Psoriasis has been associated with various autoimmune diseases, however, its relation to bullous diseases is infrequent. Of these, bullous pemphigoid appears as the main associated entity, even though both conditions differ considerably in demographic and clinical aspects. We report the case of a 42-year-old female patient, with long-standing psoriasis who consulted due to the exacerbation of psoriatic plaques associated with generalized bullous lesions on the skin and oral mucosa, with one-week duration. With clinical signs and histopathological findings compatible with bullous pemphigoid associated with psoriasis, we decided to treat her with methotrexate 10mg a week. The patient had an excellent response after two months of treatment.
Psoriasis (PSO) is a chronic inflammatory disease with a worldwide prevalence of 2 to 4%.1 It has been associated with various autoimmune diseases, such as inflammatory bowel disease, celiac disease, among others, being infrequent its association with bullous diseases.2 Bullous pemphigoid (BP) is the most frequent blistering dermatosis and the most associated with PSO, with about 50 cases reported in the literature since 1929.3,4 The pathogenic mechanisms of this association remain unknown, considering that both conditions have well-known demographic, clinical, histopathological and therapeutic differences.
We present the case of a woman with long-standing PSO associated with BP of recent onset.
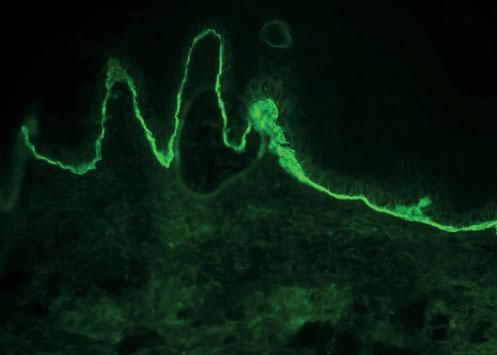
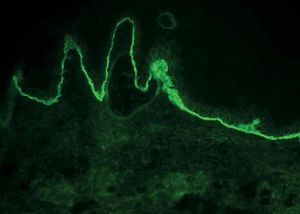
Case ReportA 42-year-old female patient had a history of PSO since 17 years of age, without other co-morbidities, under irregular treatment with high-potency topical corticosteroids. She consulted due to one-week course of generalized bullous lesions on previously healthy skin and oral mucosa, associated with extension of psoriatic plaques on the trunk and extremities, without triggering factors like phototherapy, drugs or sunlight exposure. Physical examination revealed tense and confluent blisters on the back of hands, palms and soles with serous content, erosions on the oral mucosa and extensive desquamative erythematous plaques on the forearms, thighs, legs and lower back (Figure 1). A skin biopsy was performed (3 samples), which revealed psoriasiform dermatitis with parakeratosis, intracorneal pustule, hypogranulosis, dilated dermal capillaries with predominantly polymorphonuclear moderate superficial inflammatory infiltrate with the presence of a subepidermal blister with neutrophils and eosinophils in one of the samples. In direct immunofluorescence, IgG and C3 deposits with linear pattern were found in the dermoepidermal junction, compatible with BP (Figure 2). Indirect immunofluorescence was not made, due to unavailability.
Treatment was started with methotrexate 10mg weekly, associated with folic acid 5mg weekly and medium-potency topical corticosteroids.
After 2 months of treatment, the patient showed marked improvement, with remission of the bullous lesions and scarce erythematous desquamative lesions on the dorsal region, maintaining no bullous lesions or psoriatic plaques in the fourth month of follow-up (Figure 3).
DiscussionThe association of PSO and BP is infrequent, with few reports in the literature to allow the estimation of the real frequency in which this association occurs. It is estimated to be around 2.1% and 5.3% in Taiwanese and Chinese populations, respectively.5,6 In Latin America, there are only reports of isolated cases. In the largest case series that included 145 patients with bullous diseases and PSO, it was found that 63% of these corresponded to BP, being more frequent in men (82.1%) with ages between 50 to 80 years. Blistering lesions are described in both healthy skin and skin with psoriatic plaques. In most cases, the PSO precedes BP in several years, with an average interval of 15 to 25 years.3,6,7 Regarding the proposed pathogenic mechanisms, it is described that for unknown reasons there would be an alteration of the immune response mediated by T lymphocytes, in which antibodies directed against stratum corneum and granulosum structures present in psoriasis could attack the basement membrane. On the other hand, electron microscopy has shown damage to the basement membrane in patients with PSO, generating alterations in antigenicity, with subsequent exposure and development of autoantibodies.8 Anti-p200 pemphigoid or an-ti-laminin-gamma-1 pemphigoid, described just over 20 years ago, with great clinical and histopathological similarity to BP, emerges as a bullous disease of frequent association with PSO, mainly in the Japanese population, which suggests that a high proportion of the cases of pemphigoid and PSO would correspond to this entity.9 The lack of availability of immunoassay techniques for the detection of anti-p200 could lead to an overestimation of the coexistence between PSO and BP. One of the greatest challenges of this association is management, with methotrexate being the most used therapeutic option with good response, as presented in this case. As second line, have been reported systemic corticosteroids, cyclosporine, azathioprine, dapsone and erythromycin with etretinate.4,10 The present case is reported given the uncommon association between both conditions, especially in the Latin population, in addition to highlighting the rapid and favorable response of both conditions to methotrexate.