Multinucleate cell angiohistiocytoma is a rare idiopathic benign fibrohistiocytic and vascular proliferation usually presenting as multiple asymptomatic papules, red to violaceous in colour, primarily located on the extremities of middle-aged females. This entity is probably underdiagnosed due to the lack of recognition by clinicians and pathologists. We describe a patient with a multinucleate cell angiohistiocytoma of the face, a less frequent localization, in order to increase awareness of this entity and elucidate its clinical, histopathological, and immunohistochemistry features.
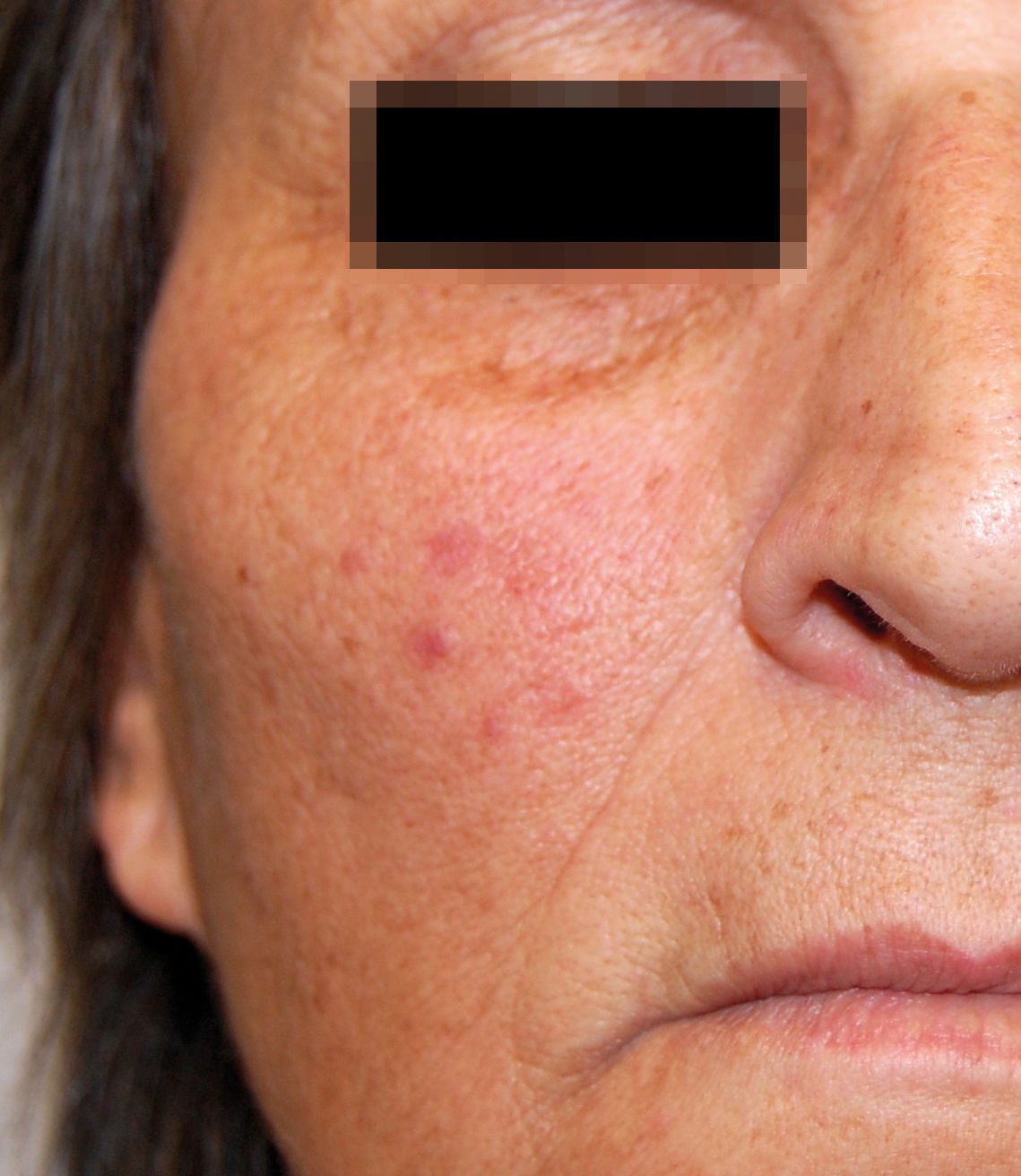
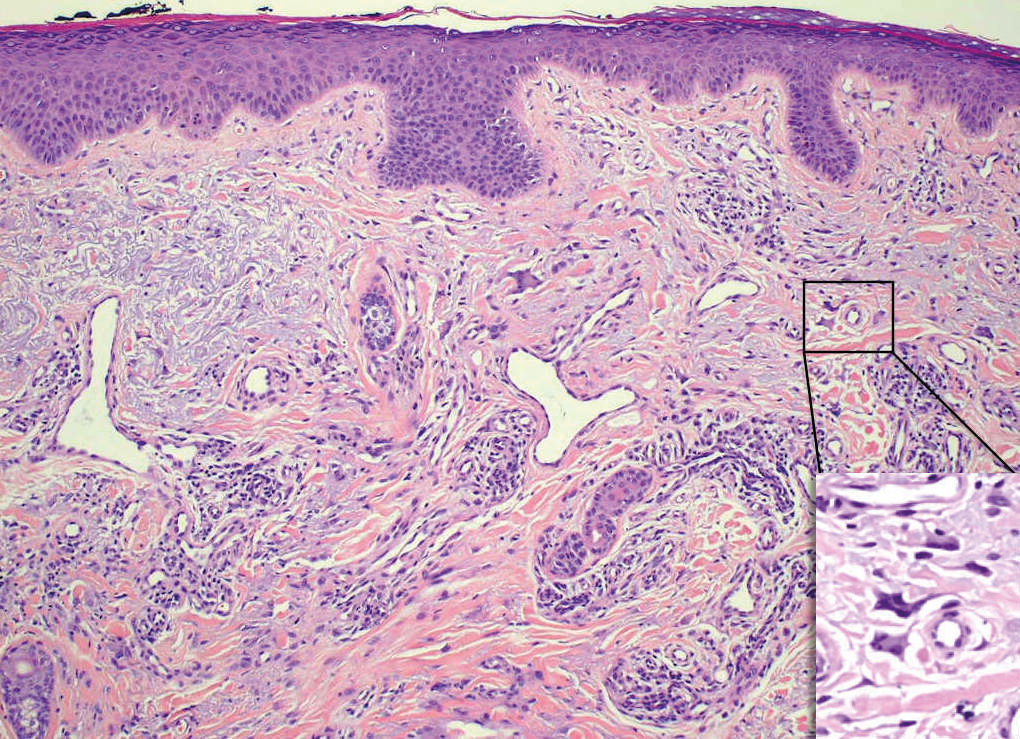
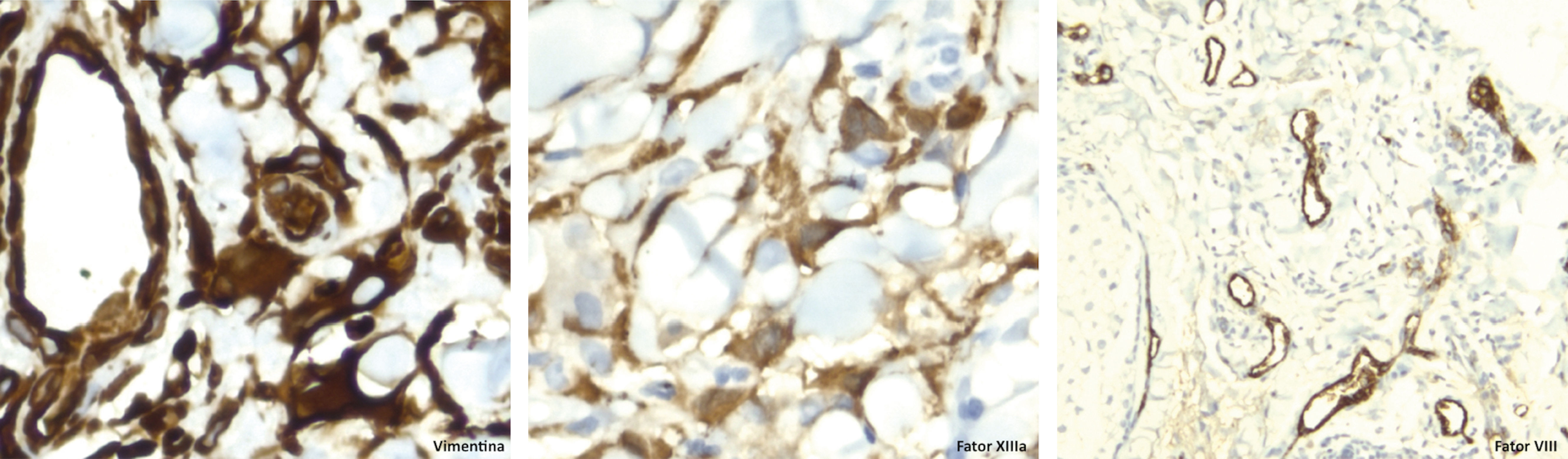
We report a healthy 60-year-old woman who presented with multiple asymptomatic, erythematous lesions scattered over the face, with progressive appearance over the last year. Objective examination revealed erythematous, non-desquamative papules with firm consistency and relatively well-defined borders, measuring 5-10 mm, located in both malar regions (Figures 1 and 2). A biopsy of one of the lesions was performed. Histopathological examination revealed multinucleated cells of varying dimensions in the superficial dermis characterized by angular outlines, mainly showing a ring arrangement in the periphery. Vimentine staining (not CD68) revealed proliferation of small-dilated vessels (FVIII- and vimentin-positive endothelial cells), interstitial infiltrate of dendritic cells (positive for FXIIIa and vimentin), and