Dear Editor,
Basal cell carcinomas (BCC) present different subtypes that exhibit diverse prognostic behavior. The main histological subtypes are nodular (including cystic and pigmented), sclerodermiform, superficial, and rare variants: micronodular and fibroepithelioma of Pinkus.1
The evolutionary differences of the different types of BCC are not well defined, nor are the processes that determine their histological differentiation. The three most representative subtypes are nodular, sclerodermiform (infiltrative), and superficial. Although more than 40% of the lesions present mixed components, different characteristics, invasiveness, and recurrences related to the subtypes are observed, suggesting different biological behaviors.1,2
The rate of cell proliferation is associated with the growth and invasiveness of various malignancies. However, the ability to promote apoptosis represents a form of primary cellular resistance to genomic and metabolic alterations linked to malignant neoplastic initiation, promotion, and proliferation.3 Thus, different expression profiles of proteins linked to proliferation and apoptosis, such as p53, ki67, survivin, and NFκB pathway (p105), may characterize the clinical subtypes of BCC and the pattern of recurrent cases relative to the adjacent normal epithelium.
This study aimed to evaluate the expression of cell proliferation and apoptosis markers in the nodular, superficial, and infiltrative (sclerodermiform) types of BCC and recurrent tumors.
We conducted a cross-sectional study involving BCC smaller than 2cm operated between 2012 and 2013 in the HC-Unesp (Botucatu-SP, Brazil), divided into: nodular only (n=18), superficial (n=6), infiltrative (n=6), and surgical recurrences, with three subtypes: superficial (n=7), nodular (n=11), and infiltrative (n=4). The research project was approved by the local research ethics committee.
The specimens’ histological slides were submitted to immunohistochemical (DAB) labeling for ki67, p53, survivin, and p105 according to manufacturers’ protocols. Micrographs of three hotspot areas of the tumor blocks and adjacent epithelium were sampled to calculate the percentage of immunolabelled cells or relative intensity of p105 cytoplasmic labeling, calculated by digital imaging analysis.
