The authors present seven cases of rhinocerebral mucormycosis associated to diabetes mellitus, which is a disease with epidemic proportions affecting individuals worldwide, particularly in developing countries, and which poses significant morbidity and mortality. Mucormycosis is an opportunistic fungal infection with high mortality and requires an invasive therapeutic approach to save the patient’s life with significant morbidity and sequelae, thus prevention is crucial.
Diabetes mellitus (DM) is one of the leading morbimortality diseases worldwide, with over 425 million affected individuals, particularly in low/medium income countries. Risk factors include an unhealthy sedentary lifestyle, diet high in refined sugar and fat, and genetic susceptibility1.
It is associated to numerous complications and comorbidities such as neutrophil dysfunction and impaired humoral immunity that predispose to fungal infections2.
Rhinocerebral mucormycosis is an opportunistic fungal infection of non-septate hyaline hyphae which are ubiquitous saprophytes that are easily isolated from decomposing vegetation and high fructose fruits, soil, manure, and human orifices3.
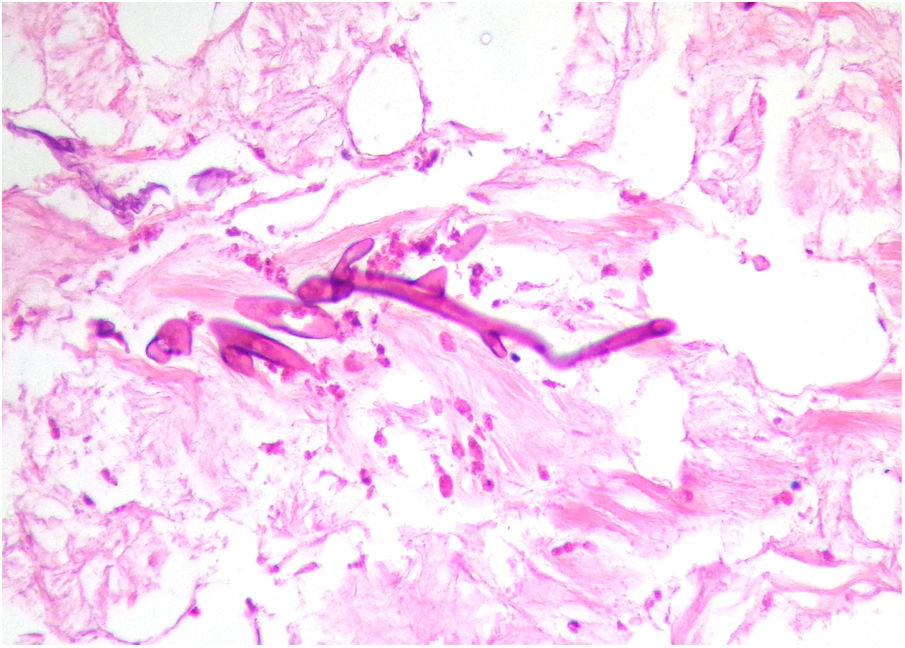
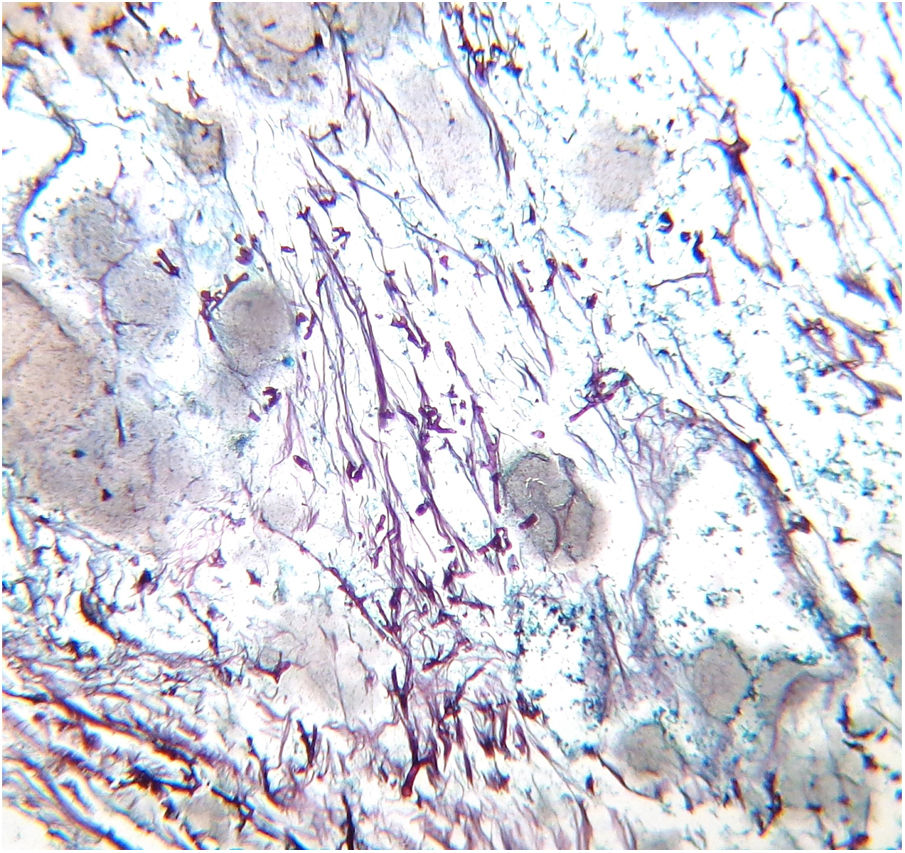
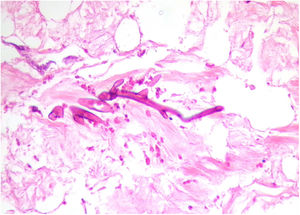
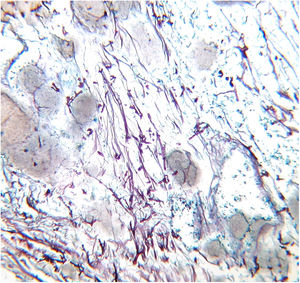
Despite adequate treatment, this infection has high mortality (40%–63%), and its prevalence has increased, probably due to the growing number and higher survival rates of immunosuppressed patients4,5. Most infections are life threatening, as the fungus has particular affinity for vascular walls that cause irreversible damage through thrombosis and ischemic necrosis. Figures 1 and 2 present biopsy specimens taken from patients for diagnosis, and the fungus can be seen invading the normal tissue.
