We report the case of a male 22-month-old child, with atypical presentation of Gianotti-Crosti syndrome after infection with Epstein-Barr virus.
Gianotti-Crosti syndrome, also known as papular acrodermatitis of childhood, is a self-limited condition that usually affects children between 2 and 6 years of age after a viral infection or vaccination.1 We report the case of a 22-month old child with vesiculobullous Gianotti-Crosti syndrome after Epstein-Barr virus infection.
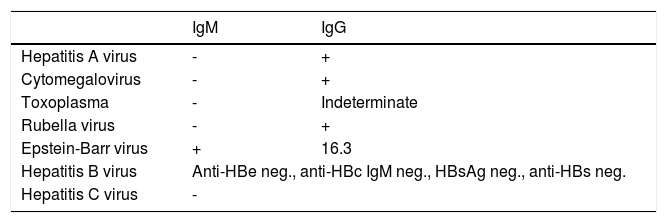
Case ReportA 22-month-old male patient, had a history of “stomatitis” in the past 15 days. He was medicated with an oral ointment containing hydrocortisone, neomycin, troxerutin, ascorbic acid, benzocaine and dipyrone. Eight days later, he developed pruritic papules on the elbows, forearms, legs, back and face (Figures 1 to 4). He was given hydroxyzine, loratadine and amoxycillin, besides moisturizers and liquid talcum, with no improvement. He had a past history of rhinitis and asthma and was born at term, after a cesarean and no complications. There was no recent history of vaccination. On dermatological examination, blisters and vesicles of different sizes were seen, isolated and grouped, localized mainly on the face and upper and lower limbs, with a few on the trunk. Hydroxyzine was prescribed (1mg/kg/day) and serologies were requested, which revealed recent Epstein-Barr virus infection (Chart 1). He returned 20 days later with complete and spontaneous resolution of the clinical picture, with no scarring.
DiscussionGianotti-Crosti syndrome was described in 1955 as a sudden-onset dermatitis, with multiple erythematous, non-pruritic papules on the limbs, face and neck of children, with limited duration. This condition, later known as papular acrodermatitis of childhood, was associated a few years later to the hepatitis B surface antigen (HBsAg).2
Already in 1964, Gianotti and Crosti reported that sometimes in infancy it was possible to see other papular or papulovesicular acral, polymorphic, frequently pruritic eruptions, HBsAg negative, that could have multiple etiologies and were thus clinically distinct from papular acrodermatitis of childhood. The lesions of this eruption, known as “papulovesicular acral syndrome”, were categorized into 3 types:
Type A — symmetrical, small, round, pink, non-coalescing lesions;
Type B — frequently coalescing lesions, forming large edematous and pruritic lesions on the limbs; and
Type C — symmetrical, erythematous, frequently purpuric and prominent lesions, usually non-pruritic, that tended to last for 2 months or more.2
In the 1970s, some authors classified the cases related to hepatitis B as “Gianotti disease”, with multiple erythematous, monomorphic and disseminated papules; the cases with normal liver function were classified as “Gianotti syndrome” and differently, had polymorphic lesions (erythematous or hemorrhagic papules, vesicles and molluscum contagiosum-like lesions) unevenly distributed.3 Posteriorly, Caputo et al.4 conducted a study to verify if such variants could be clinically distinguishable by dermatologists and reached the conclusion that this distinction was not possible. He raised the hypothesis that the papular or papulovesicular variants were influenced by other factors such as age, health status and vaccination status, and recommended the term “Gianotti-Crosti syndrome” for both variants, denomination that is used until today.4
Gianotti-Crosti syndrome has a worldwide distribution; however, since it is frequently underdiagnosed, there are no data on its real incidence, especially the vesicular cases, that are limited to only a few case reports in the literature.1 Taïeb et al.5 conducted a retrospective study in 1986 assessing files of 26 patients with Gianotti-Crosti syndrome who were seen at their service in France during 5 years, and found 12 papulovesicular cases (46%).5
Linke et al.6 described the case of a 7-year-old girl who presented with papules and pruritic plaques on the limbs and tense bullae only on the hands and feet. Autoimmune bullous diseases were ruled out with the histopathology; however, no serology was performed. The lesions had complete resolution after 1 week with oral corticosteroids and antihistamine, without recurrence.6 Recently, Stojkovic-Filipovic et al.7 described a case of papulovesicular Gianotti-Crosti syndrome in a 20-year-old man who had lesions on the face, buttocks, extensor aspects of the limbs, besides knees, elbows and palms. In this case, serologic tests were positive for parvovirus B19 and Epstein-Barr virus. The lesions had complete resolution after 3 weeks, with the use of oral and topical corticosteroid, besides antihistamines.7 Till present, we have not found in the literature vesiculobullous cases such as the one presented in this article.
After vaccination against hepatitis B, Epstein-Barr virus became the main etiologic agent of Gianotti-Crosti syndrome.8 This virus has a high prevalence in the developed countries and can lead to asymptomatic or oligosymptomatic infection or manifest as infectious mononucleosis, Gianotti-Crosti syndrome, erythema multiforme or acute genital ulcers. After the primary infection, the virus infects B lymphocytes in the oropharyngeal mucosa, becoming immortalized; this way, the infected individuals remain as asymptomatic carriers.9 Other viruses were reported in association with the syndrome, such as hepatitis A virus, cytomegalovirus, herpes-virus 6, Coxsackie virus, rotavirus, parvovirus B19, human respiratory syncytial virus, parainfluenza virus, paramyxovirus and poxvirus. There are also case reports associating the syndrome to bacterial infections, such as the ones caused by beta-hemolytic streptococcus, Mycoplasma pneumoniae and Bartonella henselae. Besides, there are some reports that the syndrome occurred after immunization against polio, influenza, hepatitis B and DPT vaccine (diphtheria, tetanus and pertussis).1
Since it is a self-limited and pauci-symptomatic condition, the management is usually expectant. Medium-potency topical or oral corticosteroids can be used in extensive cases. Antihistamines can be used in cases with associated pruritus.1
Financial support: None.
Conflict of interest: None.