The results of the tumor subtypes, adjacent epithelium, and the recurrent cases were compared by multivariate models: generalized linear mixed effects model and multiple correspondence analysis. Significance was set at p<0.05.
The sample of 50 individuals consisted of 25 (50%) females, with mean age 64.4±14.2 years and lesion diameter 0.73±0.47cm.
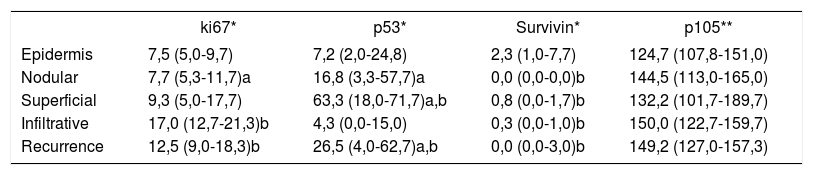
Table 1 shows the percentages of immunolabelled cells or the relative intensity of the cytoplasmic labeling of each marker, highlighting differences between ki67, survivin, and p53 among the different histological subtypes, especially the infiltrative type and the epidermis adjacent to the lesions. The p105 marker showed no differential behavior for any group.
Comparison of the median (p25-p75) percentages of immunolabeled nuclei (ki67, p53, and survivin) or relative cytoplasmic labeling intensity (p105) in histological subtypes of basal cell carcinomas and adjacent epidermis
| ki67* | p53* | Survivin* | p105** | |
|---|---|---|---|---|
| Epidermis | 7,5 (5,0-9,7) | 7,2 (2,0-24,8) | 2,3 (1,0-7,7) | 124,7 (107,8-151,0) |
| Nodular | 7,7 (5,3-11,7)a | 16,8 (3,3-57,7)a | 0,0 (0,0-0,0)b | 144,5 (113,0-165,0) |
| Superficial | 9,3 (5,0-17,7) | 63,3 (18,0-71,7)a,b | 0,8 (0,0-1,7)b | 132,2 (101,7-189,7) |
| Infiltrative | 17,0 (12,7-21,3)b | 4,3 (0,0-15,0) | 0,3 (0,0-1,0)b | 150,0 (122,7-159,7) |
| Recurrence | 12,5 (9,0-18,3)b | 26,5 (4,0-62,7)a,b | 0,0 (0,0-3,0)b | 149,2 (127,0-157,3) |
p <0.05 compared to infiltrative; b p <0.05 relative to the epidermis
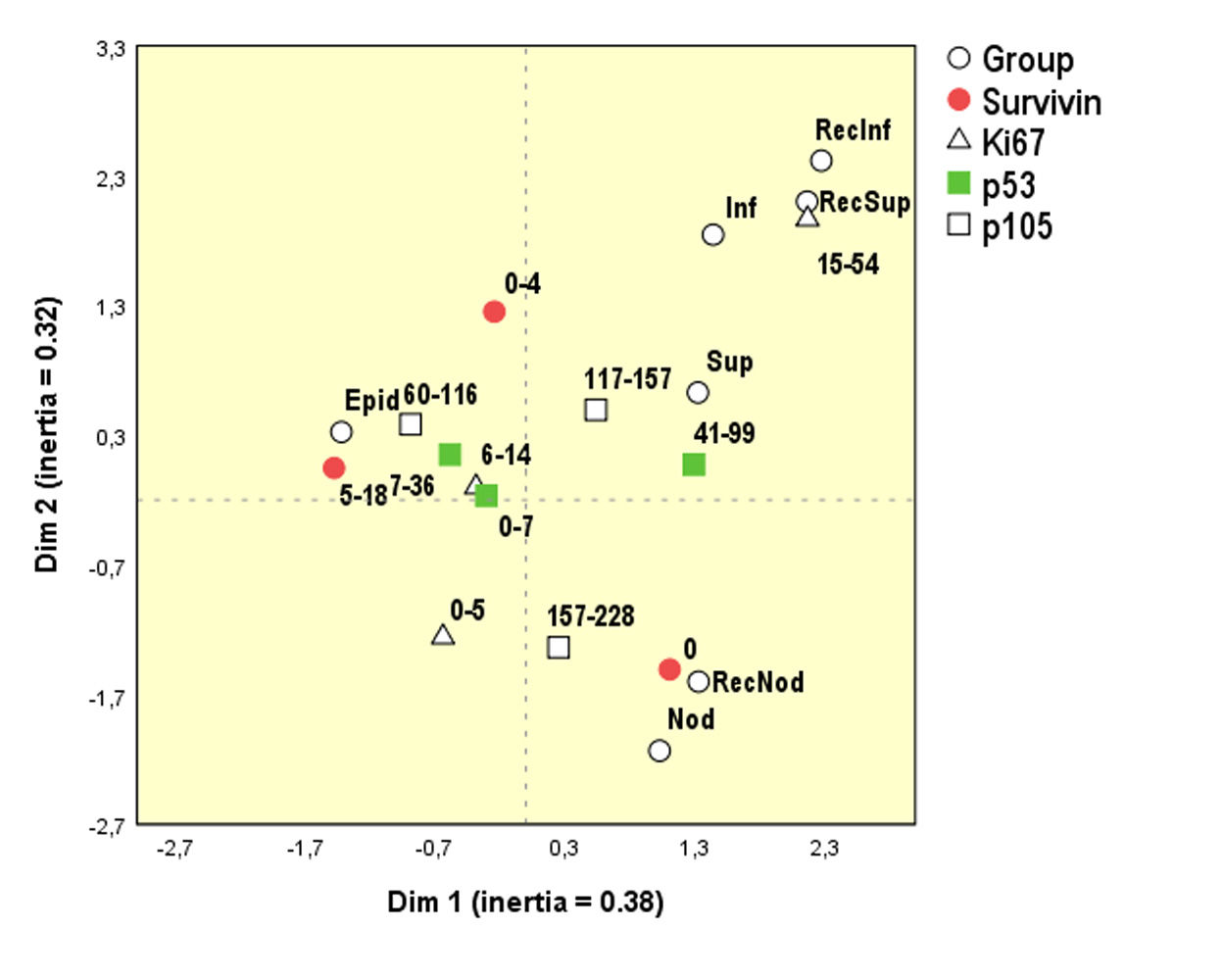
Multivariate analysis (Figure 1) identified an individualized pattern for the different subtypes. Nodular forms were associated with higher p105 and lower values of survivin. The epidermis showed higher survivin and intermediate ki67 values. Recurrent BCC subtypes maintained the same expression patterns of proliferation and apoptosis markers as the other histological subtypes of primary BCC.
