Extranodal NK/T-cell lymphoma nasal type is a rare disease that mainly affects the nasal cavity and paranasal sinuses of males in the fifth decade of life. It has aggressive and locally destructive behaviour, and can be complicated by the hemophagocytic syndrome, conferring high lethality to the disease. This article describes a case of NK/T-cell lymphoma nasal type in a previously healthy patient, exemplifying its rapid and fulminant course.
NK/T- cell lymphoma is a rare condition, more common in Asia and Latin America that represents from 3% to 10% of all non-Hodgkin lymphomas in those areas, and only 1% in Europe and North America.1–6 The tumor affects more commonly male adults (3:1) in the fifth decade of life and mainly involves the nasal cavity and paranasal sinuses.1–4
Because of its aggressiveness and local destruction, it was historically known as “lethal midline granuloma”, together with conditions that affect the central region of the face, such as Wegener’s granulomatosis and tegumentary leishmaniasis.1,2 Symptoms are non-specific in the majority of cases and the clinical picture unfolds with rhinorrhea, nasal obstruction and epistaxis, mimicking an upper airway infection.1,2 With the progression of the disease, extensive necrotic areas develop, and the prognosis becomes poor, with low survival.1,2 The hemophagocytic syndrome, characterized by the activation of the mononuclear phagocyte system, can overlap, leading to even more unfavorable outcomes.
