Primary cutaneous amyloidosis is limited to the skin without involving any other tissue. Nodular amyloidosis is rare, and atrophic nodular cutaneous amyloidosis is even rarer. We describe the fourth case of atrophic nodular cutaneous amyloidosis by searching PubMed databases. A 52-year-old female presented to our hospital with a 2-year history of orange papules and nodules without subjective symptom on her right abdomen. Review of systems was negative. Atrophic nodular amyloidosis may progress to primary systemic disease in up to 7% of cases. Because our patient had no systemic involvement, she was diagnosed with atrophic nodular cutaneous amyloidosis based on characteristic symptoms and histopathologic examination. Routine follow-up for this patient is necessary to detect any potential disease progression.
Amyloidosis is a group of disorders that are characterized by tissue deposition of amyloid. Primary cutaneous amyloidosis is limited to the skin without involving any other tissue. It has three major forms: macular amyloidosis, lichen amyloidosis, and, most rarely, nodular amyloidosis (NA). Atrophic nodular cutaneous amyloidosis (ANCA) in NA is even rarer.1-4 Here, we report a case of a 52-year-old woman with nodular atrophic cutaneous amyloidosis on her right abdomen.
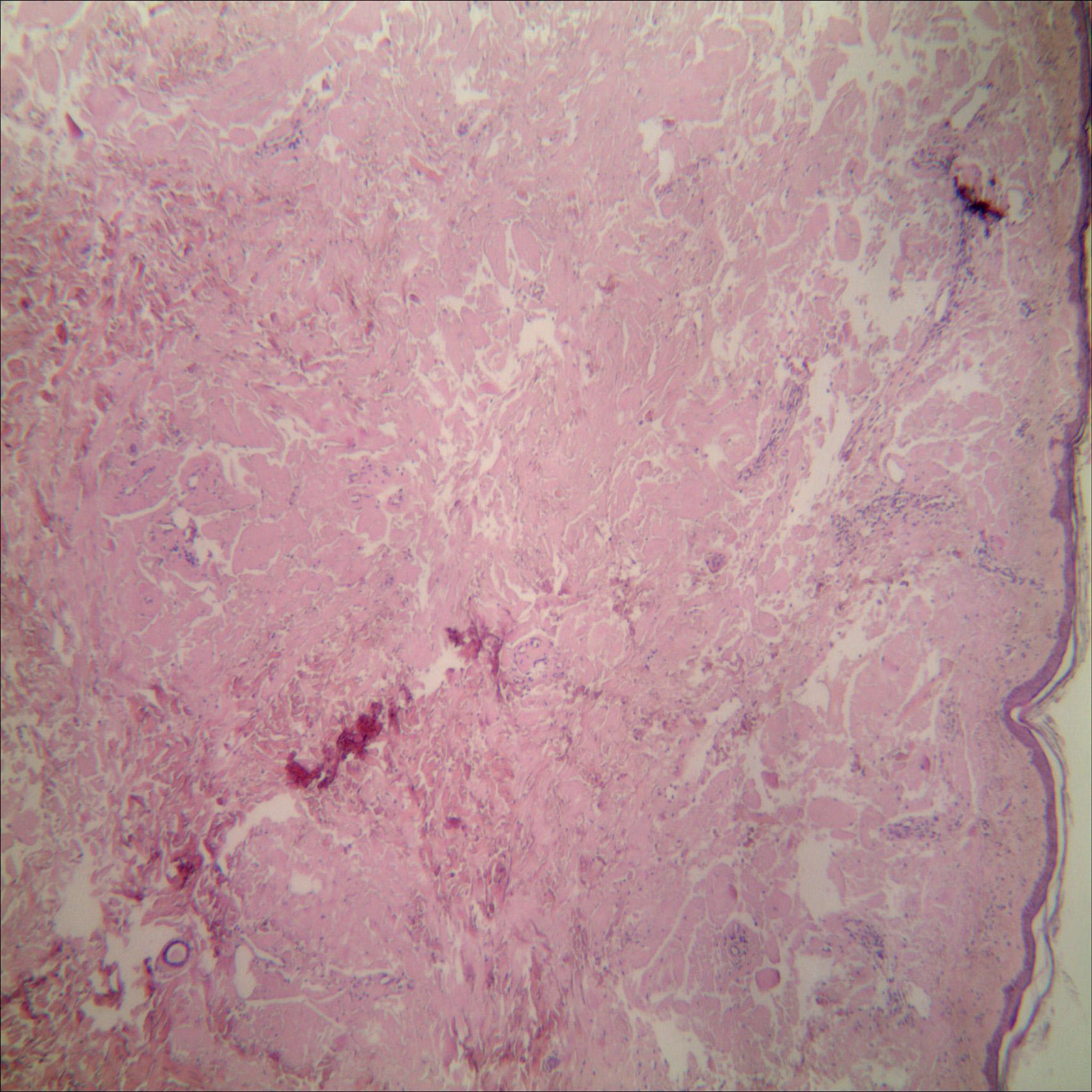
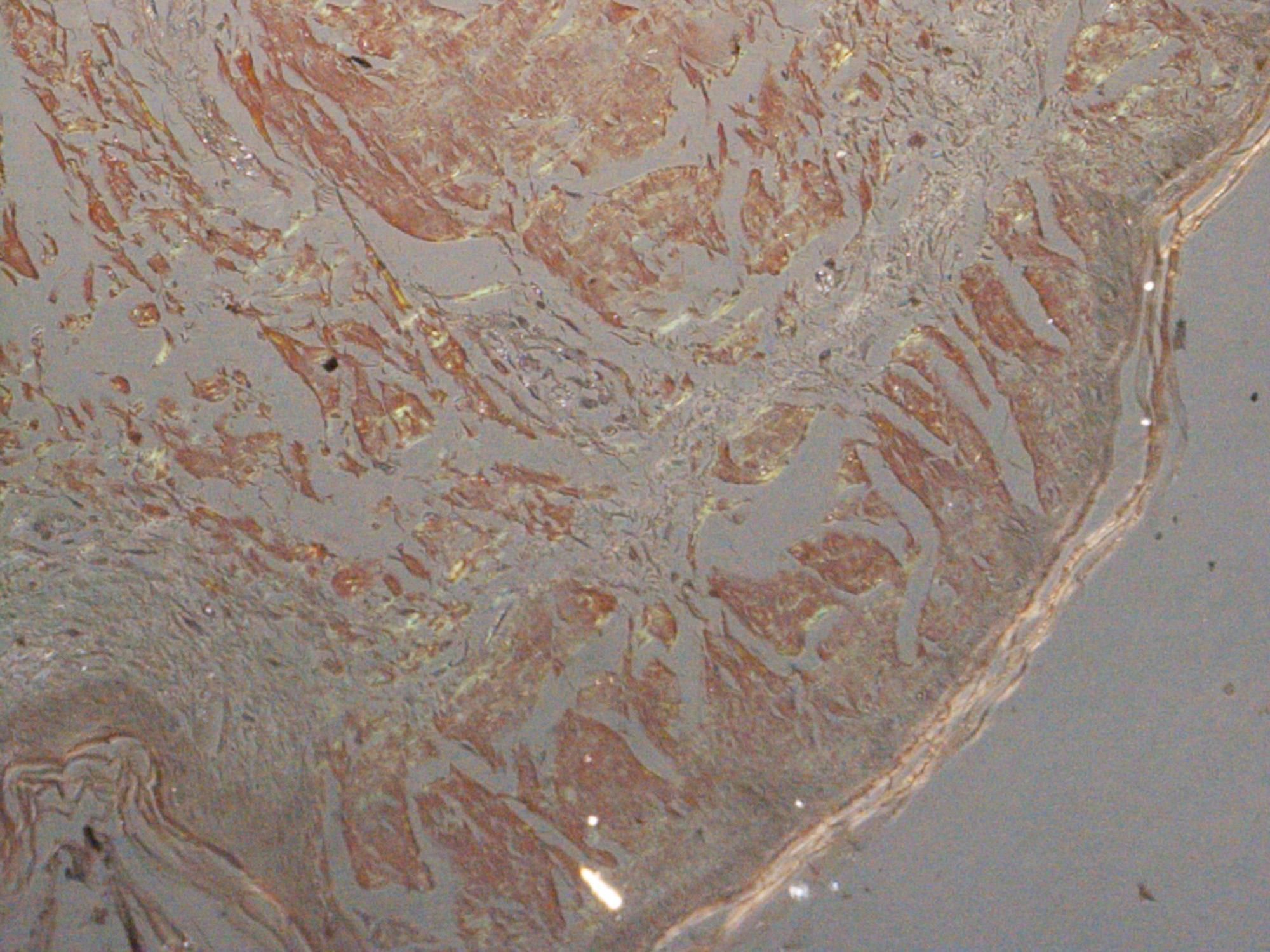
Case ReportA 52-year-old woman was followed in our dermatology clinic with a 2-year history of orange papules and nodules without subjective symptoms on her right abdomen. She recalled having had a few papules and nodules initially, that gradually increased thereafter. Before visiting our dermatology clinic, she had presented to