographic and clinical data were obtained. The Body Dysmorphic Disorder Modification of the Yale-Brown Obsessive-Compulsive Scale, Hospital Anxiety and Depression Scale was administered, and data were analyzed using SPSS 20.
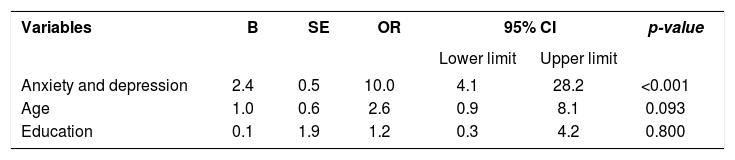
Results: Mean age of participants was 37.70±17.47 years, and 67/114 (58.8%) were females. Prevalence of body dysmorphic disorder was 41/114 (36.0%), and prevalence of anxiety/depression symptoms was 35/114 (30.7%). Prevalence of body dysmorphic disorder in patients with anxiety/depression symptoms was 15/41 (36.6%), and patients with facial disorders expressed the highest burden of anxiety/depression symptoms, in 15/35 (42.9%). Factors associated with significantly higher mean body dysmorphic disorder include age<50years (p=0.039), and anxiety/depression (p<0.001), education below high school was associated with higher mean anxiety/depression score (P= 0.031). In a binary logistic regression model, presence of anxiety/depression symptoms was predictive of body dysmorphic disorder (OR=10.0, CI: 4.1-28.2, p<0.001).
Study limitations: the study is uncontrolled, conducted in a single source of care, thus limiting generalization to nonrelated settings.
Conclusion: Prevalence of body dysmorphic disorder is high among dermatology patients and most prevalent in facial disorders. Facial diseases are associated with the highest burden of anxiety/depression symptoms. This is a clarion call for dermatologists to routinely assess for body dysmorphic disorder and appropriately refer affected patients to mental health care.
Body dysmorphic disorder (BDD) is a seriously impairing psychiatric condition characterized by excessive preoccupation with a perceived defect in one’s appearance or overemphasis on a slight defect.1,2 The fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) classifies body dysmorphic disorder under the obsessive and compulsive spectrum (OCP) disorders, due to its similarity to obsessive-compulsive disorder (OCD).3 Preoccupation per se does not connote the presence of a psychiatric disorder; however, when preoccupation is pathological, an underlying psychiatric condition may be present.4 Individuals with BDD are less likely to present to the psychiatrist first, but to dermatologists, plastic surgeons, or dentists, who all have less training to recognize and manage the disorder.4
Although individuals with BDD can be preoccupied with the appearance of any part of the body, concern with the skin, hair, and nose is the most common.5,6 In the skin, the main area of preoccupation is usually the face, despite some reported focus of concern on other areas like the neckline, arms, legs, or back. Common skin conditions that could lead to such preoccupation include acne, skin color, skin marks, wrinkles, or scarring.5,6 Patients’ concern with hair is mostly about balding or excessive body hair.5 Cororve & Gleaves found that women were more likely to be preoccupied with the breasts, hips, legs, and body weight, while men were more concerned about the genitals, excessive body hair, or balding.7 A recent study that screened for BDD among patients attending a tertiary institution found that facial flaws were the most common concern, in 62.5% of participants, followed by body asymmetry in 25%.8 It is common for individuals with BDD to spend an inordinate amount of time on rituals such as mirror checking or avoiding reflective surfaces, often attempting to hide the perceived deformity with makeup or clothing.1,9,10 Aside from the distress caused by the imagined body defects, the amount of time spent on rituals to hide them interferes with patients’ ability to function occupationally or socially, and negatively impacts their quality of life.11,12
Body dysmorphophobia is a common disorder, with a prevalence of 0.7% to 2.4% among community samples.1,13 Recent studies confirmed a high prevalence of BDD in dermatology and cosmetic surgery settings with a prevalence ranging from 4.52% to 35.16% and female preponderance.1,2,13,14 BDD has a high rate of psychiatric comorbidity, and extant literature has shown comorbidity with obsessive-compulsive disorder, major depressive disorder, social phobia, anxiety, and suicide.3,7,10,11 However, because patients’ presentation is usually first to a non-mental health professional, diagnosis may be delayed for several years after onset of the illness.4
In Nigeria and Africa as a whole, as elsewhere in world, the published literature on BDD is still scanty, and the disorder has remained underdiagnosed and underreported.12 Rapid changes in contemporary societies place a higher premium on appearance, and with the recent emergence and availability of ubiquitous social media, studies on feelings towards appearance become a subject of importance.1 Therefore, this study is planned to evaluate the prevalence of body dysmorphic disorder and symptoms of anxiety/ depression and to determine the sociodemographic and clinical correlates in patients attending the dermatology clinic in a new university teaching hospital in the Southwest of Nigeria.
