Background: Skin cancer is common in Brazil and is related to sun exposure, among other risk factors. There are no data on the incidence of malignant skin neoplasm in rural workers in western Paraná.
Objective: To analyze the incidence and profile of rural workers who were diagnosed with skin cancer at a reference service in Cascavel, western Paraná, in the last five years (2011-2016).
Methods: This retrospective cross-sectional study was carried out through a review of the anatomopathological reports of rural workers diagnosed with skin cancer at Cascavel Oncology Center (CEONC), in Cascavel. The following variables were collected: year of diagnosis, age, gender, injury location and histological subtype.
Results: A total of 681 cases of malignant epithelial neoplasia were identified, with a higher frequency in the 61-70 age group. Data analysis showed an increase of about 210% in the occurrence of skin cancers in the last 5 years. The cephalic region was the most affected, and the most common histological subtype was nodular basal cell carcinoma. There was no association between gender and location.
Study Limitations: This is a retrospective study and analysis of a secondary data bank.
Conclusion: This study is a regional estimation of the incidence of cutaneous neoplasms and provides evidence of a considerable increase in the number of diagnoses in rural workers from western Paraná, Brazil. Moreover, it is possible to conclude that the sample group studied is at risk of developing skin cancer.
The incidence of skin cancer is increasing exponentially around the world. In Brazil, it corresponds to 30% of all malignant tumors recorded.1 The estimate for the USA is that one in every five Americans will develop skin cancer during their lifetime, with around 5.4 million basal cell carcinomas (BCC) and spinocellular carcinomas (SCC) being diagnosed in 2012 alone.2,3 Under the same lens, the estimated number of new cases of non-melanoma skin cancer in Brazil in 2016 was 175,760; the number of new cases of the melanoma subtype was 5,670.1,4 These values correspond to an estimated risk of 88 new cases of malignant skin neoplasm for every 100 thousand inhabitants/year, according to a calculation based on population data from IBGE.5
Among skin tumors, non-melanoma skin cancer has the highest incidence in the world population, but has a low mortality and a high cure rate when detected early.6 Conversely, according to national epidemiological data, melanoma skin cancer is estimated to represent only 3% of malignant neoplasms, while severely affecting quality of life and often leading to metastases and death.1,7
Brazil’s South region presents a skin cancer incidence above the national rate, with Paraná having the lowest concentration rate among the southern states. The rates among men in Paraná is 5.39 cases per 100 thousand inhabitants for melanoma cancer, and 107.82 per 100 thousand inhabitants for non-melanoma cancer; the rates among women in Paraná is 5.59 cases per 100 thousand inhabitants for melanoma, and 83.27 per 100 thousand inhabitants for non-melanoma cancer.8 Cutaneous neoplasms are a public health problem, and the challenge of combating these diseases requires knowledge of the disease incidence and their variations in the different regions of the country.9
A combination of two factors may explain the elevated incidence: the European ancestry of most of the population, which is predisposed to the occurrence of this neoplasm due phenotypic characteristics such as blue eyes, light hair, and skin of phototypes I and II (according to the Fitzpatrick classification),10 and sun exposure through increased incidence of ultraviolet radiation (UV), mainly UV-B and UV-A, due to the reduction of the ozone layer over Brazil’s South region.11
Intrinsic risk factors for the development of the various types of skin cancer include a genetic component (e.g., the presence of dysplastic nevi or of a large number of nevi), skin type (related to the capacity to either tan or burn), and race/ethnicity (closely associated with melanoma).12 Compounding the intrinsic factors is excessive exposure to UV rays, which is included in the classification of the physical risks for the development of skin cancer in certain ethnic groups.13 As the main occupational risk factor, it makes outdoor workers more vulnerable to developing skin cancer.14
It is worth noting that, among the physical risk factors, UV radiation is the primary cause of non-melanoma carcinomas; furthermore, the pattern of exposure may originate different subtypes.15 Long-term sun exposure ensures the predominance of spinocellular carcinoma; conversely, basal cell carcinoma is associated with early exposure during one’s life and/or intermittent exposure.16-19
The Brazilian literature contains few studies on the epidemiological data involving malignant skin neoplasms in rural workers. The reason for this is unknown, considering that the number of cases have increase exponentially over the years — probably resulting from a combination between early detection, greater sun exposure and longer life expectancy.20
In addition to the relationship between skin cancer and sun exposure, another factor that favors the development of oncological pathology in the country is the fact that agriculture is one of the main pillars of the Brazilian economy, employing a considerable amount of the work force in the rural regions. In this context, skin cancer presents serious public health challenges, specifically in the area of occupational health. Most work activities in the agricultural sector are performed outdoors, vulnerable to weather variations and to the harmful effects of the sun’s rays — about 90% of these cancers develop in photo-exposed regions of the body.21
In light of the above, this work aims to analyze the incidence of the disease and the profile of the rural-worker patients that were diagnosed with skin cancer at the reference service in the city of Cascavel, in western Paraná, between 2011 and 2016.
