Dear Editor,
Psoriasis is one of the most common inflammatory dermatoses and, in most patients, presents with erythematous scaling plaques on extensor areas. Classically, several clinical subtypes are described, such as plaque, inverted, guttate, palmoplantar, erythrodermic, and pustular. A minor variant discussed and reported is follicular psoriasis (FP), with only 25 reports in the international literature to date. Thus, the present article describes the first Brazilian case and revises concepts of this little known entity.
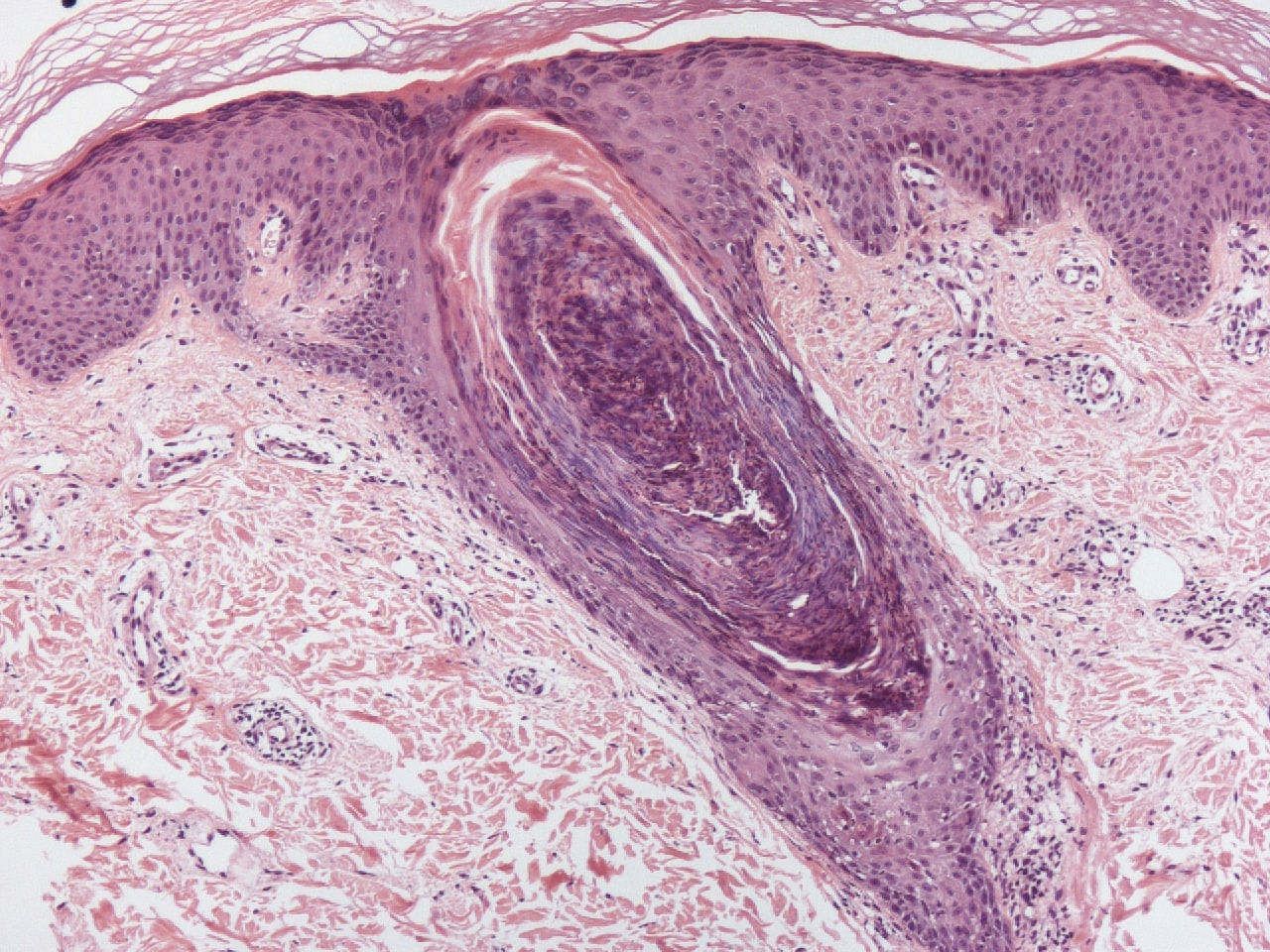
A 58-year-old female diabetic type 2 patient presented with erythematous, keratotic, exclusively follicular non-pruritic papules measuring 2-3mm in diameter. The lesions were generalized, but with higher density in the gluteal and proximal regions of the thighs (Figures 1 and 2). Still, few isolated follicular pustules could be seen. Palms of the hands and soles of the feet were unchanged. The lesions appeared 4 years ago in the lower limbs with later gradual spread. Diagnostic hypotheses were pityriasis rubra pilaris (PRP) and keratosis pilaris with secondary infection. Previous histopathological examination of biopsy specimens revealed a diagnosis of follicular porokeratosis. Histopathological review showed parakeratosis and numerous intact and degenerate neutrophils within the lumens and in the epithelium of the follicular isthmus, where they formed a spongiform pustule. In addition, mild regular perifollicular acanthosis was also present (Figure 3). Grocott’s staining revealed no fungal elements. We decided to use cephalexin for 10 days as a therapeutic test for primary bacterial folliculitis or impetiginization with no success. A second biopsy was also performed with similar results to the first. Confronting clinical and histopathological findings, we concluded by the diagnosis of follicular psoriasis. We started treatment with acitretin with improvement after 2 months.
Although FP was first described in 1920 by McLeod, only 25 cases were reported in the literature.1; The largest series of cases, published in 1981 by Stankler and Ewen, served as the basis for the division into adult and child types.2 The former has a predilection for black and diabetic women, with follicular papules concentrated mainly on the thighs, while the latter presents itself with follicular keratotic papules located on bony prominences or with disseminated lesions simulating PRP. More recently, Cuong et al. surveyed the published cases and found that 78% of the patients reported were black, corroborating the classic description.3 FP follows a chronic course with some authors suggesting that it may be an early stage of psoriasis since it may evolve into other forms of the disease.4 The clinical picture of our patient fulfills the criteria of adult-type follicular psoriasis since, besides her high pigmentation level and diabetes, the most affected areas were the thighs.
The predominant histopathological findings are parakeratosis with neutrophils, as well as acanthosis of the infundibular epithelium with hypogranulosis. Both clinically and mainly histopathologically, infected follicular keratosis is an important differential diagnosis. However, onset age of 54 years makes this possibility unlikely. In addition, regarding the histopathology of FP, Arps et al. (2013) suggest that minimal spongiosis, little serosity in the parakeratotic scale, and sparse perifollicular inflammation, as seen in our patient, differentiate FP from bacterial folliculitis.5 A clinical alternative to differentiate FP from bacterial folliculitis is the therapeutic test with antibiotics. In cases of FP, as in our patient, no improvement is observed.
We believe that psoriasis – like other dermatoses, such as lichen planus, follicular porokeratosis, and atopic dermatitis – also has a follicular variant. It is likely that follicular involvement in psoriasis is neglected, especially in countries such as Brazil, where a large part of the population is of African descent.
Financial support: None.
Conflict of interest: None.