Dear Editor,
Immunocompromised patients with hematologic neoplasms are particularly prone to developing herpes-virus infections. Both the primary infection and the reactivation of the herpes simplex virus (HSV) should be seriously considered in these cases, as they correspond to one of the most frequent mucocutaneous infections, and they have the capacity to manifest in atypical forms and mimic a range of other pathologies.1
A 60-year-old female patient presented painful pruritic lesions on the face, which began three months prior to consultation. She denied experiencing fever or other symptoms but reported being diagnosed with chronic lymphocytic leukemia (CLL) 18 months prior. Two ulcerated, crusted, erythematous infiltrated plaques were observed: one on the right epicanthus, measuring 3 × 2cm; the other in the left malar region, measuring 4 × 2.5cm (Figure 1). The hemogram showed important leukocytosis (76,920), with 73,074 lymphocytes. Tomographic exams showed bilateral axillary, para-aortic, and intercostal lymphadenomegaly, hepatic and splenic hilar lymphadenomegaly, and splenomegaly.
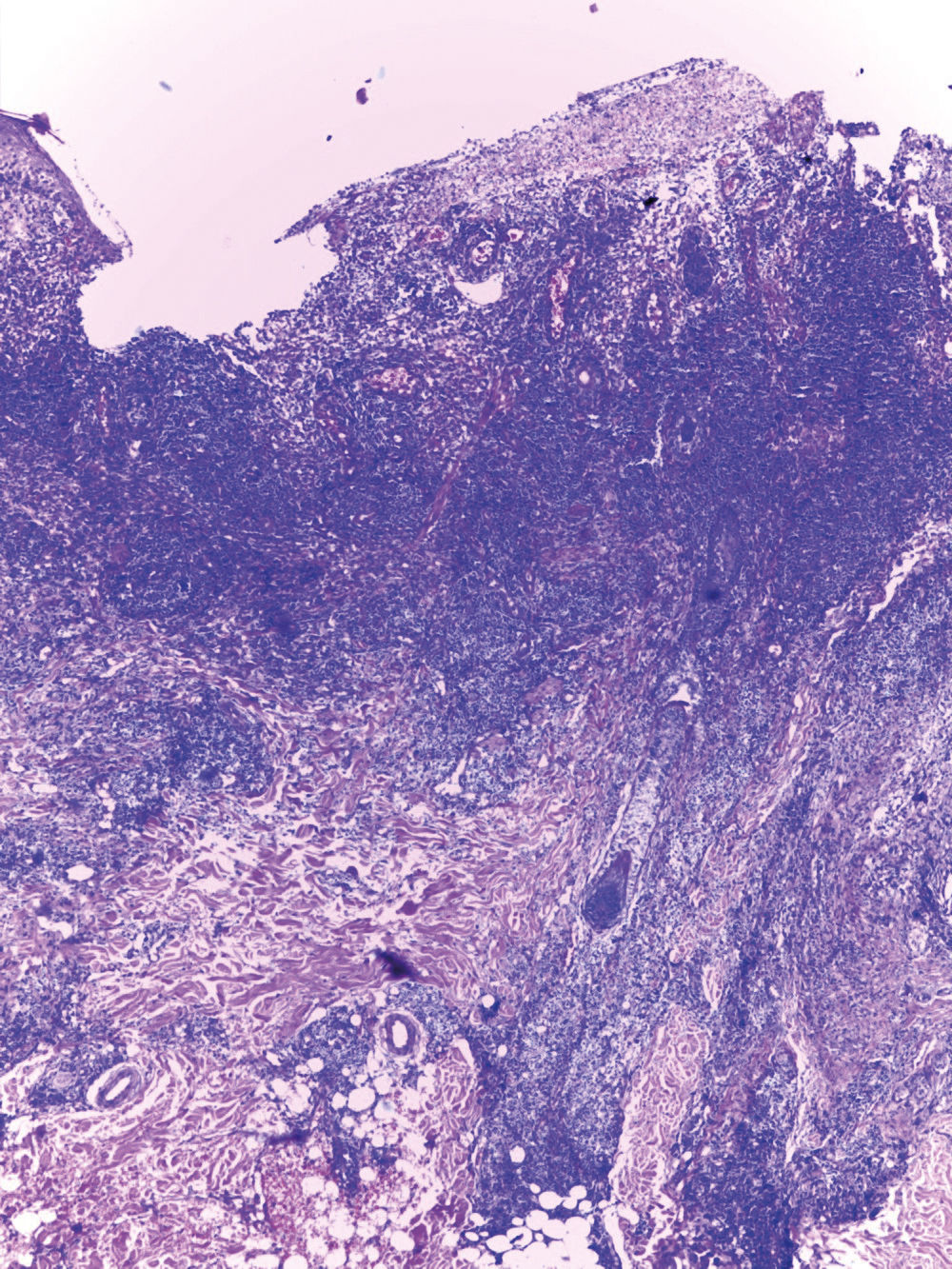
The biopsy of the cutaneous lesion in the malar region presented pathological epidermal changes of viral cytopathic effect, represented by focal necrosis and keratinocytes with karyomegaly, multinucleation, ground-glass chromatin and molded nuclei. The dermis showed a dense/diffuse nodular lymphocytic infiltrate, with lymphocytes presenting focal cytologic atypia, expressed by pleomorphism, hyperchromatism and grooved nuclei (Figure 2). Given the cytologic atypia and the patient’s underlying disease, the material was sent for immunohistochemical analysis, which revealed a predominant and mixed population of T and B cells, negativity for markers of lymphoproliferative neoplasms [CD10 (common acute lymphoblastic leukemia antigen; CALLA), deoxynucleotidyl transferase (TdT) and cyclin D1], and positivity for human herpes-viruses I and II. After oral administration of acyclovir (400mg, five times daily) for one week, the lesions were completely healed (Figure 3).
Ulcerated epidermis and remaining epithelium presenting pathological changes of viral cytopathic effect, represented by focal necrosis, keratinocytes with karyomegaly, multinucleation, ground-glass chromatin and molded nuclei. Dermis showed a dense/diffuse nodular lymphocytic infiltrate, with lymphocytes presenting pleomorphism, hyperchromatism, and grooved nuclei (Hematoxylin & eosin, x100)