MethodsThis cross-sectional study was conducted at the Dermatology Unit of the Department of Internal Medicine of the Ladoke Akintola University of Technology (LAUTECH) Teaching Hospital, Ogbomoso, Nigeria. The LAUTECH Teaching Hospital, Ogbomoso, was upgraded from the old General Hospital (a secondary hospital), built in the 1960s. The Teaching Hospital was established to meet the immediate health needs of the people of Oyo North Senatorial district including Ogbomoso land, Oyo, and Oke-Ogun area. The hospital also receives patients from part of Kwara State and the Osun State of Nigeria. The Dermatology Unit and its clinics were established in 2011 and were recently certified for postgraduate training in Dermatology. The Clinic is being run to date by two board-certified dermatologists with more than five years of experience in clinical diagnosis.
A cross-sectional design was made for systematic random sampling of participants. All willing alternate Dermatology Outpatient Clinic patients that met the inclusion criteria and signed the informed consent form were included. We included 114 participants with various skin disorders. Inclusion criteria were: consenting adults with dermatological diseases, age 18 years and above, and absence of preexisting/diagnosed psychiatric disorders or any other chronic or acute debilitating illnesses. The study excluded patients with dermatological disorders below the age of 18 years and those with any preexisting/diagnosed psychiatric disorder or debilitating acute/ chronic clinical or surgical illness. Two board-certified dermatologists evaluated and made the diagnosis of skin diseases. Most diagnoses were made clinically, and skin biopsies, scrapings, nail clippings, skin snips, and other tests were ordered to confirm or exclude differential diagnoses in some situations. The study was approved by the Research Ethics Board of the LAUTECH Teaching Hospital, Ogbomoso, with approval number LTH/OGB/EC/14/036.
Clinical assessment: sociodemographic parameters including age, education, marital status, and ethnicity were documented using a semi-structured questionnaire. History was obtained for rash, edema, ulcers, and pruritus, and duration of the symptoms and the diseases was documented in weeks. Participants were examined in daylight for diagnosis of their skin diseases. Anthropometric parameters including weight, height, and waist and hip circumference were documented using standard criteria prescribed by the National Health and Nutrition Examination Survey III. Body mass index (BMI) was calculated using the formula weight/(height2).15 Clinical diagnosis was noted, and the part of the body most significantly affected by the skin diseases was recorded.
Assessment of symptoms of body dysmorphic disorder.
Participants were evaluated for BDD using the English version of the Body Dysmorphic Disorder Modification of the Yale-Brown Obsessive-Compulsive Scale (BDD-YBOCS).16 The BDD-YBOCS is a semi-structured, clinician-rated, 12-item instrument designed to assess the severity of BDD symptoms. The first ten items on the instrument assess excessive preoccupation, obsession, and compulsive behaviors related to dissatisfaction with physical appearance, while items 11 and 12 assess insight and avoidance respectively. The 12 items are rated on a 0-4 scale, where 0 indicates no symptoms and 4 indicates extreme BDD symptoms. The total maximum score obtainable is 48 when all the rated items are summed together. BDD was dichotomized as present or absent, defined as present when the BDD total score is ≥12 and absent when the total score is less than 12. Permission to use the instrument was obtained from the senior author and copyright holder of the original version of the BDD-YBOCS.
Assessment of symptoms of anxiety and depressionSymptoms of coexisting anxiety and depression were assessed using the Hospital Anxiety and Depression Scale (HADS). HADS is a validated and reliable outcome measure developed for detection of the state of anxiety and depression within the medical outpatient setting. It is a 14-item instrument with the first seven questions designed to examine for anxiety and the last 7 for depression. Each of the items is scored 0-3 with 21 as the highest obtainable score and 0 as the lowest.17 Caseness, a score ≥ 8 for anxiety and depression, was determined based on a large systematic review by Bjelland et al., with sensitivity 0.78 and 0.79 and specificity 0.9 and 0.83 for anxiety and depression, respectively.18 The questionnaires were briefly pretested in a small population of patients before the commencement of the study.
