Primary cutaneous lymphoepithelioma-like carcinoma is a rare disease with low metastatic potential. Its morphologic and pathological features are similar to those of nasopharyngeal lymphoepithelial carcinoma. We report the case of a 60-year-old man with an infrapalpebral pearly papule, measuring 0.6 cm in diameter. The lesion was excised with a clinical hypothesis of basal cell carcinoma or squamous cell carcinoma. Histopathological analysis revealed a malignant neoplasm with syncytial arrangement of cells with vesicular nuclei, associated with dense lymphocytic infiltrate. Immunohistochemistry revealed cytokeratin-positive cells (AE1/AE3) and p63 protein, indicating epithelial histogenesis and squamous differentiation. A negative Epstein-Barr virus test result was achieved by immunohistochemistry. Primary lymphoepithelioma-like carcinoma of the skin is a differential diagnosis of lesions with prominent inflammatory infiltrates.
Lymphoepithelioma-like carcinomas are poorly differentiated malignant neoplasms whose morphology exhibits prominent reactive lymphoplasmacytic infiltrates and are usually found in the nasopharyngeal region.1 However, the lesion has been reported in other sites such as the salivary glands, thymus, tonsils, and cervix. Lymphoepithelioma-like carcinoma affecting the skin was first reported in 1988 when Swanson et al. published a series of five patients.2 Gille et al. recently reviewed approximately 60 cases.3 This article is a report of a Brazilian patient affected by this neoplasm.
Case ReportWe report a 60-year-old male patient with an erythematous papule located inferiorly to the left eyelid measuring 0.6 cm in diameter (Figure 1). He underwent excisional biopsy with clinical suspicion of squamous cell carcinoma or basal cell carcinoma.
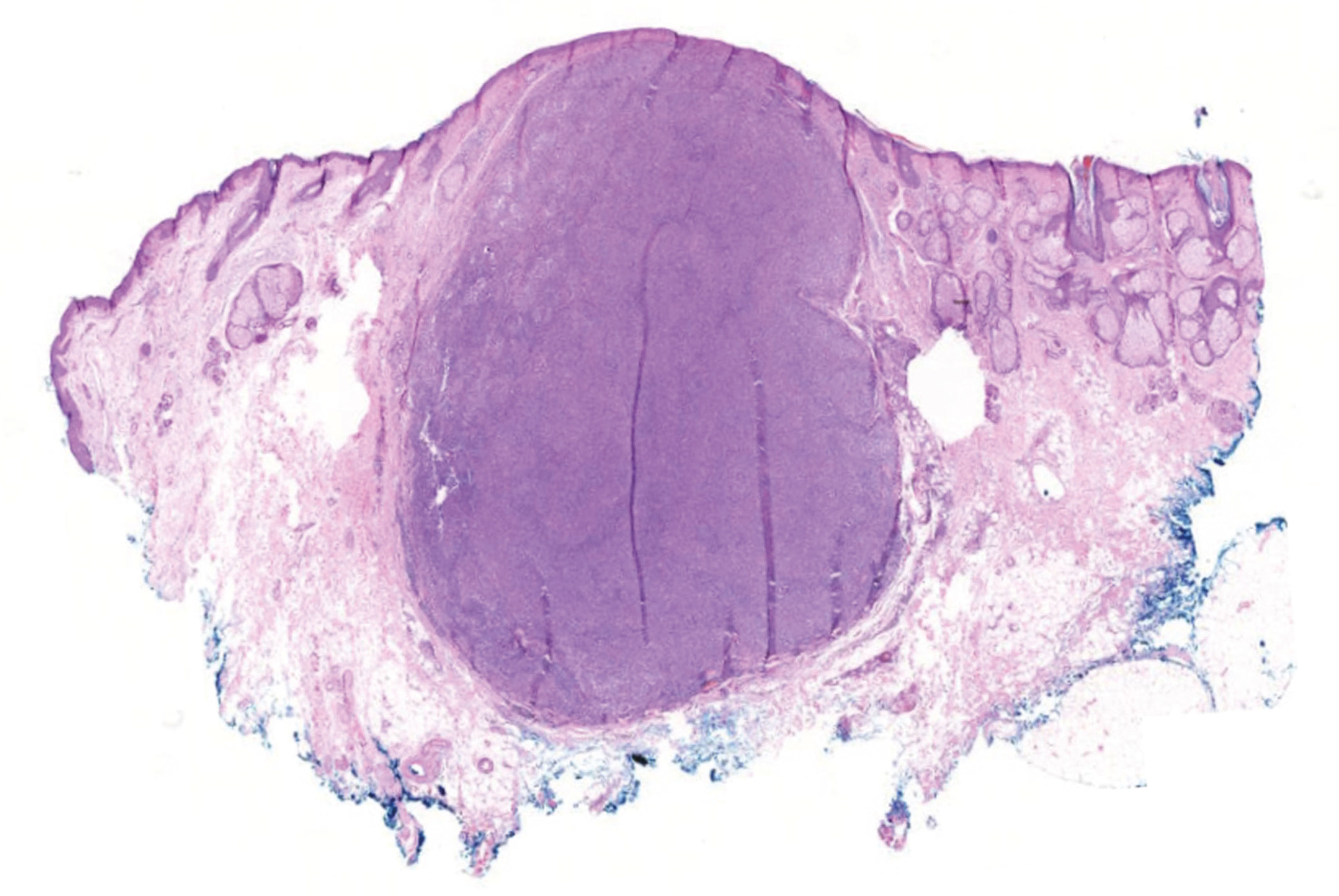
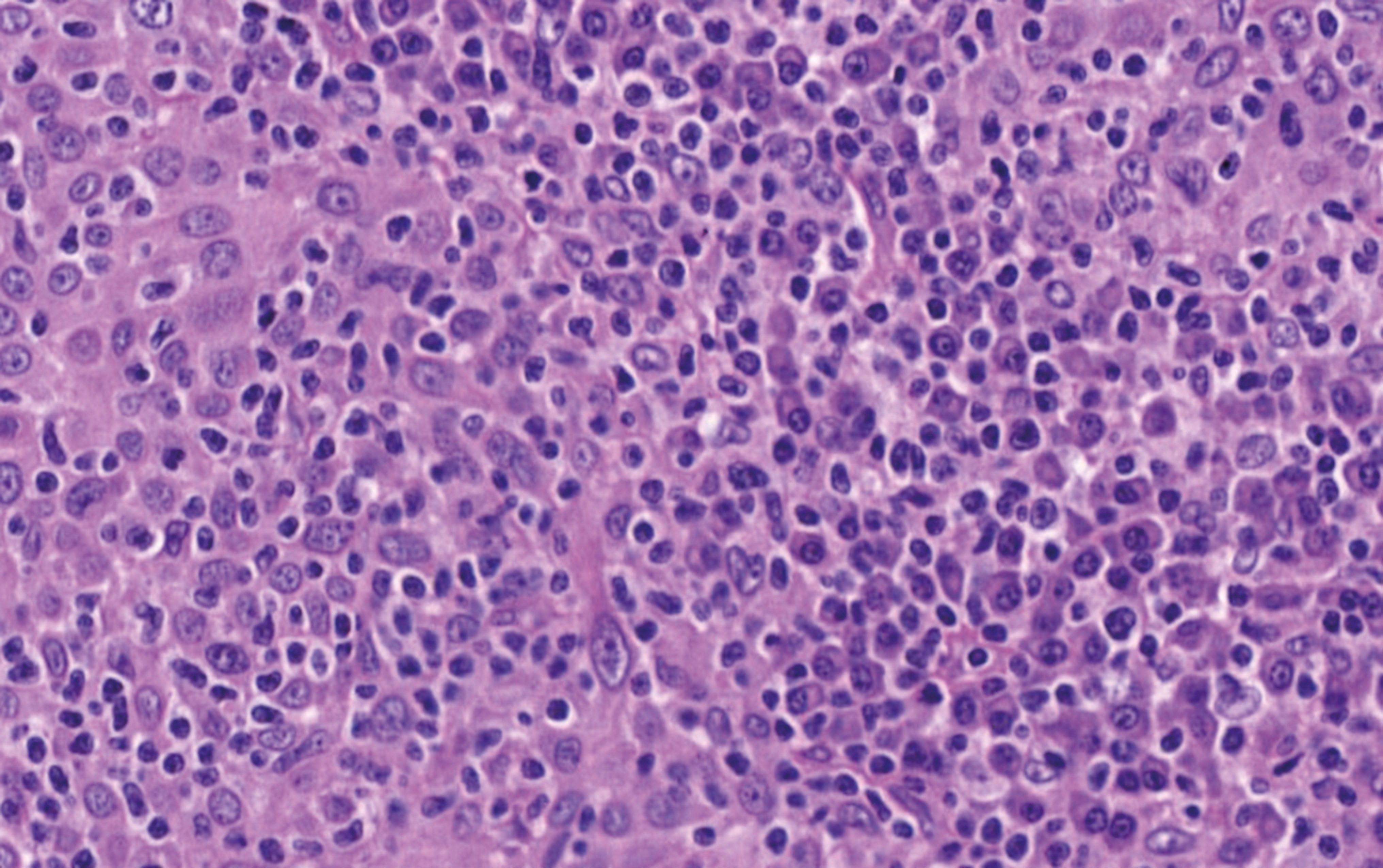
Morphological evaluation showed a circumscribed tumor with an expansive pattern of growth in the dermis, with no connection to the epidermis (Figure 2). We observed atypical malignant epithelial cells with large and vesicular nuclei in syncytial arrangement. A prominent inflammatory infiltrate, predominantly lymphocytic, surrounded the neoplastic epithelial blocks, in a reactional pattern (Figure 3).
