Granuloma annulare is a relatively common, idiopathic, benign inflammatory dermatosis, with a varied clinical presentation that often makes diagnosis difficult. It mainly affects the extremities, such as the dorsa of the hands and feet, forearms and legs. Palmar and plantar regions are generally spared. It occurs mainly in young female patients. The presentation of the palmar variant in an elderly patient is a rarity.
Granuloma annulare is a benign inflammatory skin condition that most commonly affects acral regions, such as the dorsa of hands and feet, the forearms and the legs, but usually spares the palmar and plantar regions. It occurs primarily in young people under 30 years of age and predominantly women.1 We report a case of an elderly patient that presented with a rare clinical variant, granuloma annulare of palmar involvement, that required clinical and histopathological correlation.
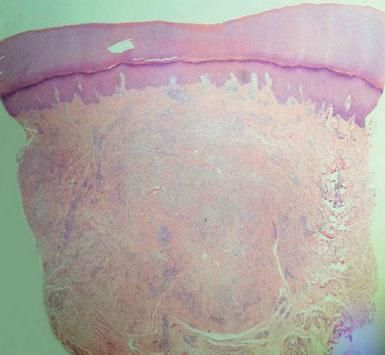
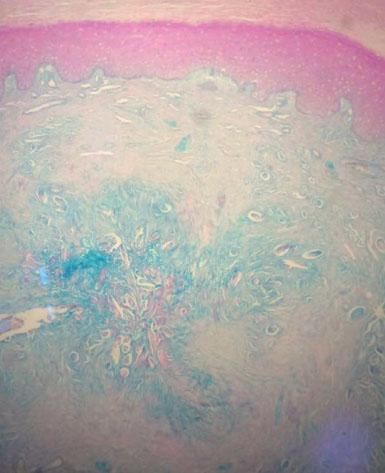
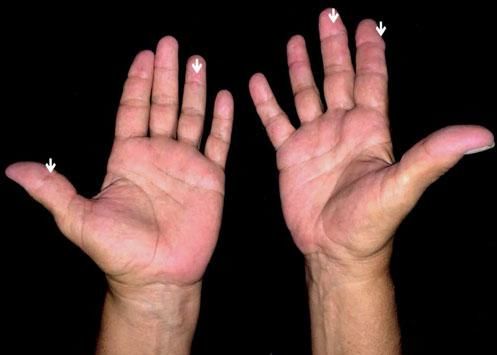
Case ReportA 63-year-old female patient, with rheumatoid arthritis for the last two years, was using methotrexate (12.5mg/week) and leflunomide (20mg/week) and was in clinical remission. Two months prior to the appointment, the patient noticed painless, normochromic, nonpruritic papules located bilaterally on the sides of the fingers and on the palmar region. She denied systemic and joint symptoms. Examination found hardened normochromic papules, approximately 0.5cm to 1 cm in diameter, located bilaterally on the sides of the fingers and on the palms. There was no involvement of the dorsa of the hands nor signs of joint involvement. In the histopathological examination, the histological sections showed hyperkeratosis and acanthosis. Palisading histiocytes and macrophages were present throughout the dermis, surrounding fragments of collagen fiber bundles in its interior. Colloidal iron staining revealed mucin in the center of the palisade. This confirmed the hypothesis of palmar granuloma annulare, for which the patient was prescribed topical clobetasol propionate 0.05% under occlusion, once daily for 30 consecutive days (Figures 1 to 4).
Granuloma annulare was observed for the first time by Fox in 1895.2 Despite being a relatively common and benign inflammatory condition, it remains an enigma in terms of etiology, associated systemic diseases and treatment.3 The physiopathogenic mechanisms are poorly understood. It is believed that an immune-mediated reaction, namely a type IV delayed hypersensitivity response, occurs in relation to precipitating factors such as trauma, insect bite, viral infection, sun exposure or use of medications.4 In the case in question, a precipitating factor justifying the development of the cutaneous lesions was not identified. Granuloma annulare occurs mainly in young women under 30 years of age, but can occur in all age groups, without ethnic or racial propensities. The acral regions are the most affected, particularly the dorsa of the hands and the forearms, but lesions can also occur on the feet, legs and torso. Generally, the palmar and plantar regions are spared. Wide clinical variability exists, comprising papular, nodular, plaque, subcutaneous, perforating and generalized forms. Frequently, the lesions are annular, symmetric, and asymptomatic and vary from normochromic and erythematous to violaceous. Depending on the clinical variant, granuloma annulare can be difficult to diagnose.1,3 In the case in question, the patient was outside of the most common age group for the appearance of granuloma annular and yet presented palmar involvement. The classic histopathological findings of granuloma annulare include hyperkeratosis, presence of fragmented collagen with necrobiotic foci, palisaded interstitial lymphohistiocytic infiltrate, and increased mucin deposition, all of which were found in this case.4,5 Granuloma annular of the palms seems to be rare, but must be included in the differential diagnosis of palmar papules and plaques. A careful assessment is recommended for the exclusion of diagnoses that can resemble granuloma annulare, such as interstitial granulomatous dermatitis, neutrophilic granulomatous disease, rheumatoid nodule, Churg-Strauss disease, erythema elevatum diutinum, acral Sweet’s syndrome, dermatofibroma and drug-induced granulomatous eruptions.4 There is a condition called “nodosity accelerated by the use of methotrexate”, which is an adverse reaction to the use of methotrexate, characterized by the accelerated appearance of small, hardened nodules mainly on the fingers. This condition occurs at a prevalence of 8% to 11% of methotrexate users, mostly in rheumatoid arthritis patients who use the medication. Relative to rheumatoid nodules, the methotrexate-induced nodules are smaller and develop more rapidly in tissues that are soft and far from the joints. They can appear on the forearms and elbows and even in internal organs.6,7 In nodosity accelerated by methotrexate, the histological alterations resemble those found in the rheumatoid nodule. In the patient in question, this hypothesis was rejected based on the histopathology. Thus, the diagnosis of granuloma annulare was confirmed by the clinical and histopathological correlation. The few cases of granuloma annulare described in the literature indicate that it occurs most often in patients under the age of 30. We report a new case of a clinically uncommon presentation in an elderly patient. The therapeutic approach is broad and still requires clinical studies with consistent data. Our patient was prescribed topical clobetasol propionate 0.05% under occlusion, once daily for 30 consecutive days, with satisfactory response.4
Financial support: None.
Conflict of interest: None.