Statistical analysisData were entered and analyzed using the Statistical Package for the Social Sciences (SPSS 18) version 18 (SPSS, Chicago, IL, USA). Frequencies of all the diagnosed skin diseases were estimated. All the categorical variables were analyzed using chi-square statistics, and continuous variables were analyzed using the Student t-test. The continuous skewed data were summarized using Mann-Whitney U statistics. All significant variables in the bivariate analysis were entered into a binary regression model as independent variables, and presence or absence of BDD was set as the dependent variable to determine the predictors of BDD. All the results of interest were represented in tables, and p-values < 0.05 were considered statistically significant.
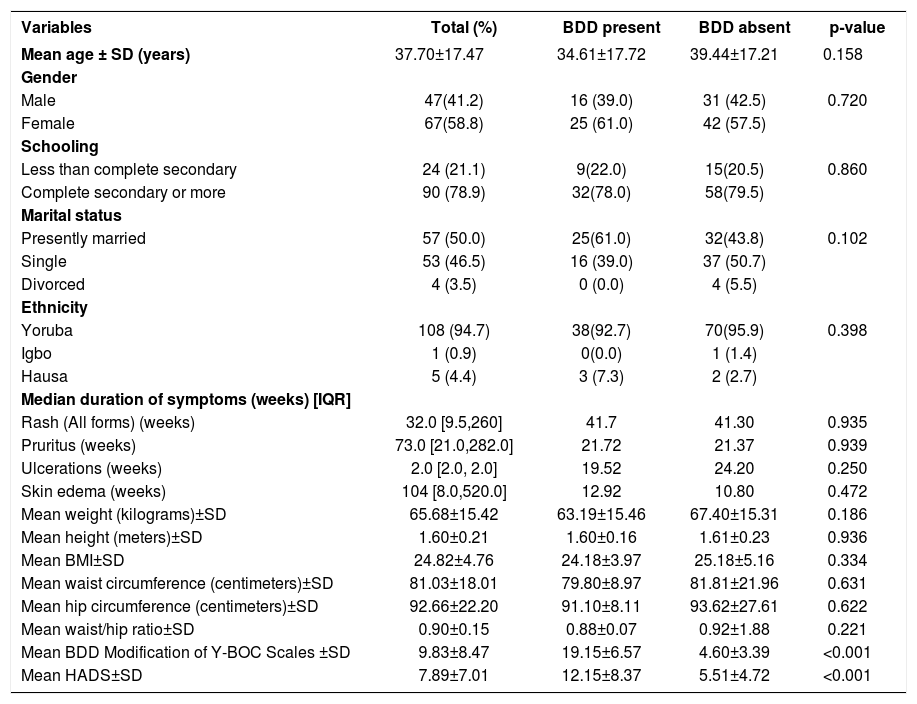
ResultsThe recruited participants were predominantly females, 67/114 (58.8%), with a mean age of 37.70±17.47 years. There was no significant difference in the mean age, educational attainment, marital status, ethnicity, or anthropometric parameters of the participants with or without BDD (Table 1).