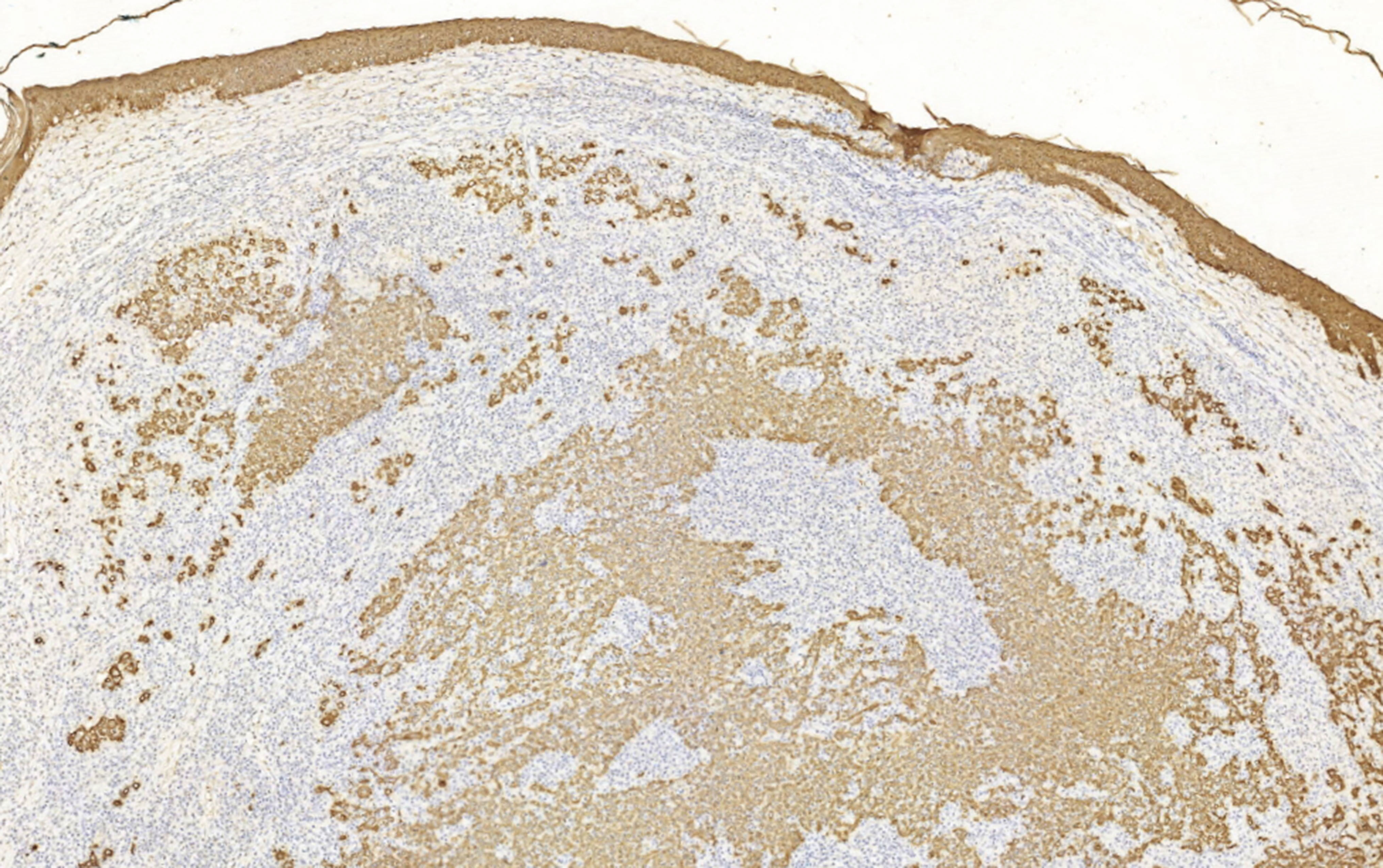
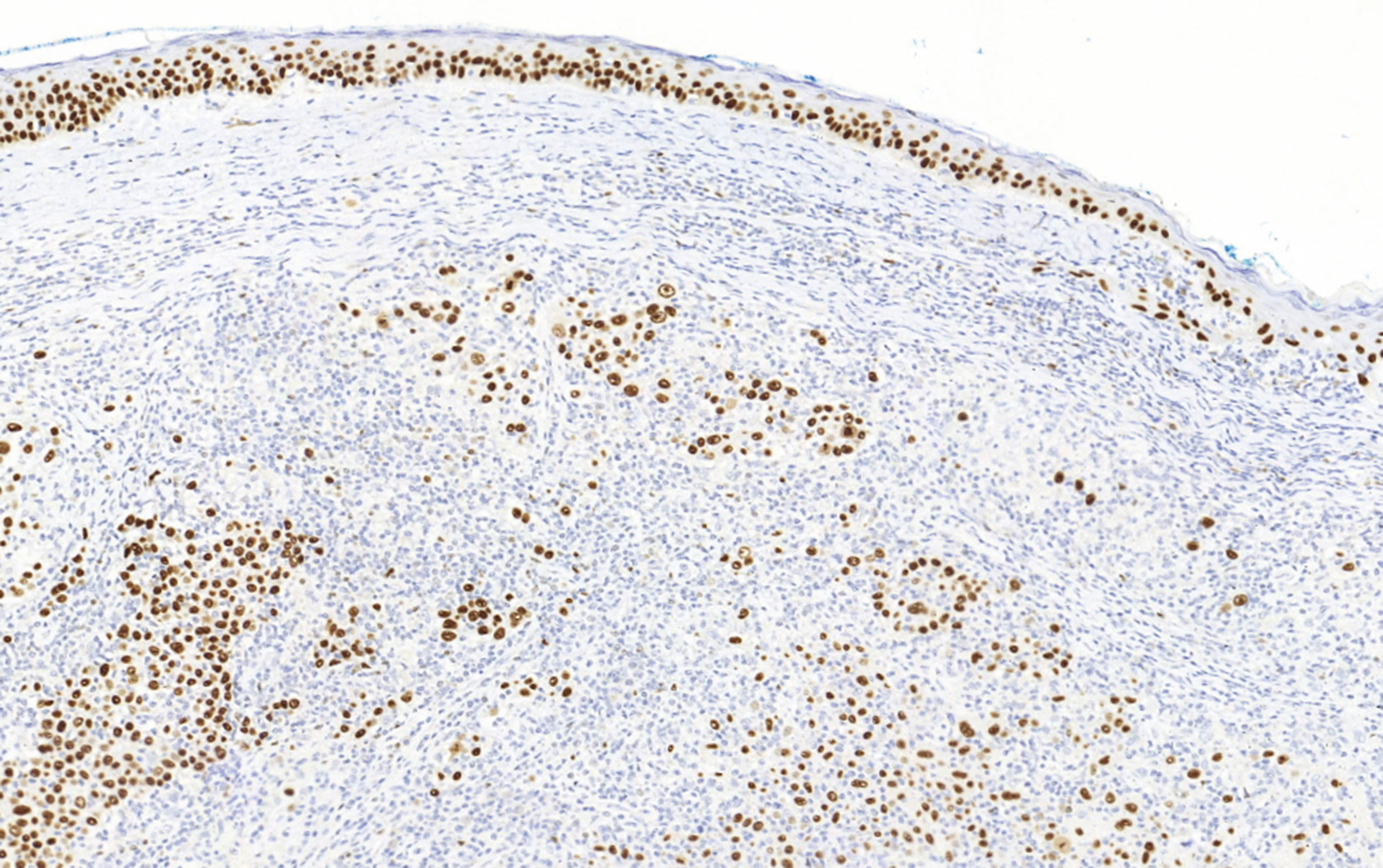
Immunohistochemical study was performed to confirm the epithelial histogenesis of the lesion. The patient was positive for cytokeratins (AE1/AE3), indicating the diagnosis of carcinoma (Figure 4). Squamous differentiation was confirmed by the positive p63 results (Figure 5). The prominent inflammatory infiltrate was positive for CD45, but the analyzed neoplastic cells showed a negative result for the same marker. Immunohistochemistry performed to investigate Epstein-Barr virus was negative for LMP-1 expression.
