Basal cell carcinoma is the most common type of skin cancer. Although the literature provides a great deal of information on the recurrences of basal cell carcinoma, studies about these indices addressing only the cases in which flaps and/or grafts have been performed for surgical reconstruction of the excision of this tumor are still lacking.
ObjectivesTo evaluate rates of recurrence of basal cell carcinoma submitted to conventional surgery with pre-established margins and reconstruction by flaps or grafts.
MethodsA retrospective and observational study was performed through the analysis of 109 patients, who met inclusion criteria with 116 basal cell carcinomas submitted to conventional surgery and pre-established safety margins, requiring reconstruction through a graft or cutaneous flap. This work was performed the small surgeries sector of Dermatology of the Specialty Outpatient Clinic of the University Hospital of the State University of Londrina, between January 1, 2011 and December 31, 2015. The following data were collected and inserted in an Excel worksheet: name, registration number of the hospital patient, sex, age, tumor location, histopathological type of BCC, procedure performed (type of flap and/or graft), follow-up time, recurrence.
ResultsOf the 116 procedures, there were recurrences in 3 cases (2.6%) that were located in the nasal region and related to sclerodermiform or micronodular histological types.
Study limitationsRetrospective nature of the study.
ConclusionThe present study of the dermatology department of this university hospital showed a low rate of recurrence of basal cell carcinoma in cases where flaps and/or grafts were used in the surgical reconstruction.
Basal cell carcinoma (BCC) is the most common type of skin cancer.1-3 BCC relapses and recurrences are problems in patient follow-up, especially when a graft and flap is required to close the surgical wound.4 In the literature, recurrences of these tumors range from 4% to 16.6%, but do not separate between the cases with recurrence by primary closure from those requiring more complex reconstructions. 5-10
In view of the absence of micrographic surgery in our service, we performed a retrospective study of excisions of BCCs with preset margins (4-5mm) requiring graft and/or flap and evaluated cases of recurrences. Although the literature brings information about the recurrences already mentioned, studies are still lacking on these indexes when only using skin flaps and/or grafts.
MethodsThe study is retrospective and observational, through analysis of medical records, approved by the Research Ethics Committee (REC) of the State University of Londrina (UEL), certificate of presentation for ethical appreciation (CPEA): 57073416.9.0000. Data were collected from all patients with BCC and who needed a skin graft and/or flap who were treated at the small surgeries outpatient clinic of the Dermatology Service of the Regional University Hospital of the North of Paraná, State University of Londrina (PR), Brazil. in the period from January 1, 2011 to December 31, 2015. Follow-up ended on December 31, 2017.
In addition to previous and post-surgery photographs (which were stored in image banks, the collection and storage of images were previously authorized by patients when they underwent surgery on Tuesday afternoons), the following data were collected and inserted in Excel spreadsheet: name, hospital patient record number, sex, age, tumor location, histopathological type of BCC, procedure performed (skin flap and/or graft type), months of follow-up and recurrences.
Exclusion criteria: cases of excision of BCC with primary closure, cases with margins compromised by tumor, recurrences, collision tumor, basal cell nevus syndrome, xeroderma pigmentosum and patients who died before completing 12 months of follow-up.
Data were analyzed and processed by GraphPad Instat and Excel 2007. Statistical significance was assessed by the chi-square test, considering a significance level of 5% (p <0.05) and were applied to compare sex, age group and location of tumors addressed initially. Fischer’s Exact Test was used when we analyzed expected frequencies below five.
A convenience sample was used, i.e., all surgeries without exclusion criteria, with BCC and needing graft/flap in the afternoon service were monitored during the period in question.
ResultsIn the period from January 2011 to December 2015, 109 patients and 117 BCC procedures were recorded in which there was need for flaps or grafts in the small surgeries sector on Tuesday afternoons of the Hospital of Clinics Outpatient Department (AHC) of the Service of Dermatology of the Regional University Hospital of the North of Paraná of the State University of Londrina (PR).
