Pseudoxanthoma elasticum-like papillary dermal elastolysis is an acquired elastic tissue disorder clinically similar to pseudoxanthoma elasticum in the absence of systemic involvement. Histopathologically, special staining of elastic fibers demonstrates a total or partial band-like loss of elastic fibers in the papillary dermis. Although ultraviolet radiation seems to be one of the main etiological factors in this entity, we report a case of pseudoxanthoma elasticum-like papillary dermal elastolysis on the neck of a woman who wore hijab.
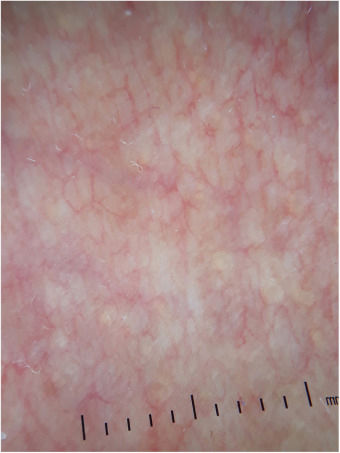
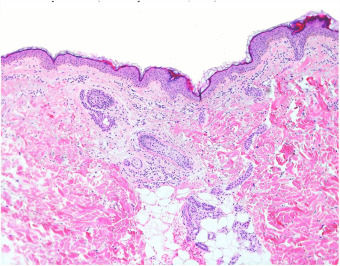
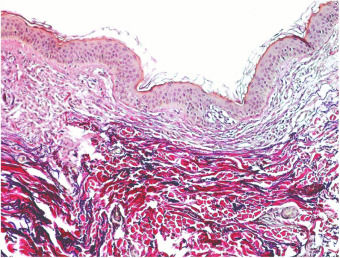
A 54-year-old female of Moroccan origin who habitually wears a hijab presented a 2 year history of mildly pruritic lesions on the neck. She denied systemic symptoms and family history of similar findings. Her medical history included mixed anxiety-depressive disorder treated with olanzapine and sertraline. Physical examination revealed white-to-yellowish millimetric non-follicular papules on the lateral aspects of the neck and supraclavicular fossae (Fig. 1). Dermoscopic examination showed multiple white-colored non-follicular papules, coalescing into plaques with arboriform vessels (Fig. 2). The biopsy showed slight sclerosis of the papillary dermis with neovascularization and a mild inflammatory infiltrate including lymphocytes and some melanophages (Fig. 3). In the same area, van Gieson stain demonstrated a decrease in the number of elastic fibers that were often thin and fragmented (Fig. 4) compatible with pseudoxanthoma elasticum-like papillary dermal elastolysis (PXE-PDE). Cardiac and ophthalmological investigations performed were unremarkable.
PXE-PDE is a rare acquired elastic tissue disorder characterized by non-follicular yellowish papules coalescing into plaques with predilection for neck, supraclavicular fossae and flexural areas.1 The lesions are usually asymptomatic, but mild itch is sometimes reported, as seen in our case. To date, it affects exclusively women mostly in middle age2 and it is not associated with any systemic involvement. Dermoscopic findings consist of multiple white-colored non-follicular papules, coalescing into plaques with linear vessels.3
Histopathologically, hematoxylin eosin staining does not reveal any specific changes. The focal inflammatory changes present in our case have not been described previously; however, it is presumed that elastic fiber loss could be the result of a transient phenomenon of inflammation. Special staining of elastic fibers with van Gieson or orcein stains are required to demonstrate a total or partial band-like loss of elastic fibers in the papillary dermis.2 Calcification or fragmentation of the elastic fibers is absent. Immunohistochemical studies using monoclonal antibodies against antibody P component can also demonstrate partial or complete loss of elastic fibers in papillary dermis.1 The presence of melanophages in the papillary dermis constitutes an additional helpful diagnostic feature.4
The cause of PXE-PDE remains unclear, and some etiopathogenic theories have been proposed: ultraviolet radiation, intrinsic aging, abnormal elastogenesis, and genetic or inheritable factors.1,2 In our case, ultraviolet radiation's etiopathogenic theory is unlikely because the patient wore hijab.
Differential diagnosis of PXE-PDE includes white fibrous papulosis of the neck, mid-dermal elastolysis, and papillary dermal elastosis. Nevertheless, the main differential diagnosis must be established with pseudoxanthoma elasticum (PXE), a hereditary disorder caused by mutation on ABCC6 gene. Clinically, PXE resembles PXE-PDE, but it appears at a younger age, and it is usually associated with ocular and cardiovascular complications. Histopathologically, PXE presents fragmentation and calcification of elastic fibers demonstrated with von Kossa stain.
Treatments for PXE-PDE, including topical retinoids, have shown poor results2; however, non-ablative fractional resurfacing laser has demonstrated to be effective in some cases.5
Herein we present a case of PXE-PDE in a patient who did not receive UV radiation because she wore hijab. In our opinion, more studies are needed in order to better understand the etiopathogenesis of PXE-PDE. It is important that dermatologists recognize this entity and differentiate it from PXE to avoid unnecessary investigation. Clinicopathologic correlation is important and elastic tissue stains are required to correctly diagnose PXE-PDE.
Financial supportNone declared.
Authors’ contributionsNuria Setó Torrent: Approval of the final version of the manuscript; elaboration and writing of the manuscript; intellectual participation in the propaedeutic and/or therapeutic conduct of the studied cases; critical review of the literature; critical review of the manuscript.
Maribel Iglesias Sancho: Approval of the final version of the manuscript; critical review of the manuscript.
Jorge Arandes Marcocci: Approval of the final version of the manuscript; critical review of the manuscript.
María Teresa Fernández Figueras: Approval of the final version of the manuscript; critical review of the manuscript.
Conflicts of interestNone declared.
How to cite this article: Setó-Torrent N, Iglesias-Sancho M, Arandes-Marcocci J, Fernández-Figueras MT. Pseudoxanthoma elasticum-like papillary dermal elastolysis in non-exposed skin. An Bras Dermatol. 2020;95:247–9.
Study conducted at the Hospital Universitari Sagrat Cor-Grupo Quirón Salud, Barcelona, Spain.