Morphological and immunophenotypic findings supported the diagnosis of lymphoepithelioma-like carcinoma of the skin. The patient was screened for possible primary lesion of the nasopharynx. Based on the negative results for nasopharyngeal cancer or other types of tumors, a primary cutaneous carcinoma was confirmed. The patient had a favorable evolution, without relapses or lymph node involvement.
DiscussionSquamous cell carcinoma of the skin is a malignant neoplasm with variable clinical behavior, ranging from indolent to aggressive tumors with considerable metastatic potential.4 According to a classification proposed by Cassarino et al., lymphoepithelioma-like carcinoma is a variant with intermediate malignant potential, with an estimated 5-10% risk of metastasis.4
Lymphoepithelioma-like carcinoma is an uncommon cutaneous neoplasm, generally affecting individuals over 50 years of age, with no gender predilection.5 The etiology of this squamous cell carcinoma variant is still uncertain. Ho et al. discussed two theories6. One of them inferred an epidermal origin, but this hypothesis is contradicted by the absence of connection between the lesion and the epidermis in cases reported in the literature. The other theory suggests an adnexal origin, corroborated by the identification of areas of adnexal differentiations in some of the tumors previously described.6,7
Clinically, these cutaneous lesions are usually located on the scalp and in the neck region. The trunk and extremities are also reported as preferential sites.3 This lesion has also a tendency to appear in areas of greater sun exposure. Clinical manifestations include erythematous nodules, plaques, or papules, with months of evolution.3 The patient presented had had an erythematous papule for five months, which is, according to the literature, the most common presentation.3,5,6,8,9
Morphology of these neoplasms is similar to that observed in other topographies, including the nasopharynx.6,10,11 The lesions tend to be well-delimited dermal nodules composed of syncytial-like epithelial arrays arranged in the midst of inflammatory lymphocytic infiltrates, sometimes with associated plasma cells.11 The syncytial aspect of epithelial clusters is quite characteristic of this type of neoplasia. The cytological pattern of our case is quite typical: large vesicular nuclei with evident nucleoli. The inflammatory infiltrate observed in these neoplasms has a reactive behavior and, in general, is predominantly composed of T lymphocytes, which are also dominant in healthy skin samples.12
Some differential diagnoses should be considered for these lesions. Lymphomas are an example due to the exuberant inflammatory infiltrate and the poorly differentiated large cells. Other possibilities include follicular dendritic cell tumors and Merkel cell carcinoma. For these hypotheses, immunohistochemical examination is a helpful elucidative tool.12
The evidence of epithelial cells is indicated by markers such as cytokeratins (AE1/AE3), cytokeratins 5/6 (CK 5/6), and epithelial membrane antigen (EMA). The identification of atypical cells with vesicular and epithelial nuclei undermines the diagnosis of lymphomas and follicular dendritic cells tumors. Merkel cell carcinoma, although epithelial, generally has a connection with the epidermis, hyperchromatic nuclei, absence of inflammatory infiltrate, and immunopositivity for neuroendocrine markers. P63 is very useful in this context: lymphoepithelioma-like carcinomas have p63 nuclear positivity, confirming their squamous differentiation. On the other hand, tumors that display neuroendocrine differentiation are negative for this marker.12
Lymphoepithelioma-like carcinoma of the skin diagnosis requires clinical investigation of the primary lesion – mainly of the nasopharynx – by imaging and laryngoscopy.11,12 In the absence of lesions in other locations, the case is considered as primary cutaneous. The most commonly treatment procedure is excisional biopsy.11 Patients, most of the time, have a good prognosis, without recurrences or metastases.3,5,9,11,12 Cases of local aggressiveness and metastasis are uncommon. An example is the patient reported by Hall et al.,13 whose clinical presentation was initially metastasized. For severe cases, which are infrequent, radiotherapy can be used with positive results.9,11
Epstein-Barr virus (EBV) role in the pathogenesis of this neoplasm affecting the skin has not been documented yet. Unlike the nasopharynx, different studies3,6,11,14,15 on these cutaneous neoplasms failed to prove the association with the virus, like in our case. For topographic sites such as the lung, stomach, and salivary gland, this relationship has already been established.14
The present case is not rare, but unusual. The infrequency may lead pathologists and dermatologists to neglect this entity. Reports of different experiences with this tumor make it possible to know their different forms of manifestation – which are not always typical – and contribute to the knowledge of the disease.
Financial support: None.
Conflict of interest: None.