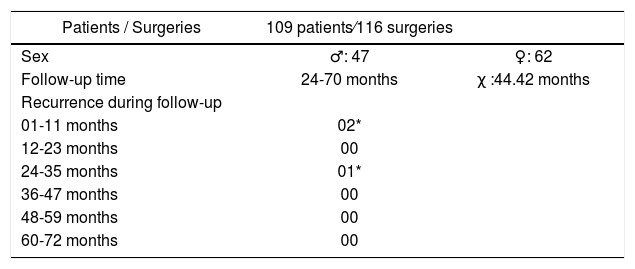
One surgery was excluded due to the patient dying before the procedure completed one year. Of the 116 interventions included in the study, none were followed for less than 24 months, including a previous procedure for the same patient who died (47 months of follow-up) (Table 1). The mean time of follow-up was 44.42 months (24-70 months).
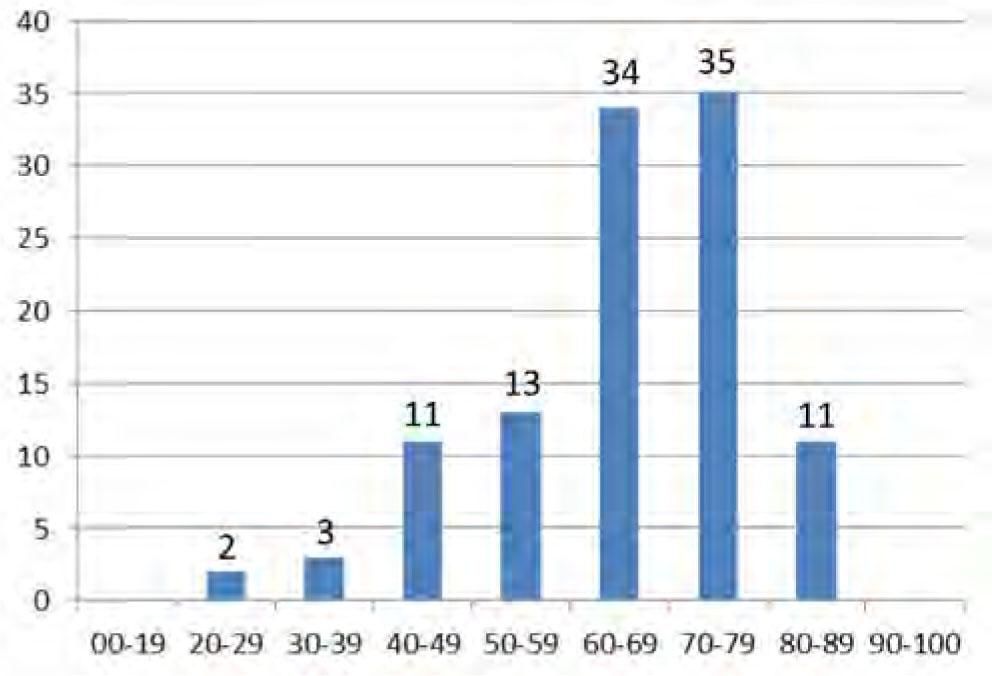
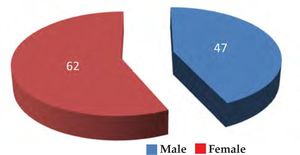
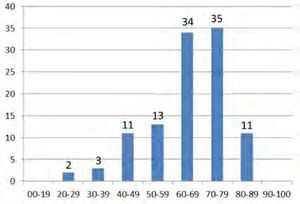
There were 43% of male patients and 57% of female patients, but without statistically significant difference (p = 1.0) between age and sex (Figure 1). The mean age was 65.48 years (29-88 years) and the most affected age group was 60-79 years, significant in relation to the sum of other decades of life (p = 0.008) (Figure 2).
Regarding the location of the lesions, the cephalic segment was predominant (101 lesions, 87.07%) in relation to the other body segments, followed by the trunk (9 lesions, 8.29%) and upper limbs (6 lesions, 5.17 %). The variables, cephalic segment and female sex, were significant (p = 0.04).