MethodsThis study was conducted according to a cross-sectional design, with a search of the data bank of the Cascavel Oncological Center (CEONC). Included in the study were the anatomopathological reports of rural-worker patients diagnosed with skin cancer and treated at the Cascavel Oncological Center (CEONC), in the city of Cascavel (PR), between 2011 and 2016. The city is located in western Paraná. Information on profession, included in the CEONC data bank of electronic medical charts, was based on the declaration of the patients themselves at the time of registration. All positive reports of different histological types of cancer were excluded.
The information extracted from the reports were transferred to a data registration record, created by the authors, using the following variables: year of diagnosis, age, sex, city of origin, location of lesion, and histological subtype.
Regarding histological type, we used the Brazilian Society of Pathology’s proposed classification, dividing into basal cell carcinoma (BCC), spinocellular carcinoma (SCC) and melanoma. The histological subtypes of basal cell carcinoma were divided, based on the same reference, into nodular with or without ulceration, undifferentiated, sclerosing, superficial, adenoid cystic, micronodular, and multicentric. Spinocellular carcinoma was divided into three histological subtypes that varied according to the degree of differentiation, as follows: undifferentiated; associated with Bowen’s disease; and verrucous. Finally, we established a standardization of the melanomas according to the Breslow index.
To evaluate the relationship between age and the area affected by cancer, we created three age categories: category 1, for patients up to 55 years old; category 2, comprising patients from 56 to 65 years of age; and category 3, for patients older than 66 years.
The collected data were entered into the program Microsoft Excel 2010, and the statistical analysis was performed in PAST 3.15 statistical software. Descriptive epidemiology was used to present characteristics of the population under study, with the variables being presented as values of absolute and relative frequency, respectively. For qualitative variables, the proportion of each cancer type in the different categories (age, sex, and affected area) were compared through Pearson’s chi-squared test, and a multinomial logistic regression analysis was performed to control the confounding variables related to affected area. The odds ratio (OR) and respective 95% confidence interval are given, representing the base category for which the lowest risk of the outcome was expected and the significance of the association between the variable in question and the outcome.
The study was approved by the Research Ethics Committee of the Faculdade Assis Gurgacz, under the registration no 61143416.3.0000.5219. Implementation of the research was approved, through signing of the information letter, by Director Reno Paulo Kunz.
ResultsBetween 2011 and 2016, 346 rural-worker patients from western Parana were identified as having anatomopathological reports of malignant skin neoplasms, diagnosed at the Cascavel Oncological Center (CEONC). Among the patients, 681 cases of skin cancer were diagnosed — grouped into basal cell carcinoma (BCC), spinocellular carcinoma (SCC) and melanoma — confirming its recurrent nature in the patients analyzed.