perivascular lymphohistiocytic infiltrate (Figures 3 and 4). Clinical and histopathological findings favored the diagnosis of multinucleated cell angiohistiocytoma. Given the benign nature of this entity, the patient refused treatment.
Multinucleated cells in the superficial dermis with an angular outline (detailed in lower right corner, Hematoxylin & eosin, X100). Proliferation of small dilated vessels, slight interstitial infiltrate of spindle or dendritic perivascular cells, mostly lymphohistiocytic (Hematoxylin & eosin, X40)
Multinucleated cell angiohistiocytoma (MCA), first described in 1985 by Smith and Wilson-Jones, is a rare benign vascular and fibrohistiocytic proliferation, which occurs most often in women between 40 and 70 years of age.1-5 It usually manifests itself as asymptomatic grouped papules, red-brownish to violaceous in color, of indolent appearance and progressive growth, usually located on the dorsum of the hands or on the legs.2-5
The pathogenesis of MCA remains unknown, but the current evidence points to a reactive process.3-6 It appears to be an underdiagnosed entity with less than 150 cases reported in the literature.6
Histopathologically, MCA is characterized by vascular hyperplasia associated with an increased number of factor XIIIa-positive fibrohistiocytic interstitial cells and multinucleated cells with angular contours located in the dermis.3,7 Although not pathognomonic of MCA, the presence of multinucleated giant cells is the most specific histopathological finding (3-10 hyperchromatic nuclei and basophilic cytoplasm).7,8 In a immunohistochemical study, multinucleated cells are stained by vimentin and, alternatively, by CD68. Mononuclear dendritic cells are positive for vimentin, factor XIIIa, MAC387, and lysozyme. Endothelial cells, in turn, are positive for vimentin, CD31, CD34, and factor VIII.3,4,9
In the present case, the differential diagnosis with fibrous papule of the face/angiofibroma is particularly prominent. Clinically, these diagnoses are less likely, since the fibrous papules appear as isolated skin-color lesions and angiofibromas, ususally associated with other syndromes. These lesions are exophytic with harder consistency and well-defined limits. Histologically, although MCA, angiofibroma, and fibrous papule exhibit common characteristics of dilated capillaries in the dermis, in the latter two, the collagen bundles show a vertical or perifollicular orientation (unlike the horizontal orientation observed in MCA) with only a few multinucleated cells.3,7,10
Although MCA follows a slowly progressive course, rare cases of spontaneous regression are described in the literature, for which a conservative approach is recommended.3-5
MCA is a distinct clinical-pathological entity that should be considered in the differential diagnosis of other vascular and fibrohistiocytic proliferations. The present case revealed a less frequent location of this pathology that may impose some difficulties in its diagnosis.
Financial support: None.
Conflict of interest: None.