Case ReportA 46-year-old male patient with nasal congestion and refractory sinusitis for 2 years, for which he was being treated with multiple antibiotics, was shown. As past history, there was septoplasty five years prior and systemic hypertension. He reported worsening of the nasal obstruction, dysphagia, dysphonia, facial edema and enlarged cervical lymph nodes in the last two months. He was admitted in the emergency department with profuse oral cavity bleeding and facial edema, with the indication for urgent tracheostomy. On dermatological examination, there was an erosive lesion on the nasal region, perinasal crusts and perforation of the nasal septum (Figures 1 and 2).
Computed tomography imaging (CT) of the paranasal sinuses showed a fracture of the nasal bone, anterior portion of the nasal septum, frontal process of the right maxilla and of the anterior nasal spine; thickening of the soft tissue of the nasal pyramid; fracture of the posterior-lateral wall of the right orbit; bilateral maxillary and ethmoid hemosinus; blood density material in the nasal fossae; and normal nasal cavity. Head CT scan showed no abnormalities.
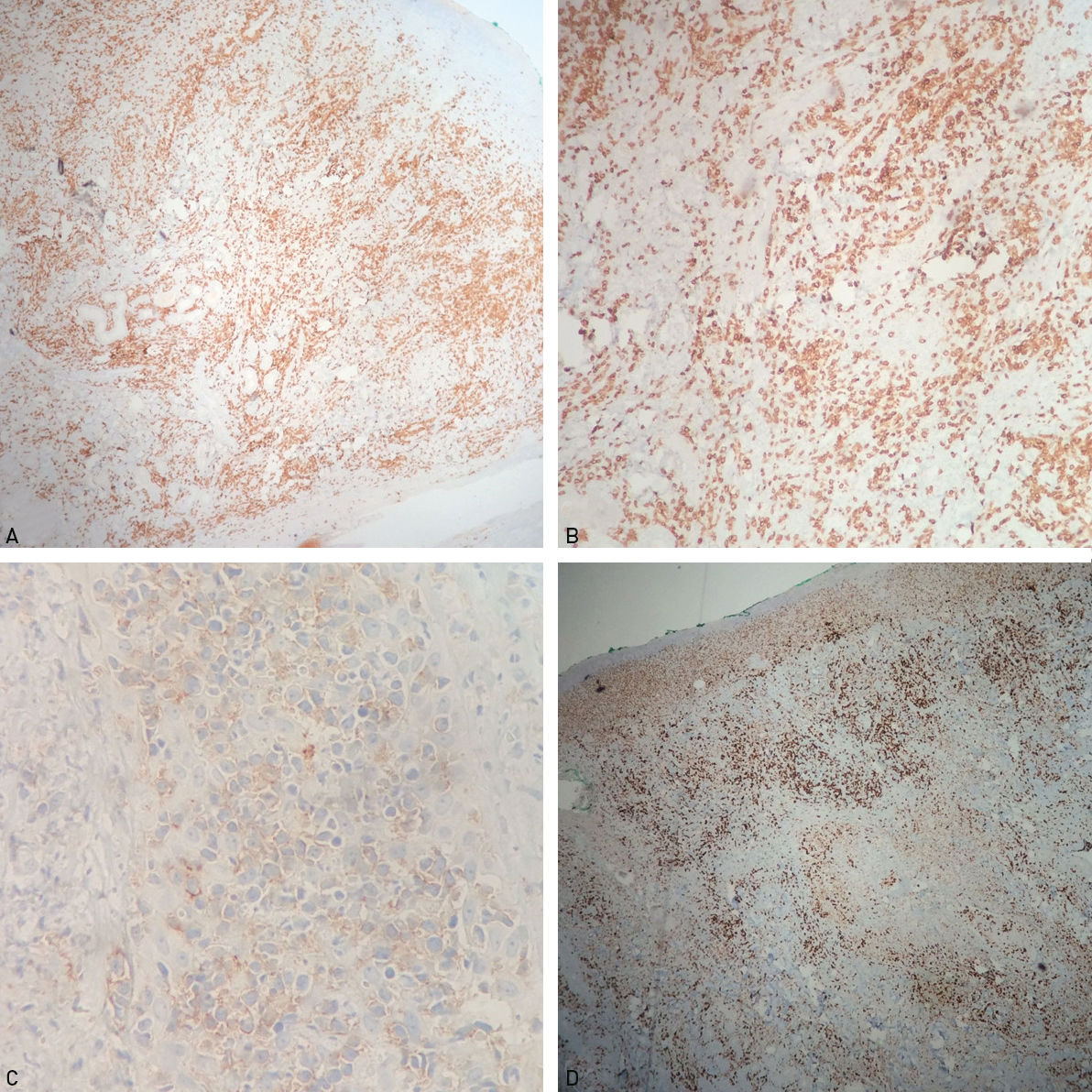
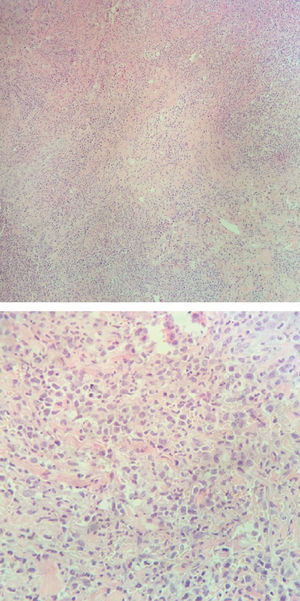
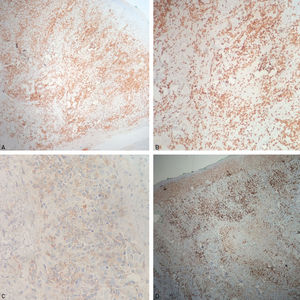
The patient underwent an incision biopsy of the perinasal area for culture and histopathology, which revealed an infiltrate with atypical small and medium lymphoid cells in the deep dermis and some large pleomorphic lymphocytes (Figure 3). Immunohistochemistry was positive for CD3, CD7, CD30, CD8 (weak), CD2, granzyme B, EBV-LMP1 and CD56 (weak) and negative for myeloperoxidase, CD68, CD15, CD99, CD10, CD20, CD5 and CD4. The Ki-67 proliferative index was 70% (Figure 4). Special staining for fungi were negative. These findings supported the diagnosis of NK/T-cell lymphoma, nasal type.