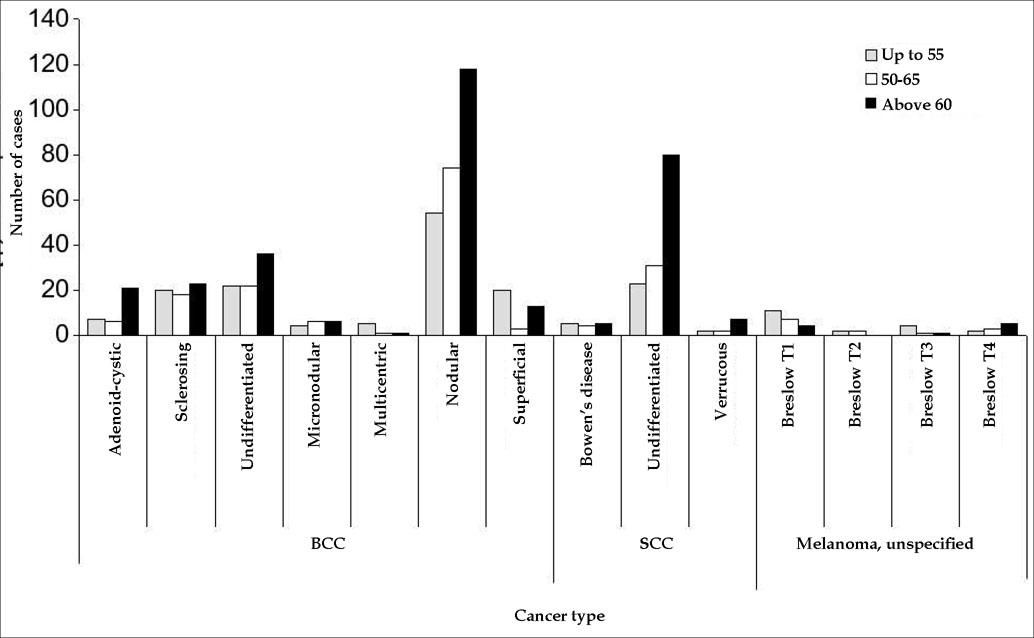
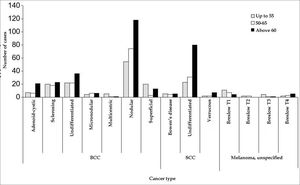
Of the 681 cases, 170 (24.96%) occurred in females. The ages of the patients ranged from 31 to 100 years; the age group with the highest prevalence of epithelial neoplasms was 61-70 years. Graphic 1 shows the patients categorized by age range, according to the frequency of cases. To assess the relationship between age and the site affected by cancer, three age categories were created: category 1, for patients up to 55 years old; category 2, comprising patients from 56 to 65 years of age; and category 3, for patients older than 66 years.
We found the age factor to be statistically significant only for the following types of cancer: multicentric BCC (p=0.02), superficial BCC (p=0.0001), undifferentiated SCC (p=0.002) and T1 melanoma (p=0.01). For the other types of cancer, age was not a risk factor (Graphic 1).
When comparing the individuals by age, the chance of acquiring multicentric BCC is 89% less for people older than 66 years (OR=0.11 (0.01-0.95). For superficial BCC, the chance of acquisition is estimated to be 7.32 times greater for people between 56 and 65 years (OR=7.32 (2.13-25.1); p=0.0001); people older than 66 years are 66% less likely to acquire this type of cancer (OR=0.34 (0.160.70); p=0.0001). For undifferentiated SCC, the chance of acquisition is 2.28 times greater for people older than 66 years (OR=2.28 (1.38-3.79); p=0.002). For T1 melanoma, the risk is 81% lower for individuals older than 66 years (OR=0.19 (0.06-0.62); p=0.01).
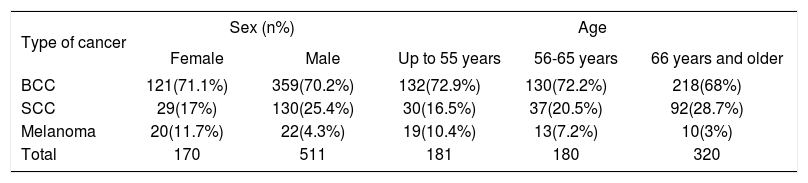
Table 1, which generally analyzes the major types of skin cancer, shows that the incidence of BCC was similar between the sexes. Conversely, SCC had greater involvement among men, while melanoma had a considerably higher incidence among women. In relation to age, both BCC and SCC occurred with greater frequency in patients older than 66 years. In contrast, melanoma presented predominantly in patients up to 55 years of age.