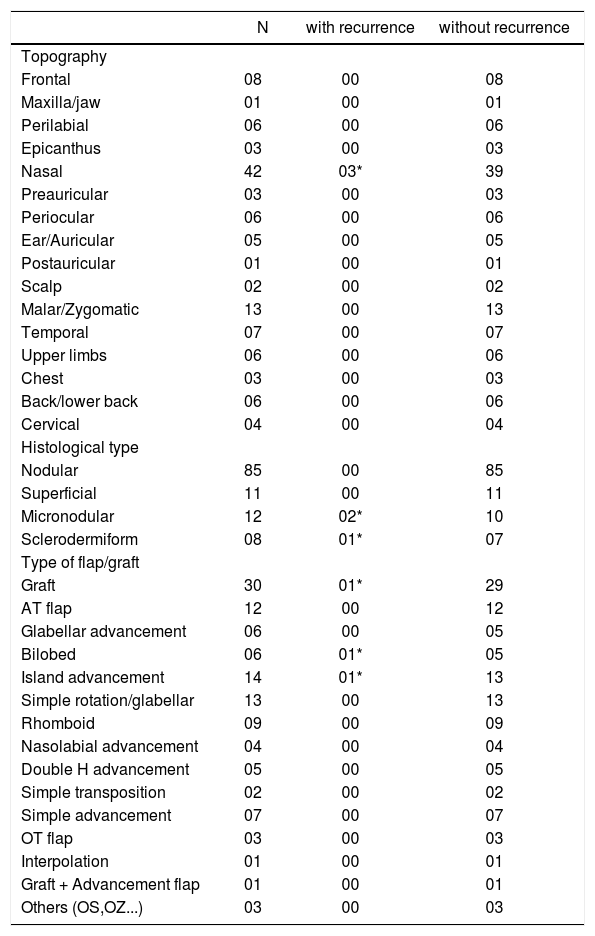
The predominant histopathological type in the study was nodular (85 lesions, 73.28%). The most aggressive forms (micronodular and sclerodermiform) accounted for 20 lesions (17.24%) and were statistically significant when compared to the other subtypes in relation to recurrence (p = 0.0001). Of these, three (2 micronodular and 1 sclerodermiform) recurred on the nasal region and the other 10 micronodular forms and 7 sclerodermiform forms, located on extra-nasal regions, did not recur (Table 2). When comparing the nasal region to other sites of the body in relation to recurrence, the nose was significant (p = 0.02). Recurrences occurred after 6 months (2 cases) and 25 months (1 case) of the surgery (Table 1).
Relation of the location, recurrences, histological type and procedures performed
| N | with recurrence | without recurrence | |
|---|---|---|---|
| Topography | |||
| Frontal | 08 | 00 | 08 |
| Maxilla/jaw | 01 | 00 | 01 |
| Perilabial | 06 | 00 | 06 |
| Epicanthus | 03 | 00 | 03 |
| Nasal | 42 | 03* | 39 |
| Preauricular | 03 | 00 | 03 |
| Periocular | 06 | 00 | 06 |
| Ear/Auricular | 05 | 00 | 05 |
| Postauricular | 01 | 00 | 01 |
| Scalp | 02 | 00 | 02 |
| Malar/Zygomatic | 13 | 00 | 13 |
| Temporal | 07 | 00 | 07 |
| Upper limbs | 06 | 00 | 06 |
| Chest | 03 | 00 | 03 |
| Back/lower back | 06 | 00 | 06 |
| Cervical | 04 | 00 | 04 |
| Histological type | |||
| Nodular | 85 | 00 | 85 |
| Superficial | 11 | 00 | 11 |
| Micronodular | 12 | 02* | 10 |
| Sclerodermiform | 08 | 01* | 07 |
| Type of flap/graft | |||
| Graft | 30 | 01* | 29 |
| AT flap | 12 | 00 | 12 |
| Glabellar advancement | 06 | 00 | 05 |
| Bilobed | 06 | 01* | 05 |
| Island advancement | 14 | 01* | 13 |
| Simple rotation/glabellar | 13 | 00 | 13 |
| Rhomboid | 09 | 00 | 09 |
| Nasolabial advancement | 04 | 00 | 04 |
| Double H advancement | 05 | 00 | 05 |
| Simple transposition | 02 | 00 | 02 |
| Simple advancement | 07 | 00 | 07 |
| OT flap | 03 | 00 | 03 |
| Interpolation | 01 | 00 | 01 |
| Graft + Advancement flap | 01 | 00 | 01 |
| Others (OS,OZ...) | 03 | 00 | 03 |
The skin graft was the most used type of reconstruction (in 30 cases, 25.86%) and there was no significant relationship between recurrence and this type of reconstruction (p = 0.88) (Table 2).