Demographic and clinical characteristics of the study participants
| Variables | Total (%) | BDD present | BDD absent | p-value |
|---|---|---|---|---|
| Mean age ± SD (years) | 37.70±17.47 | 34.61±17.72 | 39.44±17.21 | 0.158 |
| Gender | ||||
| Male | 47(41.2) | 16 (39.0) | 31 (42.5) | 0.720 |
| Female | 67(58.8) | 25 (61.0) | 42 (57.5) | |
| Schooling | ||||
| Less than complete secondary | 24 (21.1) | 9(22.0) | 15(20.5) | 0.860 |
| Complete secondary or more | 90 (78.9) | 32(78.0) | 58(79.5) | |
| Marital status | ||||
| Presently married | 57 (50.0) | 25(61.0) | 32(43.8) | 0.102 |
| Single | 53 (46.5) | 16 (39.0) | 37 (50.7) | |
| Divorced | 4 (3.5) | 0 (0.0) | 4 (5.5) | |
| Ethnicity | ||||
| Yoruba | 108 (94.7) | 38(92.7) | 70(95.9) | 0.398 |
| Igbo | 1 (0.9) | 0(0.0) | 1 (1.4) | |
| Hausa | 5 (4.4) | 3 (7.3) | 2 (2.7) | |
| Median duration of symptoms (weeks) [IQR] | ||||
| Rash (All forms) (weeks) | 32.0 [9.5,260] | 41.7 | 41.30 | 0.935 |
| Pruritus (weeks) | 73.0 [21.0,282.0] | 21.72 | 21.37 | 0.939 |
| Ulcerations (weeks) | 2.0 [2.0, 2.0] | 19.52 | 24.20 | 0.250 |
| Skin edema (weeks) | 104 [8.0,520.0] | 12.92 | 10.80 | 0.472 |
| Mean weight (kilograms)±SD | 65.68±15.42 | 63.19±15.46 | 67.40±15.31 | 0.186 |
| Mean height (meters)±SD | 1.60±0.21 | 1.60±0.16 | 1.61±0.23 | 0.936 |
| Mean BMI±SD | 24.82±4.76 | 24.18±3.97 | 25.18±5.16 | 0.334 |
| Mean waist circumference (centimeters)±SD | 81.03±18.01 | 79.80±8.97 | 81.81±21.96 | 0.631 |
| Mean hip circumference (centimeters)±SD | 92.66±22.20 | 91.10±8.11 | 93.62±27.61 | 0.622 |
| Mean waist/hip ratio±SD | 0.90±0.15 | 0.88±0.07 | 0.92±1.88 | 0.221 |
| Mean BDD Modification of Y-BOC Scales ±SD | 9.83±8.47 | 19.15±6.57 | 4.60±3.39 | <0.001 |
| Mean HADS±SD | 7.89±7.01 | 12.15±8.37 | 5.51±4.72 | <0.001 |
BDD-body dysmorphic disorder, Y-BOC - the Yale-Brown Obsessive-Compulsive Scale, SD-standard deviation, %-percentage
Overall median duration of the presenting symptoms for all forms of skin rash was 32.0 weeks (IQR-9.5, 260), pruritus 73.0 weeks (IQR-21.0, 282), skin ulcerations 2.0 weeks (IQR 2, 2), and skin edema 104 weeks (IQR 8.0, 520). There was no significant difference in the mean rank of the duration of symptoms for participants with or without BDD. Participants with BDD had a significantly higher mean HADS score (12.15±8.37 vs. 5.51±4.72, p=0.001) compared to those without it (Table 1).