Percentage distribution of cancer types according to sex and age group
| Type of cancer | Sex (n%) | Age | |||
|---|---|---|---|---|---|
| Female | Male | Up to 55 years | 56-65 years | 66 years and older | |
| BCC | 121(71.1%) | 359(70.2%) | 132(72.9%) | 130(72.2%) | 218(68%) |
| SCC | 29(17%) | 130(25.4%) | 30(16.5%) | 37(20.5%) | 92(28.7%) |
| Melanoma | 20(11.7%) | 22(4.3%) | 19(10.4%) | 13(7.2%) | 10(3%) |
| Total | 170 | 511 | 181 | 180 | 320 |
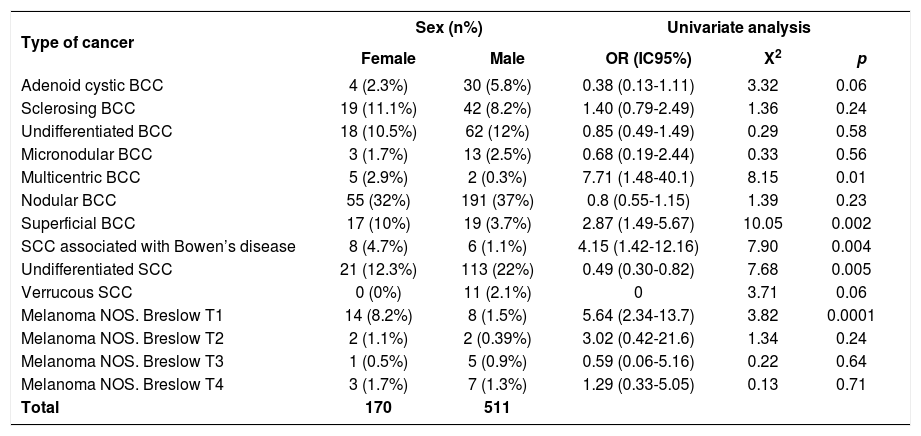
A gender differential in incidence rates was found only for the following types of cancer: multicentric BCC (p=0.01), superficial BCC (p=0.002), SCC associated with Bowen’s disease (0.004), undifferentiated SCC (p=0.005) and TI melanoma (p=0.0001). For the other types of cancer, the sex was not a risk factor, as shown in table 2.
Univariate analysis of skin cancer subtypes relative to gender
| Type of cancer | Sex (n%) | Univariate analysis | |||
|---|---|---|---|---|---|
| Female | Male | OR (IC95%) | X2 | p | |
| Adenoid cystic BCC | 4 (2.3%) | 30 (5.8%) | 0.38 (0.13-1.11) | 3.32 | 0.06 |
| Sclerosing BCC | 19 (11.1%) | 42 (8.2%) | 1.40 (0.79-2.49) | 1.36 | 0.24 |
| Undifferentiated BCC | 18 (10.5%) | 62 (12%) | 0.85 (0.49-1.49) | 0.29 | 0.58 |
| Micronodular BCC | 3 (1.7%) | 13 (2.5%) | 0.68 (0.19-2.44) | 0.33 | 0.56 |
| Multicentric BCC | 5 (2.9%) | 2 (0.3%) | 7.71 (1.48-40.1) | 8.15 | 0.01 |
| Nodular BCC | 55 (32%) | 191 (37%) | 0.8 (0.55-1.15) | 1.39 | 0.23 |
| Superficial BCC | 17 (10%) | 19 (3.7%) | 2.87 (1.49-5.67) | 10.05 | 0.002 |
| SCC associated with Bowen’s disease | 8 (4.7%) | 6 (1.1%) | 4.15 (1.42-12.16) | 7.90 | 0.004 |
| Undifferentiated SCC | 21 (12.3%) | 113 (22%) | 0.49 (0.30-0.82) | 7.68 | 0.005 |
| Verrucous SCC | 0 (0%) | 11 (2.1%) | 0 | 3.71 | 0.06 |
| Melanoma NOS. Breslow T1 | 14 (8.2%) | 8 (1.5%) | 5.64 (2.34-13.7) | 3.82 | 0.0001 |
| Melanoma NOS. Breslow T2 | 2 (1.1%) | 2 (0.39%) | 3.02 (0.42-21.6) | 1.34 | 0.24 |
| Melanoma NOS. Breslow T3 | 1 (0.5%) | 5 (0.9%) | 0.59 (0.06-5.16) | 0.22 | 0.64 |
| Melanoma NOS. Breslow T4 | 3 (1.7%) | 7 (1.3%) | 1.29 (0.33-5.05) | 0.13 | 0.71 |
| Total | 170 | 511 | |||
*NOS - Not otherwise specified
According to the values given in table 2, it can be inferred that, for multicentric BCC, the chance of acquisition is 671% greater for women than for men. For superficial BCC, the chance of acquisition is estimated to be 187% greater for women than for men. For SCC associated with Bowen’s disease, the chance of acquisition is estimated to be 315% greater for women than men. For undifferentiated SCC, women are 50% less likely than men to acquire the disease; and for T1 melanoma, the risk for females is 464% greater.
