Dear Editor,
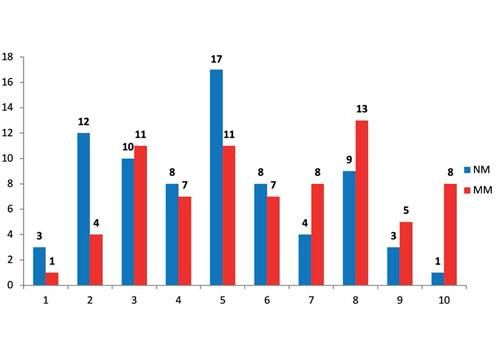
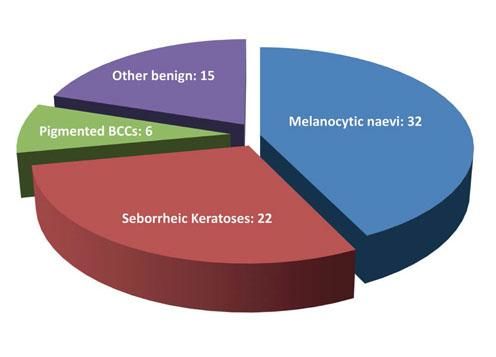
Worldwide the incidence of melanoma is increasing faster than of any other cancer. Early detection is critical in reducing mortality and morbidity, and therefore general practitioners (GPs) need to be able to screen effectively between benign and suspicious lesions.1,2 Interventions that improve the accuracy of secondary care triaging may be used to prioritize patients with malignant lesions and help combat the hindrances of long waiting times. GPs referring suspected melanomas to our department were asked to use a pro forma with an integrated 10-point Likert scoring tool and grade the likelihood of lesions being melanomas (1 least likely, 10 most likely). Based on results from a previous pilot study in our department, all patients referred with a score ≥4 were triaged to an urgent appointment and those with a score of ≤3 to a soon appointment. Our aim was to assess the usefulness of this proforma in discriminating between malignant melanomas (MM) and other pigmented lesions (NM). We retrospectively assessed the clinical records of all (n=75) patients diagnosed with MM in 2016 who were referred using the above proforma and matched them with 75 consecutive NM patients. Two hundred patients with primary MM were diagnosed in our department in 2016, 75 (37.5%) of which with the above proforma. In the MM group 38 patients were male and 37 female, with a mean age of 59.8 years. In the NM group, 29 patients were male and 46 female, with a mean age of 48.4 years. Both groups had overlapping scores ranging from 1 – 10 (Figure 1). Median and mean scores in the MM group were 6 and 6.02. The NM group had a median score of 5, and mean of 4.78. There was no statistical difference between the two groups (p=0.97). Forty-one MMs had Breslow thickness <1mm, 26 between 1-4mm, and eight >4mm. Of the 75 NM lesions, 32 represented benign naevi, 22 seborrheic keratoses, six were pigmented basal cell carcinomas, and 15 represented a mixture of other benign lesions (Figure 2). Using this proforma and based on a score of 4 as the cut-off, 78% of all NM lesions and only 80% of MMs would have been given an urgent appointment. Furthermore, adjusting the cut-off value would not improve the situation meaningfully. Based on earlier studies, 60-95% of GP referrals of lesions to UK dermatologists were benign, and GPs could only recognize 66.7% of all skin malignancies.3,4 Taking the above into consideration, any triaging tool that is based on GP scoring is likely to be unsuccessful. Interestingly, recent developments in the field of artificial intelligence have shown promising results on the ability of computer programs to accurately recognize and classify cutaneous tumours.5 Even though further research is required for such tools to be widely available, their potential for use on mobile devices may be key in augmenting the clinical decision-making of GPs and transforming the referral process.5 Until such programs become available it is hard to quantify the effort, resources, and time required to train GPs and the success of such an undertaking. We therefore argue that all suspicious pigmented lesions referred to secondary care be triaged as urgent. ❑
Financial support: None.
Conflict of interest: None.