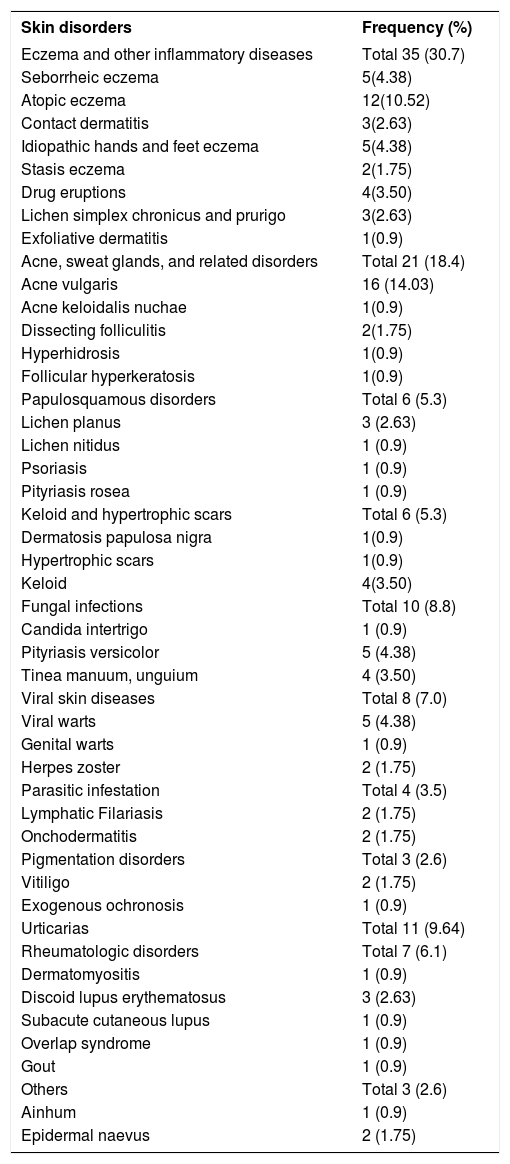
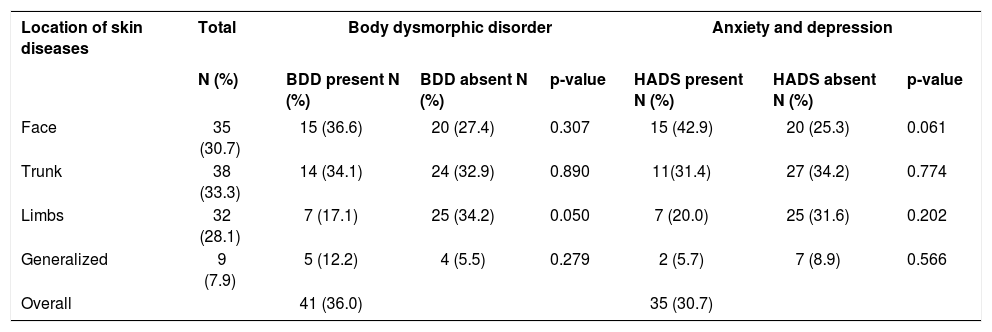
Table 2 shows the pattern of skin diseases seen in the study subjects. Eczema and related skin diseases 35(30.7%), acne and related conditions 21(18.4%), urticaria 11 (9.64%), fungal infections 10 (8.8%), viral skin infections 8 (7.0%), and rheumatological disorders 7(6.1%) were the six leading skin disorders. Affected sites included trunk 38 (33.3%), face 35 (30.7), limbs 32 (28.1), and generalized disorders 9 (7.9%) (Table 3).
Pattern of skin disorders among participants
| Skin disorders | Frequency (%) |
|---|---|
| Eczema and other inflammatory diseases | Total 35 (30.7) |
| Seborrheic eczema | 5(4.38) |
| Atopic eczema | 12(10.52) |
| Contact dermatitis | 3(2.63) |
| Idiopathic hands and feet eczema | 5(4.38) |
| Stasis eczema | 2(1.75) |
| Drug eruptions | 4(3.50) |
| Lichen simplex chronicus and prurigo | 3(2.63) |
| Exfoliative dermatitis | 1(0.9) |
| Acne, sweat glands, and related disorders | Total 21 (18.4) |
| Acne vulgaris | 16 (14.03) |
| Acne keloidalis nuchae | 1(0.9) |
| Dissecting folliculitis | 2(1.75) |
| Hyperhidrosis | 1(0.9) |
| Follicular hyperkeratosis | 1(0.9) |
| Papulosquamous disorders | Total 6 (5.3) |
| Lichen planus | 3 (2.63) |
| Lichen nitidus | 1 (0.9) |
| Psoriasis | 1 (0.9) |
| Pityriasis rosea | 1 (0.9) |
| Keloid and hypertrophic scars | Total 6 (5.3) |
| Dermatosis papulosa nigra | 1(0.9) |
| Hypertrophic scars | 1(0.9) |
| Keloid | 4(3.50) |
| Fungal infections | Total 10 (8.8) |
| Candida intertrigo | 1 (0.9) |
| Pityriasis versicolor | 5 (4.38) |
| Tinea manuum, unguium | 4 (3.50) |
| Viral skin diseases | Total 8 (7.0) |
| Viral warts | 5 (4.38) |
| Genital warts | 1 (0.9) |
| Herpes zoster | 2 (1.75) |
| Parasitic infestation | Total 4 (3.5) |
| Lymphatic Filariasis | 2 (1.75) |
| Onchodermatitis | 2 (1.75) |
| Pigmentation disorders | Total 3 (2.6) |
| Vitiligo | 2 (1.75) |
| Exogenous ochronosis | 1 (0.9) |
| Urticarias | Total 11 (9.64) |
| Rheumatologic disorders | Total 7 (6.1) |
| Dermatomyositis | 1 (0.9) |
| Discoid lupus erythematosus | 3 (2.63) |
| Subacute cutaneous lupus | 1 (0.9) |
| Overlap syndrome | 1 (0.9) |
| Gout | 1 (0.9) |
| Others | Total 3 (2.6) |
| Ainhum | 1 (0.9) |
| Epidermal naevus | 2 (1.75) |
Prevalence of body dysmorphic disorder and anxiety/depression symptoms among dermatology patients according to affected site