Baseline laboratory tests did not show any significant abnormalities, except for a platelet count of 88,000. During admission, the patient evolved with acute renal failure, liver failure, hyperbilirubinemia, thrombocytopenia and disseminated intravascular coagulation (DIC). Death occurred in less than 30 days of admission.
DiscussionAccording to the WHO-EORTC primary cutaneous lymphoma classification, revised in 2008, extranodal NK/T-cell lymphoma, nasal type is a clinically aggressive lymphoma from natural killer cells (NK) or, more rarely, from cytotoxic T lymphocytes.2,5 It typically affects the nasal and paranasal regions, but it can also affect the lungs, gastrointestinal tract, testicles, kidneys, pancreas, central nervous system and skin,2–6 the latter being the second most commonly involved area after the nasal cavity.2,3 Cutaneous lesions can also be similar to those seen in mycosis fungoides.3 Enlarged lymph nodes can be seen, particularly in patients with nasal involvement, and they can be inflammatory or related to the tumor.1
Initial symptoms are not specific, such as rhinorrhea, nasal obstruction and epistaxis,1 seen in this reported case. The clinical picture is often mistaken by sinusitis and airway infection, and the patients are frequently treated with multiple antibiotic courses, what delays the diagnosis of lymphoma.1,4,6 With the progression of the disease, edema, necrosis and destruction of the surrounding tissues appear, what can progress with destruction of the nasal wall and oronasal fistulas, besides fever and weight loss.1,4
The association of the pathogenesis of the tumor with Epstein-Barr virus (EBV) infection is well established in the literature.1–3 On the histopathology, extranodal NK/T-cell lymphoma presents with a mixed cellular infiltrate, with atypical lymphocytes, plasma cells, eosinophils and histiocytes, besides the common angiocentric and angiodestruction features.1,2,4,5 Immunohistochemistry is positive for CD45Ro, CD3, CD7 and CD56, besides Eber and cytotoxicity markers such as TIA-1 and granzyme B.4,5 Proliferation index, KI-67, tends to be elevated. Considering the clinical picture of the reported patient, along with the histological and immunohistochemistry findings, besides the association with EBV infection demonstrated by the marker EBV-LMP1, it was possible to confirm the diagnosis of extranodal NK/T-cell lymphoma, nasal type.
The marked destructive capacity of the tumor is responsible for its high mortality, that can be worsened by the hemophagocytic syndrome, a hyperinflammatory and aggressive condition usually secondary to lymphomas, viral infections (especially EBV infections) and autoimmune conditions.7–9 The form related to lymphomas is more common in non-Hodgkin lymphomas and can be seen in patients with NK/T-cell lymphoma, nasal type, relatively frequently.7,10 The syndrome is triggered by abnormalities in multiple cytokines, generating the activation of T lymphocytes and histiocytes, as well as an increase in interferon gamma, tumor necrosis factor alpha and interleukins 6, 10 and 12.10 The clinical and laboratory findings are fever, pancytopenia, raised ferritin levels, low fibrinogen levels, liver abnormalities, coagulation disorders and renal dysfunction, such as in our patient.7–9 The syndrome is frequently related to a poorer prognosis and unfavorable outcome.8,9
Treatment protocols for NK/T-cell lymphoma are yet not well established, but combinations of radiotherapy and chemotherapy are routinely used, and bone marrow transplant has been investigated.1,6 However, prognosis remains poor due to the rapid and aggressive course of the disease, with high rates of failure to the multidrug chemotherapy regimens.3,5 Mean survival estimated in the literature is of 12.5 months;2,5 5-year survival is between 20% to 65%.1 Therefore, it is extremely important to consider this diagnosis in patients with refractory sinusitis or destructive lesions on the central region of the face, that can be easily mistaken with paracoccidioidomycosis, tegumentary leishmaniosis, Wegener’s granulomatosis and other conditions, in order to provide an earlier diagnosis and allow better chances for treatment.