Cutaneous herpes-virus infections typically present as vesicular eruption on an erythematous base. The diagnosis is made, in most cases, based on clinical history, dermatological examination and the Tzanck test.2 However, in immunocompromised patients, the clinical presentation is often atypical, which can lead to diagnostic delay. In those cases, a direct fluorescent antibody test, a viral culture, or a cutaneous biopsy with immunohistochemistry may be necessary to make a definitive diagnosis.3 The susceptibility of patients with CLL to herpes-virus infections results from factors related to the disease, such as deficiencies in immunoglobulin and in T-cell function.4 Moreover, the modalities used to treat CLL further increase the risk of infection.
The histopathological findings in biopsies of fully developed cutaneous herpes-virus infections consist of an intraepidermal vesicle with varying degrees of epithelial necrosis. Most of the characteristic changes are observed in the nuclei of keratinocytes and involve chromatin marginalization, ballooning and a ground-glass appearance. In the cytoplasm of these keratinocytes, the earliest change is the presence of vacuolization. The mechanism by which the intraepidermal vesicles form includes ballooning of the keratinocytes and reticular degeneration. Ballooning is a cytological characteristic of viral infections; the affected cells appear swollen and separated from the neighboring cells through loss of their intercellular bridges (secondary acantholysis). In the surrounding environment, the typical infiltrate is mixed, with lymphocytes, neutrophils, and multinucleated giant cells, though variable patterns of inflammation are described, including folliculitis, vasculitis, and lymphoid infiltrate with cytologic atypia.5
Wain et al. (2008) described two immunocompromised patients in which infection by HSV triggered an intense pseudolymphatic reaction, whose clinical aspects and histological differential diagnosis were of cutaneous lymphoma,4 just as in the case described in this article. Herpetic infections should, therefore, be included in the differential diagnosis of acute and chronic ulcers in a patient with leukemia or another immunocompromising condition.1 For these patients, even providing a good anamnesis and a good physical exam, the correct diagnosis and the introduction of appropriate therapy may not be achieved without support from histopathological and immunohistochemical exams.
Financial support: None.
Conflict of interest: None.