The well identified predisposing factors are ketoacidosis by decompensated diabetes mellitus, advanced kidney failure, drug abuse, immunosuppressive treatment, or any other disease that causes neutropenia or polynuclear neutrophil deficit4–7.
Initially, most patients complain of symptoms similar to acute bacterial sinusitis, but rapid deterioration occurs with alterations in the visual acuity, facial edema, and necrotic areas, which are the hallmarks of the disease, either on the face or intraorally. Orbit involvement occurs in 66%–100% of the cases and any contiguous region may also be involved5.
Timely diagnosis is fundamental for a positive outcome, so treatment with amphotericin B should be initiated on clinical presumption. Also, aggressive surgical debridement is fundamental, as removing the necrotic areas will reduce the fungal burden and will also facilitate the antifungal’s action3,4. Amphotericin B improves survival rate up to 55%, adding to the results of surgical debridement. Another option is posaconazole and hyperbaric oxygen3,5,7.
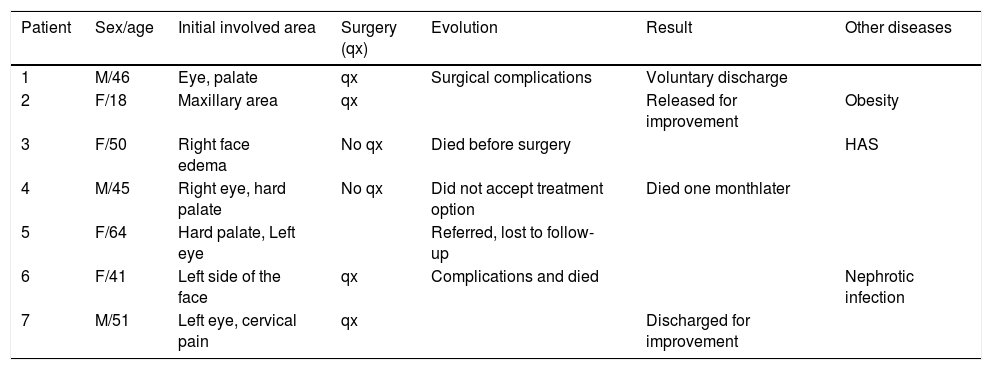
Cases reportThe authors present seven cases of diabetic patients that attended this tertiary care hospital with rhinocerebral mucormycosis (Table 1). They were three males and four females, with ages ranging from 18–64 years (Figures 3 and 4). One of them was referred to another hospital because of lack of space, another did not accept surgery, and another died before the surgery was performed. Of the four patients who underwent surgery, two died in the postsurgical period and the other two were discharged for improvement after several weeks. All of them received amphotericin B as part of the treatment, including those who did not undergo surgery.
