Dear Editor,
PEComas are rare mesenchymal tumors, consisting of distinct epithelioid cells from the histological and immunohistochemical point of view, with clear or granular cytoplasm, tending to organize in perivascular form, expressing both melanocytic cell markers and myogenic markers.1 They display cell similarity with angiomyolipoma, “sugar cell” tumors, and lymphangioleiomyomatosis.1 PEComas have been identified at various anatomical sites, but only 8% of cases have cutaneous or subcutaneous manifestations.2 Armah et al. published a literature review in 2009, when they counted no more than 100 cases published in English,1 the majority in the uterine corpus of middle-aged women. Head and neck PEComas are among the least common. At this topography, cases in the nasal cavity are the most prevalent.1 We found only two previously published cases located on the cheek.2,3 The first was a deep lesion, traversing the buccinator muscle and resected by transoral access.3 The second case was similar to ours, manifesting as a cystic skin lesion on the cheek of a 44-year-old male, with cytologic criteria indicative of malignancy, with no signs of metastases after two years of follow-up.2
These tumors tend to display benign behavior, but the spectrum of clinical manifestations varies. Malignant cases tend to present with two or more of the following: tumor size >5cm, infiltrative growth pattern, hypercellularity, exuberant and hyperchromic nuclei, zones of necrosis, high mitotic activity (>1/50), vascular invasion, and atypical mitoses.4 Late metastases to the lungs, liver, intestines, bones, and lymph nodes have been described, confirming the tumor’s malignant behavior.1
Differential diagnosis includes melanoma, clear cell carcinoma and sarcoma, myoepithelioma, paraganglioma, and alveolar sarcoma.1 The cells are immunoreactive to smooth muscle and melanocytic markers.1 HMB45 is considered the most sensitive marker for PEComa, followed by Melan-A.5 Smooth muscle actin (SMA) is the most widely described smooth muscle marker.1 Meanwhile the desmin marker is more prevalent in cutaneous cases as compared to visceral cases.1,5
Due to the lesion’s rarity and the scarcity of available information, there is still no consensus on the ideal treatment for PEComa. Surgery remains the most widely recommended treatment for the primary tumor, metastases, or local recurrence. The role of adjuvant therapy remains uncertain, but treatment strategies with adjuvant chemotherapy and/or radiotherapy have been reported.1
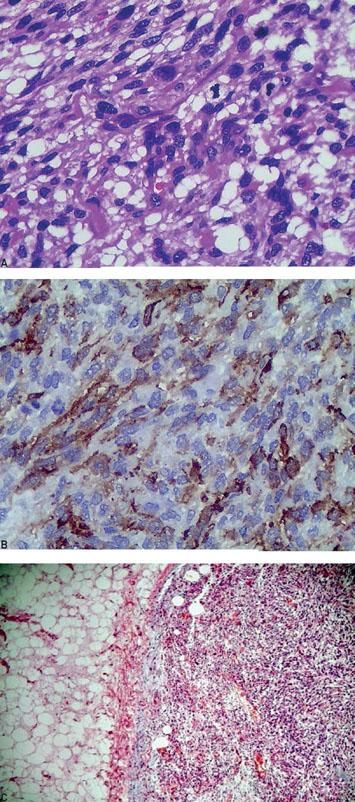
We describe the case of a 69-year-old male presenting a lesion with two months’ evolution on the left cheek. The patient had already undergone surgery at another service when the lesion first appeared, with initial suspicion of infected sebaceous cyst. Anatomical pathology was suggestive of sarcomatous mesenchymal neoplasm, with positive margins and fragmentation of the specimen. The patient presented at our service with a nodular, fibroelastic lesion measuring 3-4cm, mobile, occupying the superficial soft tissues at the left parotideal region, with no signs of facial paralysis, but with signs of infiltration of the overlying skin (Figure 1). The patient underwent resection with preservation of the facial nerve and reconstruction with a transverse platysma flap (Figure 2). Anatomical pathology revealed a 3cm, dull light-brown homogenous subcutaneous lesion. Under light microscopy, the tumor consisted of a spindle cell pattern with edema and collagen bands, high mitotic index (> 10/10HPF), and atypical nuclei, with no signs of neural or lymphatic invasion (Figure 3A). The resection margins were negative. Immunohistochemistry showed diffuse immune reactivity to SMA (Figure 3B) and focal reactivity to CD68 and HMB45 and negativity to AE1/AE2, CD34, desmin, EMA, factor XIIIa, melan-A, and S-100 protein. The diagnosis of grade II PEComa was confirmed. Adjuvant radiotherapy was preformed in the surgical bed (66Gy/30 fractions). In three months of post-radiotherapy follow-up, the patient presented signs suggesting relapse in the ipsilateral level V cervical lymph node and underwent a salvage neck dissection, without confirmation of malignancy. Since then, he has remained free of signs of active disease but is still in the first 16 months of post-treatment follow-up. The case should alert surgeons, dermatologists, and pathologists to this differential diagnosis.
Financial support: None.
Conflict of interest: None.