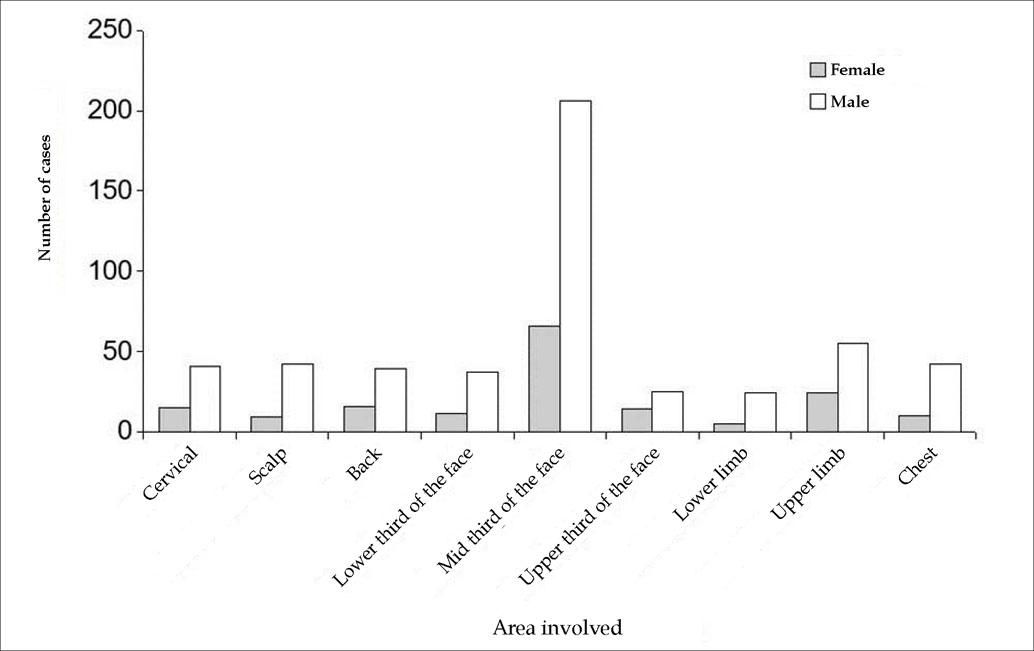
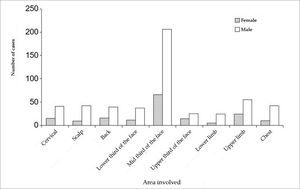
The frequency of carcinomas, per gender, diagnosed relative to their anatomical localization in the patients, is presented in graphic 2. There was a predominance of BCC in the cephalic region, principally on the middle third of the face.
According to graphic 2, the sex factor had no influence on the site of cancer occurrence, since both genders presented a similar incidence for the occurrence.