DiscussionDepending on the location and size of the BCC, surgical reconstruction requires grafts or skin flaps. The literature does not separate recurrence rates only by considering this type of procedure (recurrence rates published include excision with primary closure, curettage, cryosurgery, as well as skin flap and graft jobs). Tumor recurrences are problems and great challenges for patient follow-up, especially when it is necessary to perform more complex surgeries to close the surgical wound.
Although other types of procedures were excluded, our sample showed a mean age of 65.48 years (29-88 years) and the age group most affected of 60-79 years, corroborating with the group of other studies of BCC.2,3
Although the literature shows numerical superiority in men1, other studies demonstrate the prevalence of female sex, as in our case (57% female).2,3 Mantese et al suggests that the explanation would be that the female population is a target audience for prevention campaigns, which makes them more aware of the first signs of skin cancer.2
The present study showed a predominance of lesions in the cephalic segment (p <0.05), the most common site of BCC according to the literature, in view of the greater exposure and cumulative effect of solar rays.1-3,5-10
The nodular histopathological type predominated in the study (85 lesions, 73.28%), in accordance with other studies.2,8 The micronodular and sclerodermiform subtypes considered as aggressive forms8,11,12 accounted for 20 lesions (17.24%), and were associated to recurrences (p <0.05). The nasal region, site of the 3 relapses in the study (p <0.05, Fisher’s Exact Test), is cited in the literature as a risk factor, considering the difficulty of surgical margins due to local anatomy, or concern about the aesthetic outcome.2,3,8
Although the histopathological margins of our nasal recurrences were not affected at the time of the intervention, because the micrographic method was not used, the slides made by sampling could have failed to visualize a site involved and explain their recurrences.13,14
Ocanha et al5 presented 25 relapses in their study, in which one-third had relapsed in the first postoperative year. However, in the same study, the compromised margins were related to the recurrences and were not separated from the more complex surgeries. The reason that one of our exclusion criteria was follow-up of less than 12 months (but the minimum follow-up was 24 months in the study) was that the recurrence rate was high in the first year, although we agreed that the ideal follow-up would be five years or more. Our recurrences occurred 6 months (2 cases) and 25 months (1 case) after the surgery (Table 1).
Table 2 shows the types of reconstructions used and were chosen according to the best situation for each occasion. Although the graft was the most prevalent (in 30 cases, 25.86%), there was no significant relationship between relapse and this type of reconstruction (p = 0.88).
Despite the low recurrence rates (2.6%), the authors still recommend Mohs micrographic surgery, as it could save healthy tissue adjacent to the tumor and avoid the need for a skin flap or graft, in addition to near 99% cure.13,14 But we hope to have contributed to the better understanding of the natural history of BCC when using more complex reconstructions in conventional surgery.
ConclusionThe present study of the dermatology department of this university hospital showed low rates of recurrence of BCC in those cases where flaps and/or grafts were used in the surgical reconstruction with pre-established margins (by the conventional method). Recurrence was related to the site (nasal region) and more aggressive histological type (micronodular and sclerodermiform).
Financial support: None.
Conflict of Interest: None