another dermatology clinic with a diagnosis of cutaneous amyloidosis, but received no treatment. Review of systems was negative. She had a history of diabetes, liver steatosis and gallstone surgery. Physical examination showed atrophic, flaccid, soft, scattered orange papules and nodules of different sizes on her right abdomen (Figure 1A and 1B). The following tests were performed, with normal results: blood and urine routine, liver and kidney function, urine protein electrophoresis, chest X-ray, abdominal ultrasound and so on. Skin biopsy revealed atrophy of the epidermis; collections of reddish amyloid protein deposited in the dermis, subcutaneous tissue, and around the blood vessels (Figure 2A). The material stained with Congo red, with an apple-green birefringence on polarized light. (Figure 2B).
The patient was diagnosed with nodular atrophic cutaneous amyloidosis. Surgical excision was performed, and now she is undergoing follow-up.
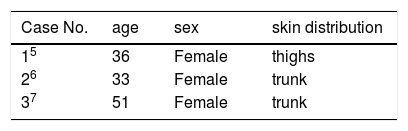
DiscussionPrimary cutaneous amyloidosis is limited to the skin, and is characterized by the deposition of amyloid without involving any other tissue. Nodular amyloidosis is rare, and atrophic nodular cutaneous amyloidosis in NA is rarer1. By searching PubMed databases, there are only 3 articles that reported nodular atrophic cutaneous amyloidosis (Table 1).5-7
In rare cases of nodular amyloidosis, the amyloid is composed of aggregated kappa and lambda light chains, which can occasionally indicate a serious underlying systemic disease, with an estimated 7% of patients progressing to systemic amyloidosis.1,2,5 Therefore, patients with atrophic nodular cutaneous amyloidosis should be regularly evaluated for progression.2 Our patient has no systemic disease, according to multidisciplinary examination at present.