Perceptual map of Multiple Correspondence Analysis. Black circles represent the cell types studied, and the other symbols represent the response intensity of each marker (Epid = epidermis, RecNod, RecInf, and RecSup = recurrence with nodular, infiltrative, or superficial histology)
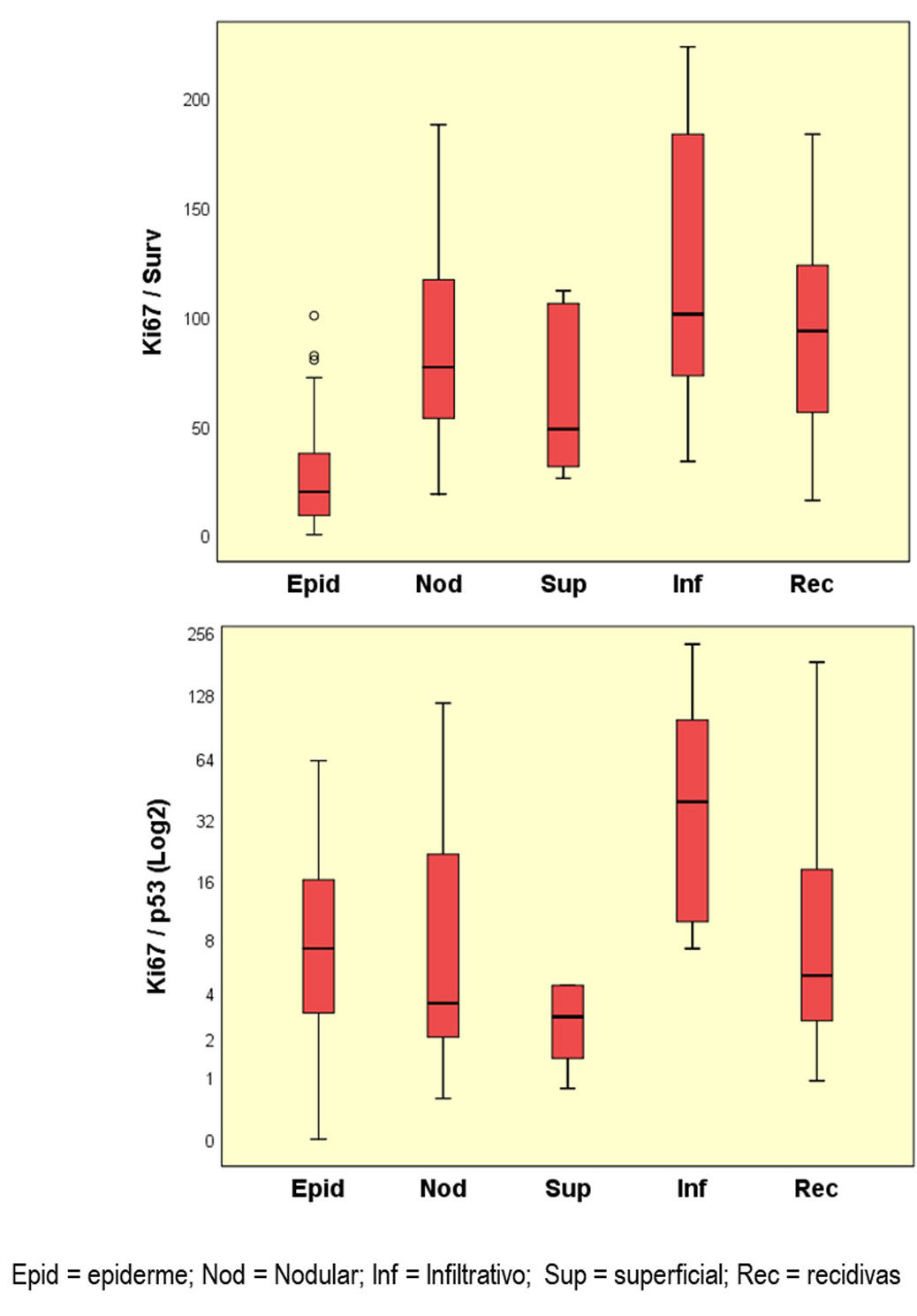
All BCC subgroups showed higher ki67-to-survivin ratio (Figure 2) than the epidermis (p<0.05). The ki67/p53 ratio differed between the infiltrative and superficial subtypes (p<0.05). The other ratios between markers did not present striking results (data not shown).
The current study explored patterns of proliferation and apoptosis in different BCC subgroups, compared to relapses and adjacent epithelium.
Ki67 is the principal marker of cell proliferation and serves as a prognostic index for various neoplasms, as well as cancerization field activity. The p53 protein is associated with apoptotic activity, resistance to proliferation, and invasion. Survivin, on the other hand, is expressed in several neoplasms, evidencing resistance to apoptosis.3
Neoplasms differed from the adjacent epithelium due to higher ki67 and lower survivin expression, suggesting that the latter may play a key role in resistance to apoptosis in the skin cancerization field. Unlike squamous cell carcinomas and actinic keratoses, the basal cell carcinomas express little survivin, indicating that they use another mechanism of resistance to apoptosis, such as interference in the p53 and Bcl2 pathways.4
The p53 protein appears to significantly influence the containment of invasive neoplasms. The higher ki67/p53 ratio in infiltrative versus superficial BCC may provide the basis for the invasive growth versus radial expansion characterizing these subgroups.5
There is some question as to modification of the biological behavior in BCC recurrence, but in this study the labelling patterns of the underlying histological subtypes were maintained. The highest relapse rate occurred in the infiltrative subtypes.
In conclusion, BCC subtypes and adjacent epithelium presented different patterns of proliferation and apoptosis expression. Recurrent tumors expressed the same patterns as the primary BCC subtypes.
Financial Support: FUNADERSP – 2016.
Conflict of interest: None.