Trichilemmal carcinoma is a rare adnexal neoplasia with histologic features reminiscent of the outer root sheath of hair follicles. The clinical presentation of trichilemmal carcinoma is variable, as it may mimic basal cell carcinomas and squamous cell carcinomas, thus requiring histologic diagnosis. We report the case of a patient with aggressive trichilemmal carcinoma in the auricle.
Trichilemmal carcinoma (TC)—also known as trichilemmocarcinoma—is a rare neoplasm that manifests as an asymptomatic exophytic or polypoid mass located in sun-exposed areas in older adults. TC may mimic basal or squamous cell carcinomas, keratoacanthomas and proliferating pilar tumors (PPT).1,2 While described as locally destructive, surgical excision is reported to have positive clinical outcomes with low metastatic and recurrence rates.1–5 Herein, we report the first Colombian case of a TC in an older adult, involving the retroauricular region.
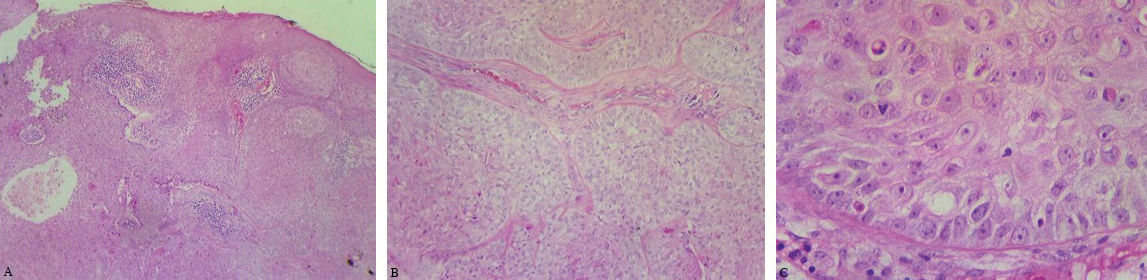
Case ReportAn 84-year-old man presented to our clinic with a 5-year history of an ulcerated tumor arising from his left retroauricular region, with local destruction of the auricle (Figures 1 and 2). One year before, a biopsy performed at another institution reported it as a sclerodermiform basal cell carcinoma with squamous differentiation. A new biopsy was performed, identifying a multilobular tumor with polygonal cells, palisade arrangement with focal inversion, and a thick hyaline membrane surrounding each lobule; some segments with foci of trichilemmal keratinization, cytological atypia, high mitotic index and atypical mitotic figures (Figure 3). These findings were compatible with a TC. A head-and-neck computed tomography (CT) scan showed no other pathological findings. The patient underwent total auriculectomy, parotidectomy and lymphadenectomy.
Histopathological features. (A) Lobular lesion with connection to epidermis, comprising polygonal cells with atypical nuclei, increased mitosis, peripheral palisading, with foci of trichilemmal keratinization. (Hematoxylin & eosin, x4). (B) Tumor lobules surrounded by hyaline basement membrane (Hematoxylin & eosin, x10). (C) Tumor cells with several atypical mitoses (Hematoxylin & eosin, x40)
Malignant hair follicle tumors account for 1% of adnexal carcinomas.6 Prior to 2014, a total of 103 cases of TC had been reported; 60% of these cases occurred in men, 51% involved the face, and the average age of the patients was 72.5 years.1 Although the pathogenesis remains unclear, documented risk factors are ultraviolet radiation, solid organ transplant, immunosuppression, scars, burns, and genetic diseases like xeroderma pigmentosum and Cowden disease.1 TC may also develop on seborrheic keratosis, nevus sebaceous, discoid lupus scarring and tuberculosis verrucosa cutis.1,3,7,8
Clinical manifestations are variable, mimicking basal or squamous cell carcinomas, keratoacanthomas and nodular melanomas, but TC usually behaves as a benign tumor and is amenable to curative resection with conventional surgery. Some authors suggest that safety margins greater than 1 cm are associated with increased overall survival.1,4,5,8,9 Nonetheless, safety margins of 1 cm have been used safely and cost-effectively.4 However, over the past decade, Mohs micrographic surgery has been shown to have higher recurrence-free rates, becoming the gold standard treatment to preserve the surrounding healthy tissue.1,5 Additional therapeutic approaches include treatment with 5% imiquimod applied three times per week for eight weeks, for which no relapse has been observed at sixteen-month follow-up, and adjuvant radiotherapy for patients with high-risk disease.1,10 Since there are few articles reporting metastatic disease, magnetic resonance imaging and CT scan have been proposed as additional work-up studies for patients with TC.6 There are currently no guidelines for treatment or follow-up of TC, but it is recommended that these tumors be treated as non-melanoma skin cancers.1
Unlike the usually less aggressive behavior of trichilemmal carcinomas reported throughout the literature, our patient presented with a locally aggressive tumor that, considering the previous biopsy reporting the lesion as a sclerodermiform basal cell carcinoma with squamous differentiation, posed a diagnostic challenge.
In conclusion, this is a case of a locally aggressive trichilemmal carcinoma. Although initially diagnosed as a basal cell carcinoma, the tumor had histopathological features comparable to those reported throughout the literature for trichilemmal carcinoma, strongly supporting the diagnosis of this rare entity, which remains a challenge for dermatologists and pathologists.
Financial support: None.
Conflict of interests: None.