| Location of skin diseases | Total | Body dysmorphic disorder | Anxiety and depression | ||||
|---|---|---|---|---|---|---|---|
| N (%) | BDD present N (%) | BDD absent N (%) | p-value | HADS present N (%) | HADS absent N (%) | p-value | |
| Face | 35 (30.7) | 15 (36.6) | 20 (27.4) | 0.307 | 15 (42.9) | 20 (25.3) | 0.061 |
| Trunk | 38 (33.3) | 14 (34.1) | 24 (32.9) | 0.890 | 11(31.4) | 27 (34.2) | 0.774 |
| Limbs | 32 (28.1) | 7 (17.1) | 25 (34.2) | 0.050 | 7 (20.0) | 25 (31.6) | 0.202 |
| Generalized | 9 (7.9) | 5 (12.2) | 4 (5.5) | 0.279 | 2 (5.7) | 7 (8.9) | 0.566 |
| Overall | 41 (36.0) | 35 (30.7) | |||||
n=number; %-percentage; BDD- body dysmorphic disorder; HADS-Hospital Anxiety and Depression Scale
Overall prevalence of BDD symptoms was 41/114 (36.0%), with the highest prevalence in patients with facial skin disorders (36.6%). Other prevalence rates included conditions on the trunk, 14 (34.1%), and the limbs, 7 (17.1%), and generalized skin diseases, 5 (12.2%). A similar pattern was noted for anxiety/depression: 35 individuals presented symptoms of anxiety and depression, or a prevalence of 30.7%. Prevalence rates for anxiety and depression were highest in patients with facial disorders, 15 (42.9%), followed by the trunk, 11(31.4%), limbs, 7 (20.0%), and generalized skin diseases, 2 (5.7%) (Table 3).
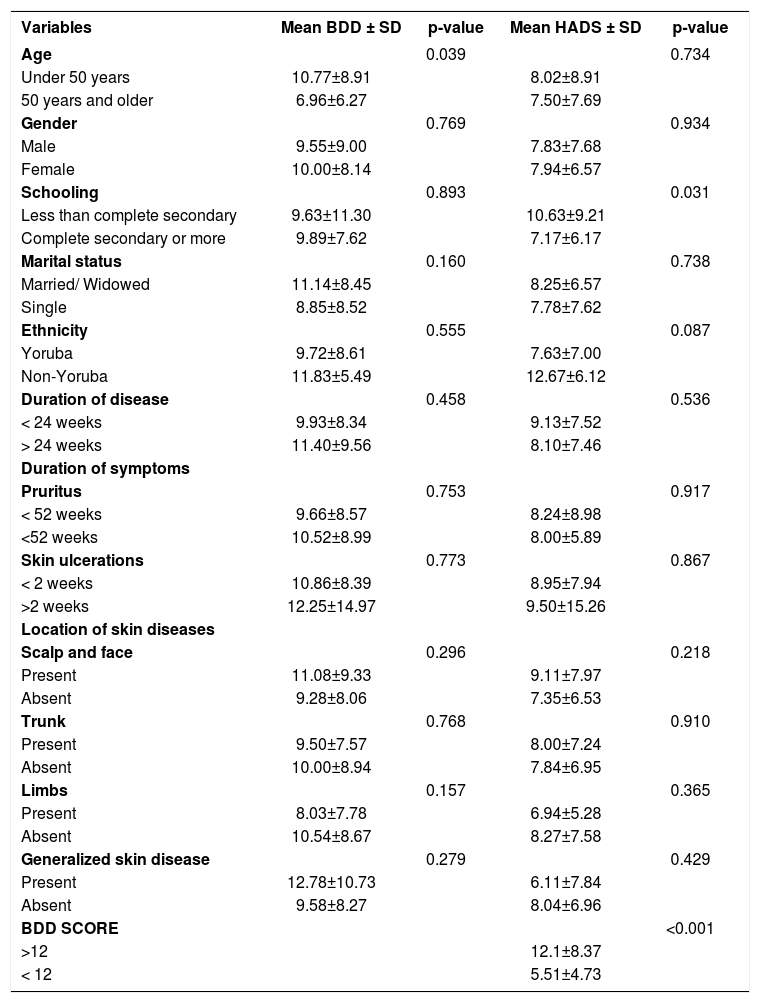
Table 4 shows the sociodemographic and clinical correlates of BDD and anxiety/depression. Participants below the age of 50 years were more likely to have higher mean BDD scores compared to those older than 50 years (10.77±8.91vs 6.96±6.27, p=0.039). Similarly, participants with less than a complete high school education had higher mean HADS scores (10.63±9.21vs7.17±6.17, p=0.031) compared to those with more schooling. The mean BDD score was significantly higher for patients with facial conditions (11.09±9.28, p=0.296) and generalized skin diseases (12.78±10.73, p=0.279), but lower for those with conditions affecting the trunk (9.50±7.50) and limbs (8.03±7.78). Participants with BDD had significantly higher anxiety/depression scores (12.10±8.37 vs. 5.51±4.73, p<0.001). There were no significant differences according to gender, marital status, or disease duration in the mean BDD and HADS scores. Participants with less than complete secondary education scored higher on HADS (p=0.031) compared to those with more schooling (Table 4).