The diagnosis of this disease requires the combination of clinical manifestation with histopathological examination with a specific stain. Atrophic nodular cutaneous amyloidosis usually presents one or more asymptomatic brown or yellow nodules, with a surface that appears atrophic, and may be thin and wrinkled with whitish-yellow color.8 Histopathologic features include amyloid deposits in the dermis, subcutaneous fat, and blood-vessel walls. A perivascular infiltrate of plasma cells may be observed. In addition, Congo red, periodic acid-Schiff, and thioflavin T stains are positive.1,9 Our patient meets the diagnostic criteria of atrophic nodular cutaneous amyloidosis, however, one should differentiate from colloid milium, systemic amyloidosis and nodular or swelling amyloidosis.10 Clinical manifestation is the appearance of atrophic, flaccid and soft lesions on photoprotected skin, and the histopathology shows reddish amyloid protein deposited in the dermis, subcutaneous tissue, and around the blood vessels, which exclude colloid milium. Systems and laboratory examination are all negative and systemic amyloidosis can be temporarily dismissed. Although the histopathology will be similar to nodular or swelling amyloidosis, there are differences in the clinical manifestations.
We are presenting our case with the purpose of highlighting this rare condition, which will encourage clinicians to biopsy more cases of clinically suspected atrophic nodular cutaneous amyloidosis and improve our understanding of this rare entity.
Financial support: None.
Conflict of interest: None.