Dear editors,
Here we report a case of Fox-Fordyce disease (FFD). The patient is a 26-year-old woman with complaints of skin lesions in the bilateral axillae and vulva areas for 7 years. Seven years ago, some pruritic skin-colored papules began to appear in the bilateral axillae and vulva areas. The number of skin lesions increased gradually from then on. The lesions were intermittently pruritic, particularly in higher temperature during mental strain. She was well before, and both medical history and family history of the patient were unremarkable. The physical examination revealed numerous round (2-4mm), skin-colored to reddish papules (Figure 1). The hair in both axillae were sparse, and there was hair growth throughout from the center of some papules. The surrounding skin was normal.
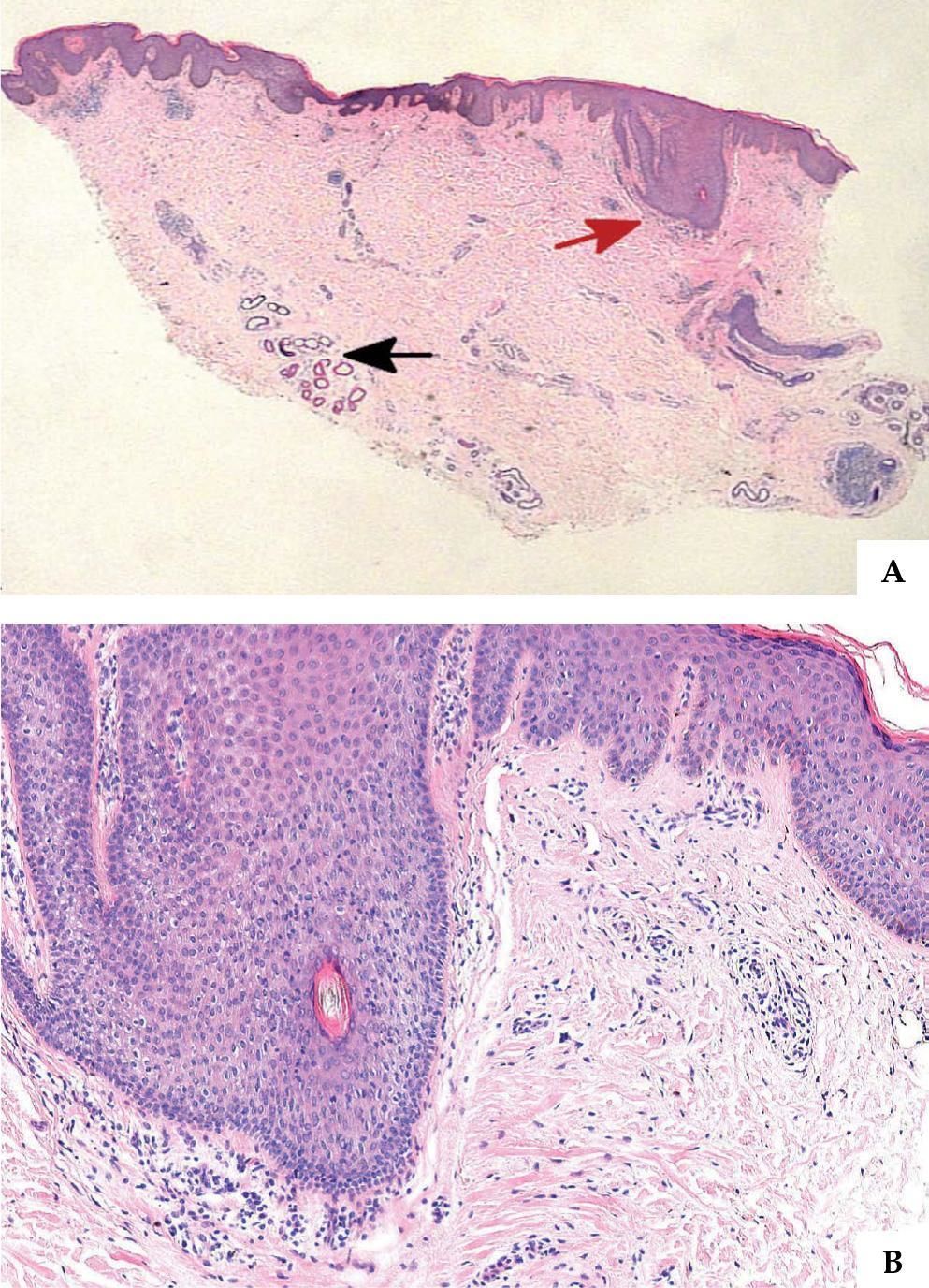
Incision biopsy of the armpit showed hyperkeratosis and irregular acanthosis. The spongiosis involved the epidermis as well as the hair follicle. The dermis had a mild, superficial, perivascular and perifollicular lymphocytic infiltrate as well as some histocytes and eosinophils. We could find some dilated sweat gland ducts in the deep dermis (Figure 2). We diagnosed the patient with FFD based on the typical clinical parameters and histopathological characteristics.
A - Hematoxylin & eosin, X10. Hyperkeratosis and irregular acanthosis, some mononuclear cells (indicated by red arrow) forming an infiltrate around hair follicle; dilation of sweat gland ducts (indicated by black arrow) in the lower-mid dermis. B - Hematoxylin-eosin, X100. Follicular spongiosis, some lymphocytes and a few histocytes and eosinophils
Fox–Fordyce disease was first described in 1902 by George Henry Fox and John Addison Fordyce.1 It is a rare inflammatory disease of the apocrine sweat glands characterized by severely pruritic follicular papules confined to apocrine gland-bearing areas such as the axillae, groins, pubic region, perineum, labia majora, areola mammae, and umbilicus. It is predominantly seen in women. The disease occurs mostly in postpubertal women between 13 and 35 years old. It has rarely been reported before puberty, after menopause, or in men. Itching is aggravated by emotional, physical, or pharmacological stimulations that cause apocrine sweating. The exact etiopathogenesis of the disease remains elusive. Some case reports revealed that laser hair removal therapy may cause the disease.2
Histopathological examination is characterized by keratin plugging, resulting in dilatation and rupture of the apocrine duct. Rupture results in spongiosis of the follicular wall. Perifollicular and perivascular inflammatory infiltrate is also observed. Perifollicular foamy cells could be the histopathologic hallmark of this disease.
There is no definitive treatment for Fox-Fordyce disease. However, many different therapeutic modalities have shown variable efficacy in small subsets of patients. Previously, many therapies have been applied to this disease, including topical and intralesional application of corticosteroids, topical or systemic retinoid, clindamycin, benzoyl peroxide, oral contraceptives, isotretinoin, and phototherapy, but the efficacy was unsatisfactory. However, some case reports revealed that topical pimecrolimus and tacrolimus, excision-liposuction and curettage, fractional carbon dioxide laser, pulsed dye laser and so on may be proposed to remove the cutaneous lesions. 3-5 For this patient, we chose the topical treatment with corticosteroids as well as oral antihistamines for 1 month. Although there was no change in lesions, the pruritus improved slightly.
In conclusion, although Fox-Fordyce disease is uncommon, it is not difficult to diagnose based on clinical and histopathologic manifestations. When we encounter similar cases in clinical work, we shall try to search for pathogenesis and effective treatments for the disease.
Financial support: None.
Conflict of interests: None.