Comparison of mean scores on body dysmorphic disorder scale and hospital anxiety and depression scale according to demographic and clinical variables
| Variables | Mean BDD ± SD | p-value | Mean HADS ± SD | p-value |
|---|---|---|---|---|
| Age | 0.039 | 0.734 | ||
| Under 50 years | 10.77±8.91 | 8.02±8.91 | ||
| 50 years and older | 6.96±6.27 | 7.50±7.69 | ||
| Gender | 0.769 | 0.934 | ||
| Male | 9.55±9.00 | 7.83±7.68 | ||
| Female | 10.00±8.14 | 7.94±6.57 | ||
| Schooling | 0.893 | 0.031 | ||
| Less than complete secondary | 9.63±11.30 | 10.63±9.21 | ||
| Complete secondary or more | 9.89±7.62 | 7.17±6.17 | ||
| Marital status | 0.160 | 0.738 | ||
| Married/ Widowed | 11.14±8.45 | 8.25±6.57 | ||
| Single | 8.85±8.52 | 7.78±7.62 | ||
| Ethnicity | 0.555 | 0.087 | ||
| Yoruba | 9.72±8.61 | 7.63±7.00 | ||
| Non-Yoruba | 11.83±5.49 | 12.67±6.12 | ||
| Duration of disease | 0.458 | 0.536 | ||
| < 24 weeks | 9.93±8.34 | 9.13±7.52 | ||
| > 24 weeks | 11.40±9.56 | 8.10±7.46 | ||
| Duration of symptoms | ||||
| Pruritus | 0.753 | 0.917 | ||
| < 52 weeks | 9.66±8.57 | 8.24±8.98 | ||
| <52 weeks | 10.52±8.99 | 8.00±5.89 | ||
| Skin ulcerations | 0.773 | 0.867 | ||
| < 2 weeks | 10.86±8.39 | 8.95±7.94 | ||
| >2 weeks | 12.25±14.97 | 9.50±15.26 | ||
| Location of skin diseases | ||||
| Scalp and face | 0.296 | 0.218 | ||
| Present | 11.08±9.33 | 9.11±7.97 | ||
| Absent | 9.28±8.06 | 7.35±6.53 | ||
| Trunk | 0.768 | 0.910 | ||
| Present | 9.50±7.57 | 8.00±7.24 | ||
| Absent | 10.00±8.94 | 7.84±6.95 | ||
| Limbs | 0.157 | 0.365 | ||
| Present | 8.03±7.78 | 6.94±5.28 | ||
| Absent | 10.54±8.67 | 8.27±7.58 | ||
| Generalized skin disease | 0.279 | 0.429 | ||
| Present | 12.78±10.73 | 6.11±7.84 | ||
| Absent | 9.58±8.27 | 8.04±6.96 | ||
| BDD SCORE | <0.001 | |||
| >12 | 12.1±8.37 | |||
| < 12 | 5.51±4.73 |
BDD- Body Dysmorphic Disorder;
HADS-Hospital Anxiety and Depression Scale
In a binary logistic regression model of all significant contributory variables, presence of symptoms of anxiety/depression was predictive of BDD. Participants with symptoms of anxiety and depression were ten times more likely to have BDD compared to those without such symptoms (OR=10.0, CI: 4.1-28.2, p<0.001) (Table 5).