Patient data and evolution.
| Patient | Sex/age | Initial involved area | Surgery (qx) | Evolution | Result | Other diseases |
|---|---|---|---|---|---|---|
| 1 | M/46 | Eye, palate | qx | Surgical complications | Voluntary discharge | |
| 2 | F/18 | Maxillary area | qx | Released for improvement | Obesity | |
| 3 | F/50 | Right face edema | No qx | Died before surgery | HAS | |
| 4 | M/45 | Right eye, hard palate | No qx | Did not accept treatment option | Died one monthlater | |
| 5 | F/64 | Hard palate, Left eye | Referred, lost to follow-up | |||
| 6 | F/41 | Left side of the face | qx | Complications and died | Nephrotic infection | |
| 7 | M/51 | Left eye, cervical pain | qx | Discharged for improvement |
All of the patients acquired the fungal infection prior to the hospitalization, except for one patient who was admitted to the hospital for a nephrotic infection that resulted in nephrectomy; after several days she developed mucormycosis symptoms.
Of the three patients who died, two of them had metabolic dyscontrol and all presented ketoacidosis at some point during the disease.
DiscussionThe diagnosis of mucormycosis requires clinical suspicion and quick action, as the fungal invasion of the vessels advances rapidly. Its diagnosis is considered an emergency. Ideally, it must include mycological diagnosis with a direct exam and a culture that grows in 24hours. Also, to determine the extent of the damage, imaging tests are of great help, such as tomography. Surgical debridement provides a chance to cure, and material for histopathological confirmation. The main differential diagnosis is invasive aspergillosis.
DM is a global burden with a rise in prevalence and incidence during the last decade, and besides being directly related to death, it is also very associated to serious morbidity and disability.
For example, in the Mexican population, since the year 2000, DM is the leading cause of death among women and the second in men, representing 15% of deaths. Up to 90% of the cases are related to obesity, and 72% of Mexican adults are obese8. Thus, the public health system must simultaneously address these two diseases as an epidemiological emergency. This scenario may also be observed in other countries, particularly those of Latin America that have similarities to Mexico, which must also be aware of this risk.
These seven cases were related to this metabolic disease, supporting that mucormycosis is an opportunistic fungal infection that affects critically ill patients of any age and with any kind of immunosuppression, particularly those living with diabetes.
These cases are an example of what may become a more and more frequent diagnosis in the near future if this obesity epidemic is not reverted or at least slowed down.
Financial supportNone declared.
Authors’ contributionsErick Martínez-Herrera: Data collection, analysis, and interpretation; effective participation in research orientation.
Angélica Julián-Castrejón: Effective participation in research orientation; intellectual participation in propaedeutic and/or therapeutic conduct of studied cases.
María Guadalupe Frías-De-León: Data collection, analysis, and interpretation; intellectual participation in propaedeutic and/or therapeutic conduct of studied cases.
Gabriela Moreno Coutiño: Approval of the final version of the manuscript; study conception and planning; critical review of the literature; critical review of the manuscript.
Conflicts of interestNone declared.
How to cite this article: Martínez-Herrera E, Julián-Castrejón A, Frías-De-León MG, Moreno-Coutiño G. Rhinocerebral mucormycosis to the rise? The impact of diabetes world epidemics. An Bras Dermatol. 2021;96:196–9.
Study conducted at the Hospital Regional de Alta Especialidad de Ixtapaluca, Ixtapaluca, México.