The most frequent histological type, according to the classification proposed by the Brazilian Society of Pathology,22 was basal cell carcinoma, with 480 cases — corresponding to 70.32% of the total — followed by spinocellular carcinoma (23.53%) and, finally, by melanoma (6.14%).
The most frequent histological subtype among the basal cell carcinomas, again according to the classification proposed by the Brazilian Society of Pathology, was nodular (51.25%) with or without ulceration, followed by undifferentiated (16.67%, sclerosing (12.70%), superficial (7.5%), adenoid cystic (7.08%), micronodular (3.33%) and, lastly, multicentric (1.54%); however, it should be noted that 16.67% were not classified.22
The spinocellular carcinoma histological type was also subdivided, forming three histological subtypes that vary according to the degree of differentiation. They are, from highest to lowest incidence, as follows: undifferentiated (84.27%); associated with Bowen’s disease (8.08%); and verrucous (6.91%).
Using globally recognized classification criteria, the Breslow index confers the most meaningful values in the prediction of disease progression, as it describes the thickness of the melanoma (measured in millimeters) and the presence or absence of ulceration (determined histopathologically).23,24 The thinner the melanoma, the greater the chance of curing it. On that basis, a standardization for melanomas was established according to the Breslow index, with the following findings: melanoma Breslow T1 (52.38%), followed by Breslow T4 (23.80%), Breslow T3 (14.28%) and, lastly, melanoma with Breslow T2 subtype (9.52%).
In relation to the year of diagnosis, 55 cases were reported in 2011; 79 cases in the following year; and 91 cases in 2013. In 2014, there were 118 cases; in 2015, there was an increase of 53 cases, reaching 171 by the end of the year; and in the final year of analysis, 2016, 167 cases were recorded.
DiscussionWe analyzed 681 reports of anatomopathological diagnoses of malignant skin neoplasms in rural-worker patients treated at the Cascavel Oncology Center (CEONC), in the municipality of Cascavel (PR), between 2011 and 2016. Cascavel is a regional pole and a reference center for 52 cities in the west region of Paraná; the sample is, therefore, representative of the study region. The total number of cases diagnosed per year has increased in the number of skin cancers over a five-year period, with 55 cases in the first year of the study (2011) and 167 cases in the last year (2016).
This increase can be explained by the increment in the number of diagnoses made in the municipality, due to the greater knowledge and awareness that doctors and patients have about the lesion; by the intensification of solar radiation; and by rural workers’ habit being exposed to the sun without protection.25
An additional, associated factor is the increase in ultraviolet radiation resulting from the depletion of the ozone layer. It is predicted that, for every 10% reduction in the ozone layer, there is an increase of 40% in the incidence of skin cancer.26 Furthermore, a majority of the population of Paraná has light skin, owing to European colonization, and is therefore more susceptible to damage caused by ultraviolet radiation. This point emphasizes the fact that skin cancer, whether melanoma or non-melanoma, is the most common malignancy in Caucasians.27,28
Overall, 681 cases were analyzed, with only 170 (24.96%) of them occurring in women, a finding consistent with similar studies that confirm the lower participation of women in professions that involve a high level of sun exposure.29
The gender differential in the incidence of neoplasms was found only for the following types of cancer: multicentric BCC (p=0.01), superficial BCC (p=0.002), SCC associated with Bowen’s disease (p=0.004), undifferentiated SCC (p=0.005), and T1 melanoma (p=0.0001). However, for the other types of cancer, the sex was not a risk factor. It should be noted that the chance of acquisition among women was greater for multicentric BCC, SCC associated with Bowen’s disease, and T1 melanoma.
The general analysis of skin cancer types found that the incidence of BCC was similar between sexes; in contrast, SCC affected a greater number of men, and melanoma had a considerably higher incidence in women. These data refute the studies that evaluate the general population without specifying rural workers, in which the worldwide incidence of basal cell carcinoma and spinocellular carcinoma was, respectively, 1.5 times higher and 1.9 times higher in men than in women.30
In rural workers, however, the higher incidence of melanoma in women leads us to infer that their sun exposure is more intermittent and in high doses, a possible conclusion being that they assist during harvest periods. For the non-melanoma type, particularly SCC, the incidence increases with age and is higher in men than women, confirming that cumulative and continuous sun exposure favors its development.