DiscussionTo the best of our knowledge, this was the first study that examined BDD symptoms in dermatology patients in Nigeria. We found a prevalence of 36.0% in a general dermatology clinic in Ogbomoso. This prevalence was similar to but slightly higher than the upper limit of 4.52% to 35.16% documented in dermatology clinic-based studies as found in a recent systematic review.14 Expectedly, the prevalence in our sample was also higher than 0.7-2.4%, recorded in studies conducted in the general population.19,20 Previous studies have shown that BDD is more common in patients seeking plastic surgery interventions and those attending dermatology clinics than in the asymptomatic general population.14,19,20 Cumulative prevalence of BDD in dermatology patients in the present study (36.0%) was close to that reported by Bowe et al. (35.16%) and higher than the 8.81% described by Ozun et al. and 11.94% reported by Phillips et al.21-23, which included only participants with acne vulgaris. The factors that could affect the prevalence of BDD vary widely according to the assessment methods, study site, societal values, cultural norms, the survey’s setting, and the skin diseases targeted by the study.1,23
There were no differences in the current study according to gender, marital status, or body weight between participants with and without BDD, which is consistent with other studies1,6,24 Patients under 50 years of age had significantly higher mean BDD scores compared to older participants, also corroborating previous studies.24,25 Corando et al.1 also found no association between marital status or gender and BDD in their overall analysis, but found that cosmetic patients with BDD were more likely to be single women with low BMI. The higher mean BDD scores among younger individuals might be related to the fact that these people care about their appearance more than older individuals. Contrasting with our bindings, Brohede et al. in Sweden also found that BDD patients were more likely to be single, less educated, younger, and unemployed or on sick leave within a small age group.11
In the present study, conditions on the face were associated with the highest prevalence of BDD and anxiety and depression. These findings may be due to the fact that participants with facial conditions do not have their diseases disguised by clothing, with such consequences as social anxiety, shame, social avoidance or isolation, occupational dysfunction, unnecessary cosmetic surgery, and suicide, which are recognized as accompanying BDD.1,9,11,26 The high prevalence of anxiety and depression in association with facial disorders in this study confirms this assertion. The fact that the location of the conditions was not significantly associated with BDD shows that there are other inherent patient-related traits that determine who develops BDD. The duration of symptoms or diseases also appears to be irrelevant for BDD. Studies have indicated that genetic factors may be essential determinants in the development of BDD.27,28 Monzani et al. described a genetic overlap between BDD and OCD and found that genetic factors could explain 64% of phenotypic correlation between the two disorders.28 The study also demonstrated a 43% heritability concordance in monozygotic twins.28 An interplay between genetics and the presence of body blemishes in susceptible parts of the body, irrespective of size, severity, and duration of symptoms, might be responsible for the development of BDD. Genetic studies are therefore needed to identify the BDD-related gene among Africans.
Previous studies have shown that BDD patients are highly somatic and distressed by the high level of non-BDD symptoms and poor well-being in domains of depression, anxiety, somatic symptoms, and anger-hostility.9,11,29 Symptoms of anxiety and depression were highly prevalent (30.7%) in our cohort, and the presence of anxiety and depression predict the existence of BDD in a regression analysis. Similarly, a previous study also corroborated the coexistence of BDD with social phobia and obsessive-compulsive disorder.7 Philip et al.29 found depression as the psychiatric disorder most frequently associated with BDD. Perceived ugliness could present with depression and accompany suicidal ideation.30
The study’s limitations include the fact that it was not placebo-controlled and that it was cross-sectional and conducted in a single center, so the results may not be generalizable to unrelated settings. These limitations notwithstanding, the study’s strength lies in its careful selection of participants. It was also the first survey to examine the prevalence of BDD among patients attending a dermatology clinic in Nigeria and it thus produces data in an area yet to be adequately explored in our region. The study employed well-validated, reliable, and tested instruments to generate the data. The study also examined the prevalence of BDD and associations with common comorbidities, which could help provide the basis for collaborative care involving psychiatrists and psychologists.
ConclusionThe high prevalence of BDD in this study is a clarion call for dermatologists to reach beyond the clinical treatment of skin conditions and investigate symptoms of BDD by asking patients direct questions on how they feel about their appearance. Timely diagnosis and prompt referral to follow-up by mental health services aim to prevent future adverse consequences.
Study conducted at the Dermatology Unit, Department of Internal Medicine, Ladoke Akintola University of Technology Teaching Hospital, Ladoke Akintola University of Technology, Ogbomoso, Oyo State, Nigeria
Financial support: None.
Conflict of interest: None.