Although the analysis showed that skin cancer affected significantly more men than women, across all evaluated age groups, the sex factor had no influence on the cancer’s site of occurrence.
In terms of age, the largest proportion of cases were found for the 61-70 age group. However, to evaluate the influence of age on the site affected by cancer, three age categories were created: category 1, for patients up to 55 years old; category 2, comprising patients from 56 to 65 years of age; and category 3, for patients 66 years and older. In the general analysis of these categories, the one with the highest concentration of cancers was category 3 – 66 years and older – with 320 cases. This datum may be explained by the fact that rural workers spend more time exposed to risk factors for cancer development, particularly the cumulative effect of intense and intermittent sun exposure.31
Most skin carcinomas arise in areas of the body subject to frequent sun exposure.32 In this work, 60% of all cancers were in the cephalic segment, the middle third of the face being the site of the largest proportion (39.9%) of cancers, corroborating other studies that evaluated the basal cell subtype exclusively.33
This finding reinforces the importance of chronic sun exposure as a risk factor – the face being a site frequently exposed to the sun – especially considering that many outdoor workers do not use any type of sunscreen.34,35 It is noteworthy that Regulatory Norm (RN) 31 advocates the provision of personal protection equipment (PPE) for rural workers exposed to the sun, such as a wide-brimmed hat or a flap cap, non-ionizing radiation protection glasses, and full-body protection for jobs that carry a risk of heat-related injury.36 However, there is no legislation that mandates the use of sunscreen. Its use ought to be indicated for specific areas of the skin for which PPE cannot provide the desired protection.
In terms of histological type, the most frequent was nodular basal cell carcinoma, with or without ulceration (36.12%), its prevalence being in accordance with the findings of other studies; however, no other studies compared its prevalence with all carcinoma subtypes.32,37
The incidence of this type of neoplasm can be explained by an occupational exposure that occurs intermittently, which is important in the development of basal cell carcinoma and melanoma. For SCC, however, continuous exposure is more relevant. Cumulative and excessive exposure during the first 10-20 years of life is considered to increase the risk of skin cancer.38
Among the limitations of this study, the foremost is its design, since causality cannot be established in cross-sectional studies, and some variables (skin phototype, frequency of sun exposure, use of physical and chemical protection, among other aspects) were impossible to assess because the data were obtained from a secondary data bank. Furthermore, some of the reports lacked data, compromising the analysis of the results and possibly leading to some information bias.
Regarding the observed data, it should be emphasized that skin cancer is an occupation- and environment-based disease, which requires prevention. Its global epidemiology demonstrates that, compared to indoor workers, outdoor workers are at significant risk of developing skin cancer.39,40 From another perspective, more population studies are needed to assess the real magnitude of the problem and its repercussions on public heath, particularly in the group studied.
This study revealed the reality of this neoplasm’s behavior in the rural workers treated in Cascavel, western Paraná. Through this study, it was possible to identify a high-risk group and its behavioral elements. This information supports sanitary measures for primary protection among the general population — such as detection campaigns, the promotion of educational programs in schools and communities, and the optimization of public health and workers’ health actions, thereby reducing morbidity and healthcare system expenditures through recognition and early treatment of lesions37 — and it promotes the reduction of skin cancer incidence in future generations.
ConclusionThe study of 681 anatomopathological exam reports of rural workers diagnosed with skin cancer at the Cascavel Oncological Center (CEONC), between 2011 and 2016, leads us to conclude that the incidence of the disease has increased significantly, being most prevalent in men and affecting people older than 65 in particular. The site most affected was the cephalic region, and the most common histological subtype was nodular basal cell carcinoma, followed by undifferentiated squamous cell carcinoma. This study is a regional estimate of the incidence of cutaneous neoplasms and provides evidence of a considerable increase in the number of skin cancer diagnoses in rural-worker patients in Paraná, Brazil. Moreover, it is possible to conclude that the sample group studied seems to be at risk of developing skin cancer. ❑